EMG BIOFEEDBACK DEVICE. WHEN/HOW TO USE
In the dynamic realm of healthcare and wellness, technological advancements continually push the boundaries of what’s possible. Among the groundbreaking innovations, the EMG biofeedback device stands out as a beacon of progress, offering a window into the intricate interplay between mind and body. Electromyography (EMG) biofeedback, a revolutionary approach to physiological monitoring, has transformed the landscape of personalized health and performance optimization. From rehabilitation and sports performance enhancement to stress management and beyond, the potential of EMG biofeedback devices to revolutionize how we understand and interact with our physiology is truly awe-inspiring.
Table of Contents
ToggleElectromyography (EMG) biofeedback devices are versatile tools with applications spanning various medical and wellness domains. There are multiple conditions where the use of an EMG biofeedback device can be indicated.
Indications for EMG biofeedback device use
Muscle Rehabilitation
EMG biofeedback assists in rehabilitating injured or weakened muscles by providing real-time feedback on muscle activity. It aids in designing personalized rehabilitation programs.
Orthopedic Injuries
EMG biofeedback can be used for orthopedic rehabilitation, guiding patients to use specific muscle groups during exercises, and preventing compensatory movements.
Stroke Rehabilitation
Post-stroke patients benefit from EMG biofeedback to retrain and strengthen weakened muscles, enhancing overall motor function and mobility.
Chronic Pain Management
EMG biofeedback aids in managing chronic pain conditions by promoting awareness of muscle tension levels and teaching relaxation techniques.
Cerebral Palsy
EMG biofeedback helps children with cerebral palsy improve muscle control and coordination for enhanced motor function.
Posture Correction
EMG biofeedback devices can be used to correct and maintain proper posture by providing real-time feedback on muscle activity related to body positioning.
Scoliosis Management
EMG biofeedback can be integrated into scoliosis management programs to address muscle imbalances and support postural correction.
Sports Performance Enhancement
Athletes use EMG biofeedback to optimize muscle activation patterns, improve technique, optimize performance, and prevent injuries during training and competitions.
Stress Management
EMG biofeedback facilitates stress reduction by teaching individuals to recognize and control muscle tension, associated with stress (add muscles).
Anxiety Disorders
In anxiety management, EMG biofeedback assists in promoting relaxation and reducing muscle tension associated with stress.
Temporomandibular Joint (TMJ) Disorders
EMG biofeedback assists in reducing muscle tension in the jaw and face, contributing to the management of TMJ disorders.
Bruxism (Teeth Grinding)
EMG biofeedback assists in managing bruxism by helping individuals become aware of and control muscle activity in the jaw.
Headaches and Migraines
EMG biofeedback helps individuals identify and control muscle tension that may contribute to headaches and migraines.
Peripheral Nerve Injuries
EMG biofeedback aids in the rehabilitation process by guiding patients to activate specific muscles and regain control after peripheral nerve injuries.
Pre-operative and Post-operative Rehabilitation
EMG biofeedback helps prepare patients for surgery by strengthening relevant muscle groups and supports post-operative rehabilitation efforts.
Carpal Tunnel Syndrome
EMG biofeedback aids in managing muscle imbalances and tension associated with carpal tunnel syndrome.
Balance and Stability Training
EMG biofeedback is employed in balance training programs to enhance muscle control and stability, reducing the risk of falls, especially in the elderly.
Multiple Sclerosis
EMG biofeedback is used to manage symptoms of muscle weakness and spasticity in individuals with multiple sclerosis.
Parkinson’s Disease
EMG biofeedback supports individuals with Parkinson’s disease in managing muscle rigidity and optimizing motor function.
Attention Deficit Hyperactivity Disorder (ADHD)
EMG biofeedback may be used as part of a comprehensive treatment plan for ADHD, helping individuals improve focus and self-regulation.
Repetitive Strain Injuries (RSI)
EMG biofeedback assists in managing and preventing RSIs by promoting proper muscle activation and reducing strain during repetitive tasks.
