Tourette Syndrome and other tics disorders affect millions of people worldwide, often presenting significant challenges in daily life. While traditional treatments for Tourette’s focus on managing symptoms with medication or behavioral therapy, a growing body of research highlights the potential of neurofeedback for Tourette Syndrome as a non-invasive and effective alternative. This innovative approach targets the neurological roots of the condition, offering hope for long-term improvement in tic disorder treatment. In this article, we’ll explore how neurofeedback works, its benefits, and why it’s emerging as a promising treatment for Tourette’s.
Table of Contents
ToggleClassification and Types of Tic Disorders
Tic disorders can usually be classified as motor, vocal, or Tourette’s syndrome, which is a combination of both. Motor and vocal tics can be short-lived (transient) or chronic. Tourette’s is considered to be a chronic tic disorder.
Children with transient tic disorder will present with one or more tics for at least 1 month but for less than 12 consecutive months. The onset of the tics must have been before the individual turned 18. Motor tics are more commonly seen in cases of transient tic disorder than vocal tics. Tics may vary in type and severity over time. According to the American Academy of Child and Adolescent Psychiatry, a transient tic disorder, or provisional tic disorder, affects up to 10% of children during their early school years.
Tic disorders that appear before age 18 and last for 1 year or more may be classified as chronic tic disorders. These tics can be either motor or vocal, but not both. Chronic tic disorders are less common than transient tic disorders, with less than 1% of children affected.
If the child is younger at the onset of a chronic motor or vocal tics disorder, they have a greater chance of recovery, with tics usually disappearing within 6 years. People who continue to experience symptoms beyond age 18 are less likely to see their symptoms resolved.
Some research suggests that tics disorder are more common among children with learning disabilities and are seen more in special education classrooms. Children within the autism spectrum are also more likely to have tics.
Tourette’s Syndrome: Characteristics and Prevalence
Tourette’s syndrome (TS) is the most severe and least common tics disorder. The Centers for Disease Control and Prevention (CDC) reports that the exact number of people with TS is unknown. CDC research suggests that half of all children with the condition are not diagnosed. Currently, 0.3% of children aged 6 to 17 in the US have been diagnosed with TS. Symptoms of TS vary in their severity over time. For many people, symptoms improve with age. TS is often accompanied by other conditions, such as attention deficit hyperactivity disorder (ADHD) and obsessive-compulsive disorder (OCD).
The onset of Tourette syndrome is usually in childhood between the ages of 2 and 21 years. The disorder affects more males than females, with a ratio of approximately three males to 1 female. Tourette’s is a highly individualistic disorder with differing levels of severity, frequency, and impairment.
Neurodevelopmental Insights into Tourette’s Syndrome
Tourette Syndrome is a neurodevelopmental disorder characterized by persistent, chronic, and involuntary tics. These tics manifest as either motor (motor movements) or phonic (vocalizations) and can range from simple tics, such as blinking, sniffing, and head twitching, to more complex tics, such as repetitive swearing, spinning, and jumping. The cause of Tourette’s is unknown, but both hereditary and nongenetic factors likely contribute to its development.
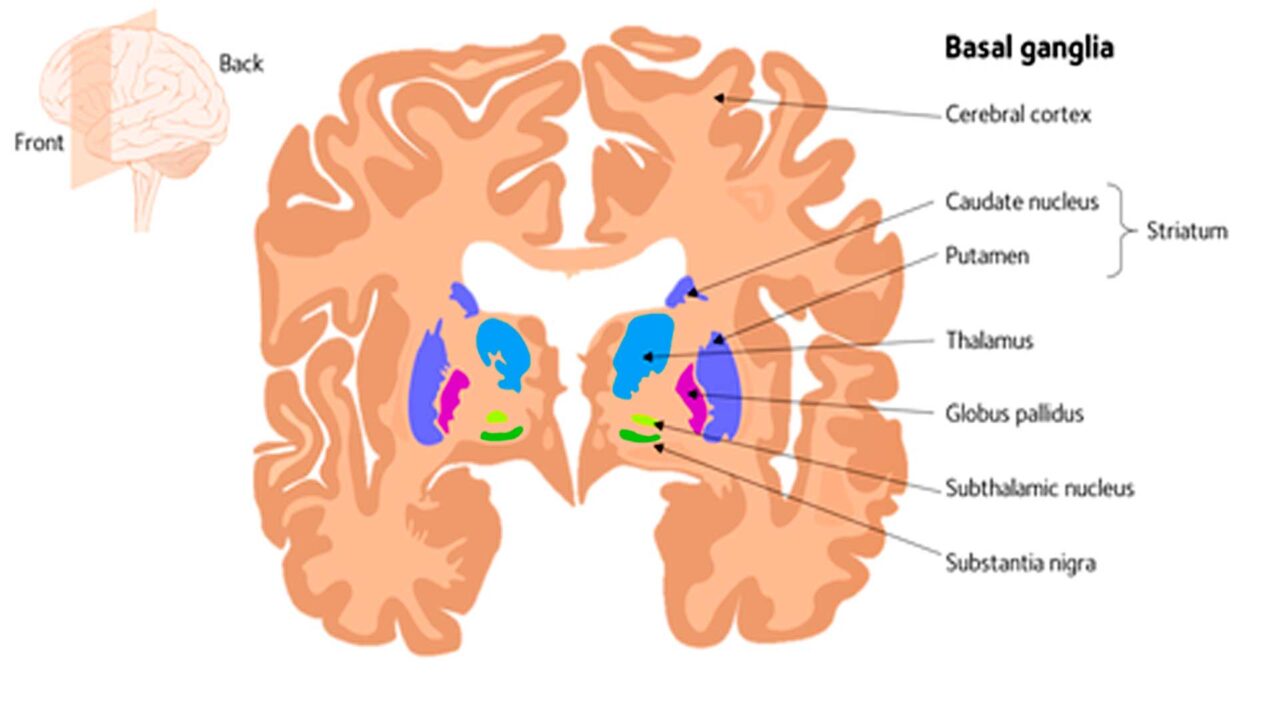
While the exact cause of Tourette Syndrome is unknown, it is believed that the presence of tics is associated with abnormalities in the brain. In particular, it is suggested that there is a distribution in the circuits linking the basal ganglia (the site that controls voluntary motor movements, eye movements, and emotion) to the frontal cortex.
Individuals with Tourette Syndrome exhibit impaired performance on cognitive tasks involving memory, attention, reading, and writing. These impairments are often more severe in individuals diagnosed with comorbid ADHD, who also display less cognitive flexibility. It is estimated that 70% of patients with Tourette Syndrome exhibit ADHD-type behaviors, and as such, Tourette Syndrome can be a debilitating diagnosis for many people.
Having tics doesn’t mean someone has Tourette’s syndrome. Tics have to be present for at least one year to be classified as Tourette’s syndrome, and at least one of the tics has to be vocal.
Symptoms of Tic Disorder
The defining symptom of tic disorders is the presence of one or more tics. These tics can be classified as:
- Motor tics: These include tics, such as head and shoulder movements, jerking of the head, twisting the neck, rolling the eyes, blinking, jerking, banging, clicking fingers, or touching things or other people. Motor tics appear before vocal tics, although this is not always true.
- Vocal tics are sounds such as coughing, blowing, throat clearing, grunting, or repeating words or phrases.
Tics can also be divided into the following categories:
- Simple tics are sudden and fleeting tics that use a few muscle groups. Examples include nose twitching, eye darting, or throat clearing.
- Complex tics: These involve coordinated movements using several muscle groups. Examples include hopping or stepping in a certain way, gesturing, or repeating words or phrases.
An uncomfortable urge, such as an itch or tingle, usually precedes tics. While holding back from performing the tic is possible, this requires much effort and often causes tension and stress. Relief from these sensations is experienced upon performing the tic.
The symptoms of tic disorders may:
- worsen with emotions, such as anxiety, excitement, anger, and fatigue,
- worsen during periods of illness,
- worsen with extreme temperatures,
- occur during sleep,
- vary over time,
- vary in type and severity,
- improve over time.