Pelvic Floor Dysfunction
EMG biofeedback aids in the rehabilitation and strengthening of pelvic floor muscles, contributing to improved bladder control, and addressing issues such as incontinence and pelvic pain.
Neuromuscular Disorders
In various neuromuscular conditions, EMG biofeedback helps individuals maintain muscle function and mitigate the impact of the underlying disorder.
Biofeedback-Assisted Relaxation
EMG biofeedback supports stress management by promoting muscle relaxation through visual or auditory cues, aiding in overall well-being.
Muscle Imbalances
EMG biofeedback helps identify and address muscle imbalances, supporting targeted exercises to achieve symmetry and optimal function.
Spinal Cord Injuries
Following spinal cord injuries, EMG biofeedback plays a role in muscle rehabilitation and re-education to enhance mobility and functional independence.
Occupational Overuse Syndrome
EMG biofeedback is used to address muscle fatigue and tension related to occupational overuse, promoting healthier work habits.
Motor Control Disorders
EMG biofeedback aids individuals with motor control disorders in refining muscle coordination and movement patterns.
Pediatric Developmental Delays
For children with developmental delays, EMG biofeedback may assist in promoting appropriate muscle development and motor skills.
Bell’s Palsy
For individuals with facial muscle weakness due to Bell’s Palsy, EMG biofeedback assists in retraining facial muscles, contributing to improved symmetry and function.
Phantom Limb Pain
EMG biofeedback is explored as a potential tool in the management of phantom limb pain, helping individuals retrain their brain’s perception of the missing limb.
Amyotrophic Lateral Sclerosis (ALS)
In the early stages of ALS, EMG biofeedback may assist in maintaining muscle function and delaying the progression of muscle weakness.
Gait Disorders
EMG biofeedback can be employed to address muscle imbalances and coordination issues affecting gait, improving overall walking patterns.
Rheumatoid Arthritis
EMG biofeedback may assist individuals with rheumatoid arthritis in maintaining joint function and managing muscle stiffness.
Ergonomics Training
EMG biofeedback devices can be used to assess and optimize muscle activity in occupational settings, aiding in the prevention of repetitive strain injuries.
It’s crucial to note that while EMG biofeedback devices can be beneficial for these conditions, their usage should be guided by healthcare professionals based on individual needs and circumstances.

Contraindications for EMG biofeedback device use
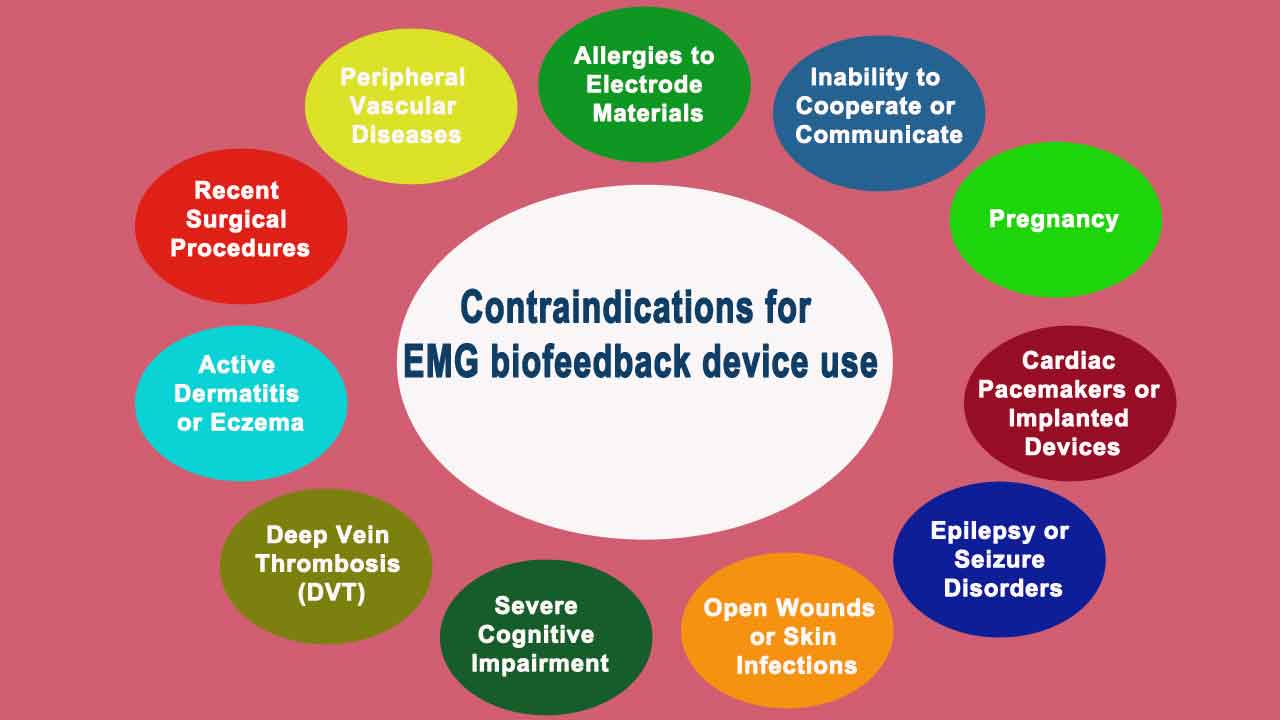
While EMG (Electromyography) biofeedback devices are generally safe and well-tolerated, certain contraindications and precautions should be considered. It’s important to consult with a healthcare professional before using an EMG biofeedback device, as individual circumstances may vary.
Open Wounds or Skin Infections
Do not use an EMG biofeedback device over areas with open wounds, cuts, abrasions, or skin infections, as it may lead to further complications or discomfort.
Active Dermatitis or Eczema
Individuals with active dermatitis or eczema may experience increased irritation when using EMG electrodes. It is advisable to avoid placing electrodes over affected skin areas.
Peripheral Vascular Diseases
Individuals with peripheral vascular diseases or circulatory disorders should use EMG biofeedback devices with caution, as impaired blood flow may affect the accuracy of readings.
Deep Vein Thrombosis (DVT)
Using EMG biofeedback devices on areas affected by deep vein thrombosis can pose a risk, as it may interfere with blood circulation and exacerbate the condition.
Pregnancy
While there is limited evidence regarding the safety of EMG biofeedback during pregnancy, it’s generally advisable to avoid using such devices over the abdominal or pelvic region, especially without specific guidance from a healthcare professional.
Cardiac Pacemakers or Implanted Devices
Individuals with cardiac pacemakers or other implanted electronic devices may need to avoid using EMG biofeedback devices near the site of implantation, as the electrical signals could potentially interfere with these devices.
Epilepsy or Seizure Disorders
EMG biofeedback devices that use visual or auditory feedback may trigger seizures in individuals with a history of epilepsy or seizure disorders.
Severe Cognitive Impairment
Individuals with severe cognitive impairment may find it challenging to understand and respond to the feedback provided by the EMG biofeedback device.
Allergies to Electrode Materials
Some individuals may be allergic to the materials used in EMG electrodes. It’s essential to check for allergies or skin sensitivities before applying electrodes.
Inability to Cooperate or Communicate
Effective use of EMG biofeedback requires cooperation and communication. Individuals who are unable to follow instructions or provide feedback may not benefit from the device.
Recent Surgical Procedures
Avoid using EMG biofeedback devices over areas that have undergone recent surgical procedures until the healing process is sufficiently advanced.
Always consult with a healthcare professional, such as a physical therapist or a physician, to assess individual suitability and receive personalized guidance before using an EMG biofeedback device, especially for those with pre-existing medical conditions or concerns.
General steps for EMG biofeedback device use
Using an EMG (Electromyography) biofeedback device involves several steps to ensure accurate and effective monitoring of muscle activity. Below is a general guide on how to use an EMG biofeedback device:
Step 1: Set Up the Device
1. Prepare the Skin:
• Ensure the skin over the targeted muscle area is clean and dry.