Causes and risk factors for Tourette’s syndrome and Tic Disorders
The exact cause of tic disorders is unknown. However, recent studies in Tourette’s research have identified specific gene mutations that may play a role. Brain chemistry, especially the brain chemicals glutamate, serotonin, and dopamine, also seems essential.
Tics with a direct cause fall into a different diagnostic category. These include tics due to:
- head injuries,
- stroke,
- infections,
- poisons,
- surgery,
- other injuries.
In addition, tics can be associated with more serious medical disorders, such as Huntington’s disease or Creutzfeldt-Jakob disease.
Risk factors for tic disorders include:
- Genetics: Tics tend to run in families, so there may be a genetic basis for these disorders.
- Sex: Men are more likely to be affected by tic disorders than women.
Conditions associated with tic disorders
Conditions associated with tic disorders, especially in children with TS, include:
- anxiety
- ADHD
- depression
- autistic spectrum disorder
- learning difficulties
- OCD
- speech and language difficulties
- sleep difficulties
Other conditions associated with tic disorders are those related to the effects of tics on self-esteem and self-image. Some research has found that children with TS or any chronic tic disorder experience a lower quality of life and lower self-esteem than those without one of these conditions.
In addition, the Tourette Association of America says that people with TS often experience difficulties with social functioning due to their tics and associated conditions, such as ADHD or anxiety.

Brain changes in Tourette’s Syndrome and Tic Disorders
Neurobiological Features of Tourette’s Syndrome and ADHD
The frequent comorbidity of TS and ADHD may reflect a common underlying neurobiological substrate, and studies confirm the hypothesized involvement of frontostriatal circuits in both TS and ADHD. However, poor inhibitory control and volumetric reductions in frontostriatal circuits appear to be core features of ADHD. In contrast, reduced volumes of the caudate nucleus and activation and hypertrophy of prefrontal regions that likely help suppress tics seem to be core features of TS. (Neuroimaging of tic disorders with co-existing attention-deficit/hyperactivity disorder – Kerstin J. Plessen, M.D., Jason M. Royal, D.M.A., and Bradley S. Peterson, M.D.)
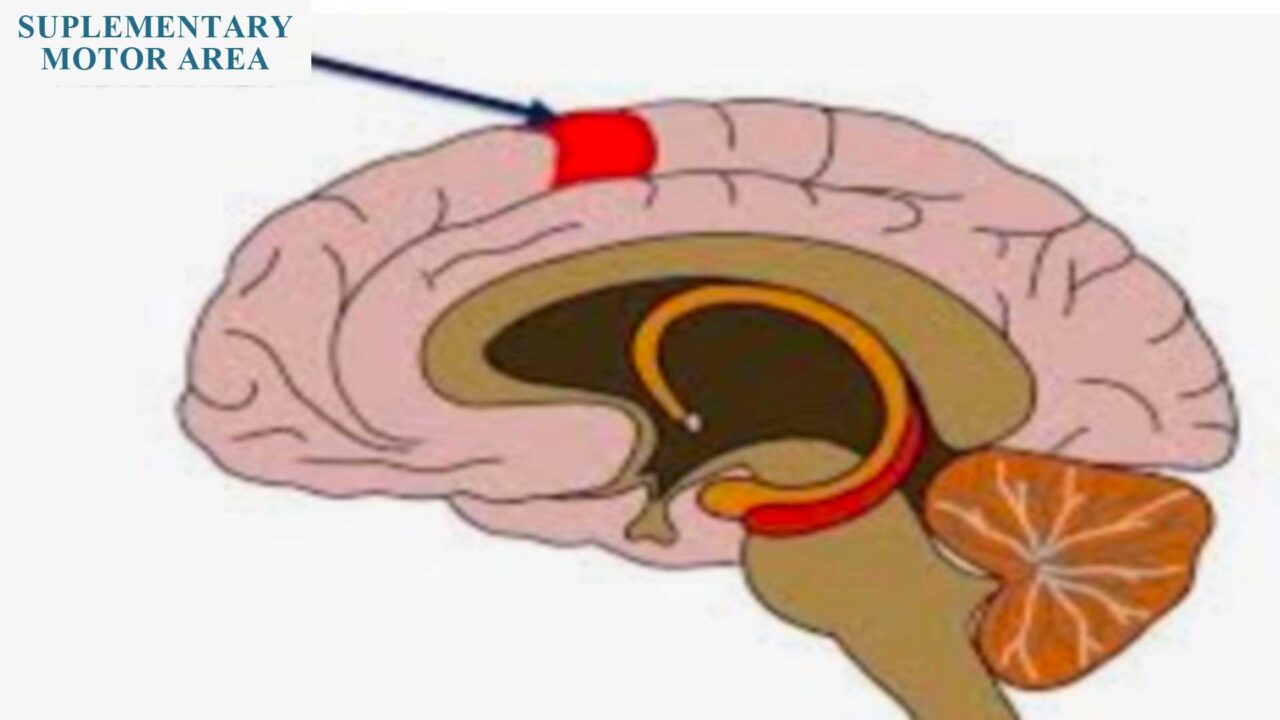
Activity in the brain’s supplementary motor area (SMA) has been associated with tics. The investigators placed tic patients in the MRI scanner and conducted a real-time functional magnetic resonance imaging neurofeedback session. The patients could see the SMA light up and try to control that area by focusing their thoughts on it. The patients who received the real neurofeedback had a greater reduction in tics on the Yale Global Tic Severity Scale than those in the sham control group.
Brain Imaging Insights into Tourette’s Syndrome