• Remove any lotions, oils, or sweat that may interfere with electrode adhesion.
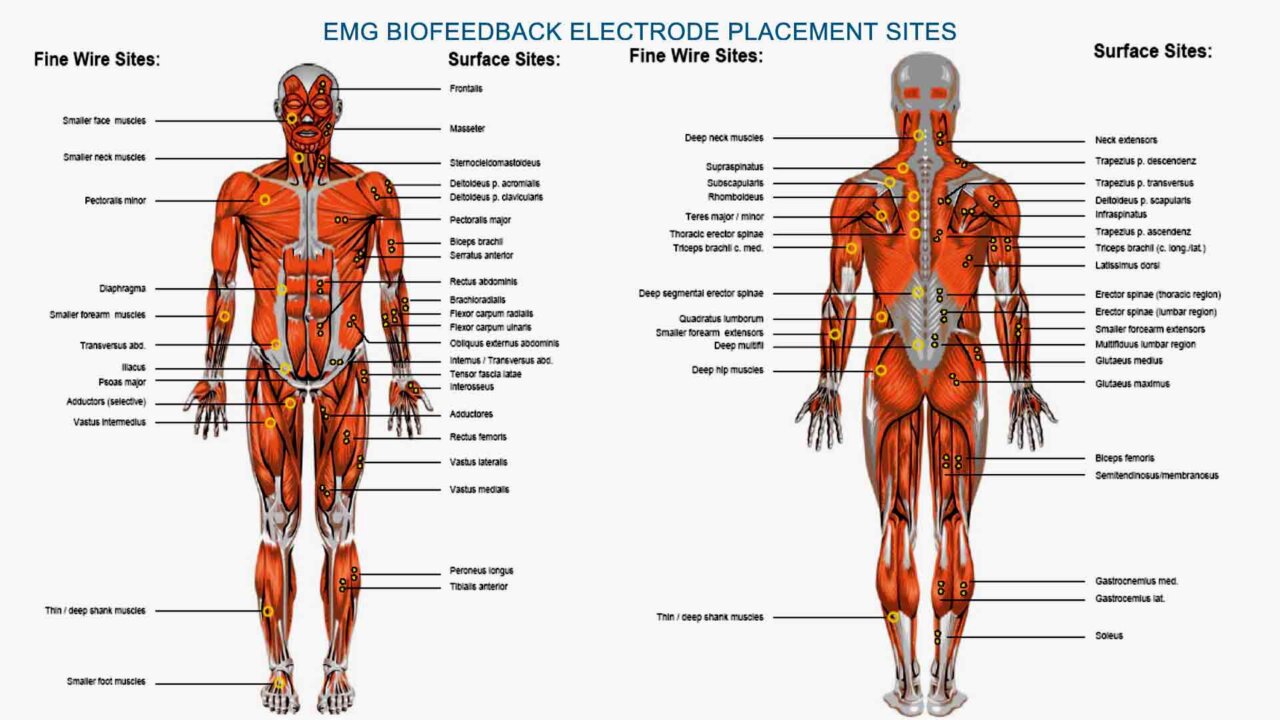
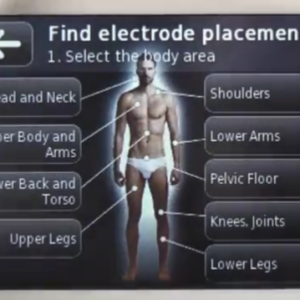
2. Attach Electrodes:
• Connect the EMG electrodes to the device according to the manufacturer’s instructions.
• Place the electrodes over the muscles you intend to monitor. Common locations include the muscle belly or along the muscle fibers.
3. Secure the Device:
• Secure the EMG biofeedback device in a comfortable and accessible location. Some devices may be strapped to the body or attached to clothing.
Step 2: Calibrate the Device
1. Zero Baseline:
• Establish a baseline to relax the targeted muscle completely. This provides a reference point for subsequent readings.