Researchers at Washington University School of Medicine in St. Louis have identified areas in the brains of children with Tourette’s syndrome that appear markedly different from those in the brains of children without the disorder.
In kids with Tourette’s, the researchers also found less white matter around the orbital prefrontal cortex, just above the eyes, and in the medial prefrontal cortex, also near the front, than in kids without the condition.
White matter acts like the brain’s wiring. Unlike the axons in gray matter, axons in white matter are coated with myelin and transmit signals to gray matter. Less white matter could mean less efficient transmission of sensations, whereas extra gray matter could mean nerve cells send extra signals.
In a scan of a child with Tourette’s, yellow indicates an area with less white matter than in the same brain region in kids who don’t have the disorder. The scans also revealed that the brains of kids with Tourette’s have more gray matter (the posterior thalamus, hypothalamus, and midbrain) than those of children without the condition.
Neurofeedback for Managing Tics and Executive Function Deficits
Deficits in executive functioning, which contribute to ADHD symptoms, also appear in TS, with the same losses of structural integrity in the cortico-striatal and cortico-thalamic pathways common to both disorders. Neurophysiological processes underlying these deficits in executive functioning can be modulated with neurofeedback.
Clinical researchers Chuanjun Zhuo and Li Li (2014) found that neurofeedback training improved motor and vocal tic symptoms (e.g., reduced tic frequency and intensity) in adolescents with refractory Tourette syndrome.
Simone Messerotti Benvenuti et al. (2011) used an SMR up-training/Theta down-training schedule for 16 sessions, followed by six more sessions of purely SMR up-training. SMR increase was better obtained when SMR up-training was administered alone, whereas Theta decrease was observed after both types of training.
After 40 SMR training sessions, 75% of patients demonstrated increased SMR production and a positive change in the theta/beta ratio.
Researchers hypothesized that training the sensorimotor cortex would increase voluntary muscle control and eliminate tics.
Neurofeedback for Tourette syndrome and Tic Disorders
Neurofeedback training is a self-regulation strategy. The brain is trained at the point where the tics are to reduce or eliminate them. In a brain with TS, there is over-arousal. The motor system is highly excitable. The overarching need is for this brain to experience calming, both generally and specifically regarding motor circuits. When such calming is achieved, the tics (motor and vocal) may be reduced.
Neurofeedback practitioners have seen significant symptom improvement in most cases with the right approach. Nonetheless, every case is different, and sometimes you may not experience a reduction in tics, but overall, you should feel more relaxed and notice better sleep quality. This condition appears to benefit from long-term training.
Presently, medications used to treat tics can cause unforeseen side effects, whereas neurofeedback therapy can be tailored to more accurately target the area of the brain that needs changing.
By Dr. Clare Albright – “Neurofeedback – Transforming Your Life With Brain Biofeedback” – www.neurofeedbackbook.com
Neurofeedback for Tourette Syndrome - Protocols
1. Sensor Placement:
Neurofeedback for Tourette syndrome typically involves applying electrodes to specific sites on the scalp according to the 10-20 system, a standardized method for locating and measuring EEG electrode placements.
Common electrode sites include Cz (vertex), Fz (midline frontal), C3/C4 (left and right central), and Pz (midline parietal).
2. Frequency Bands:
Neurofeedback protocols often target specific frequency bands associated with neurological functioning. For TS, protocols may focus on training specific frequencies like the sensorimotor rhythm (SMR) and beta waves. SMR is associated with motor control and inhibition and is often implicated in TS symptomatology.
3. Operant Conditioning:
The neurofeedback for Tourette Syndrome involves operant conditioning, where individuals learn to regulate their brain activity in response to visual or auditory feedback. In the case of TS, patients might receive positive feedback when their brain activity corresponds to a desired state (e.g., reduced hyperactivity in specific brain regions).
Electrode Application Sites According to 10-20 System
1. Cz (Vertex): Often associated with overall brain regulation.
Relevance: The central region of the motor cortex is crucial for motor control, which is often dysregulated in TS.
2. Fz (Midline Frontal): May target prefrontal areas associated with impulse control.
• Relevance: Associated with executive function and impulse control, which are often impaired in individuals with TS.
3. C3/C4 (Left and Right Central): Relevant for sensorimotor rhythm and motor control.
C3 – Relevance: Involved in motor control and coordination, targeting this area can help reduce motor tics.
C4 – Relevance: Also involved in motor control; targeting this area can help balance neural activity related to motor functions.
4. Pz (Midline Parietal): Associated with sensory processing and integration.
Neurofeedback Protocols for Tourette Syndrome
The protocol involves training individuals to increase or decrease specific brainwave activity at the targeted locations to improve motor control and reduce tics.
Sensorimotor Rhythm (SMR) Training
This protocol focuses on increasing SMR (12-15 Hz) activity to promote calm and reduce motor tics.
- Target Brainwaves: SMR (12-15 Hz)
- Goal: Increase SMR activity to enhance motor inhibition and reduce hyperactivity in the motor cortex.
Procedure:
1. Electrode Placement: Place electrodes at C3 (left sensorimotor cortex), Cz (reference), and C4 (optional for bipolar montage).
2. Baseline Recording: Record baseline SMR activity for 5-10 minutes.
3. Feedback Mechanism: Provide real-time feedback using visual (e.g., a moving bar or animation) or auditory (e.g., tone) cues. Positive feedback is given when SMR activity increases.
4. Training Sessions: Conduct 20-30 minutes of training sessions, 2-3 times per week, for 20-40 sessions.
5. Progress Monitoring: Use tic severity scales and follow-up qEEG to assess changes.
Theta/Beta Ratio Training
This protocol aims to balance theta (4-8 Hz) and beta (15-30 Hz) wave activity to improve attention and impulse control.
- Target Brainwaves: Theta (4-8 Hz) and Beta (15-30 Hz)
- Goal: Decrease theta activity and increase beta activity to improve cognitive control and reduce impulsivity.
Procedure:
1. Electrode Placement: Place electrodes at Fz (frontal midline) and Cz (reference).
2. Baseline Recording: Record baseline theta and beta activity for 5-10 minutes.
3. Feedback Mechanism: Provide feedback using visual or auditory stimuli. Positive feedback occurs when theta decreases and beta increases.
4. Training Sessions: Conduct 20-30 minutes of training sessions, 2-3 times per week, for 20-40 sessions.
5. Progress Monitoring: Utilize attention and impulse control scales and follow-up qEEG to track progress.
Alpha/Theta Training
This protocol focuses on increasing alpha (8-12 Hz) and theta (4-8 Hz) waves to promote relaxation and reduce anxiety, which can exacerbate tics.
- Target Brainwaves: Alpha waves (8-12 Hz) and Theta waves (4-8 Hz)
- Goal: Increase alpha and theta activity to reduce stress and improve emotional regulation.
Procedure:
1. Electrode Placement: Place electrodes at Cz and Fz (reference).
2. Baseline Recording: Record baseline alpha and theta activity for 5-10 minutes.
3. Feedback Mechanism: Use calming visual or auditory feedback. Positive feedback is provided when alpha and theta waves increase.
4. Training Sessions: Conduct 20-30 minutes of training sessions, 2-3 times per week, for 20-40 sessions.
5. Progress Monitoring: Use anxiety and stress scales and follow-up qEEG to monitor changes.
Effectiveness of Neurofeedback for Tourette Syndrome
Research on neurofeedback for Tourette syndrome is still in its early stages, and findings vary. Some studies suggest positive outcomes, such as reduced tic severity and improved impulse control, while others report mixed or inconclusive results.
Studies Supporting Effectiveness:
1. A study by Sokhadze et al. (2010) found that neurofeedback training significantly reduced tic frequency and improved behavioral measures in TS patients.
2. Gevensleben et al. (2014) reported positive effects of neurofeedback on tic reduction and attentional control in children with TS.
Studies with Mixed Results:
1. Dehghani-Arani et al. (2013) found improvements in tic severity and cognitive performance but reported variability in individual responses.
2. Holtmann et al. (2011) observed improved tic severity but did not find significant effects on comorbid symptoms.
Challenges and Considerations:
- The heterogeneity of Tourette syndrome poses a challenge, as individuals may respond differently to neurofeedback.
- The lack of standardized protocols across studies makes it difficult to draw consistent conclusions.
- More extensive, well-controlled studies with long-term follow-up are needed to establish the efficacy and generalizability of neurofeedback for TS.
In conclusion, while promising evidence supports the effectiveness of neurofeedback for Tourette syndrome, further research is needed to establish standardized protocols, determine optimal electrode placements, and address variability in treatment outcomes. Neurofeedback for Tourette syndrome holds the potential to be a complementary
FAQ: Neurofeedback for Tourette Syndrome
Neurofeedback trains the brain to self-regulate its over-aroused and hyperexcitable motor circuits. By providing real-time feedback on brainwave activity, it teaches individuals to increase calming rhythms (like SMR) and decrease hyperactive patterns, leading to a reduction in the frequency and intensity of both motor and vocal tics.
Research shows promising results. Studies cited in the document found that neurofeedback training significantly improved motor and vocal tic symptoms in adolescents, with one study showing 75% of patients successfully increased the brainwaves associated with better motor control after training.
A primary protocol is Sensorimotor Rhythm (SMR) Training. This involves increasing SMR waves (12-15 Hz) in central brain areas (e.g., site C3) to enhance motor inhibition and promote calmness in the motor cortex, which directly helps reduce tics.
A typical course involves 20 to 40 sessions. Sessions are usually 20-30 minutes long and are recommended 2 to 3 times per week to help the brain learn and maintain new, calmer patterns of activity.
Yes. Since conditions like ADHD and anxiety are very common in people with Tourette’s, neurofeedback is beneficial. Protocols often improve executive function, impulse control, and relaxation, which can alleviate symptoms of these co-existing conditions alongside tics.
While medications can cause side effects and only manage symptoms, neurofeedback addresses the underlying neurological dysregulation. It is a learning-based process that teaches the brain to self-correct, offering the potential for long-term improvement without reliance on pharmaceuticals.
Common placement sites are over brain areas responsible for motor control and regulation. Key sites include Cz (vertex, for overall regulation), C3/C4 (over the sensorimotor cortex for motor tics), and Fz (midline frontal, for impulse control).














Add a Comment