2. Set Thresholds:
• Adjust the sensitivity or threshold levels on the EMG device. This ensures that the device detects muscle activity above a certain level and provides feedback when necessary.
Step 3: Perform Biofeedback Training
1. Initiate Monitoring:
• Start the EMG biofeedback device to monitor real-time muscle activity.
• Perform specific movements or exercises that target the monitored muscle group.
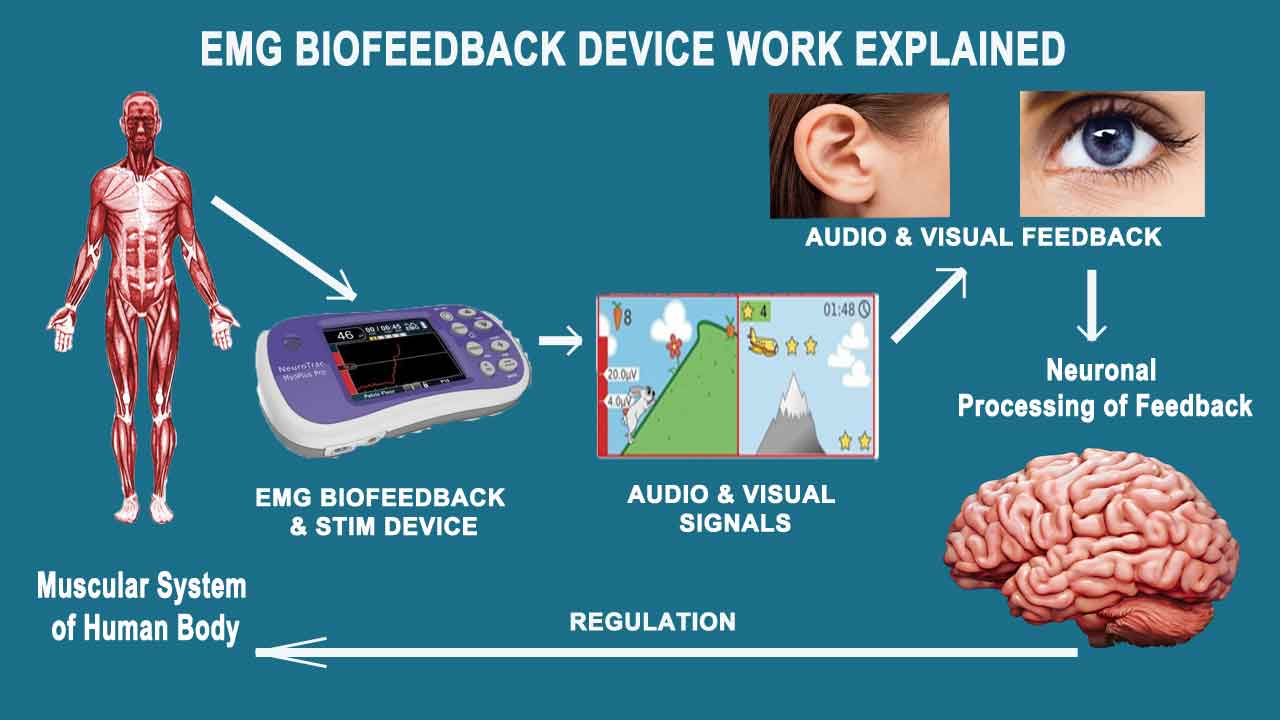
2. Visual or Auditory Feedback:
• Utilize the feedback mechanism provided by the device, which can include visual displays, sounds, or other indicators.
• Adjust muscle activity based on the feedback received. For example, reducing muscle tension or increasing muscle activation.
3. Repeat and Refine:
• Repeat the exercises multiple times, allowing to refine muscle control based on the feedback.
• Encourage gradual improvements and adjustments to optimize muscle function.
Step 4: Data Analysis
1. Review Data:
• After a biofeedback session, review the data collected by the device. Many devices store session data for later analysis.
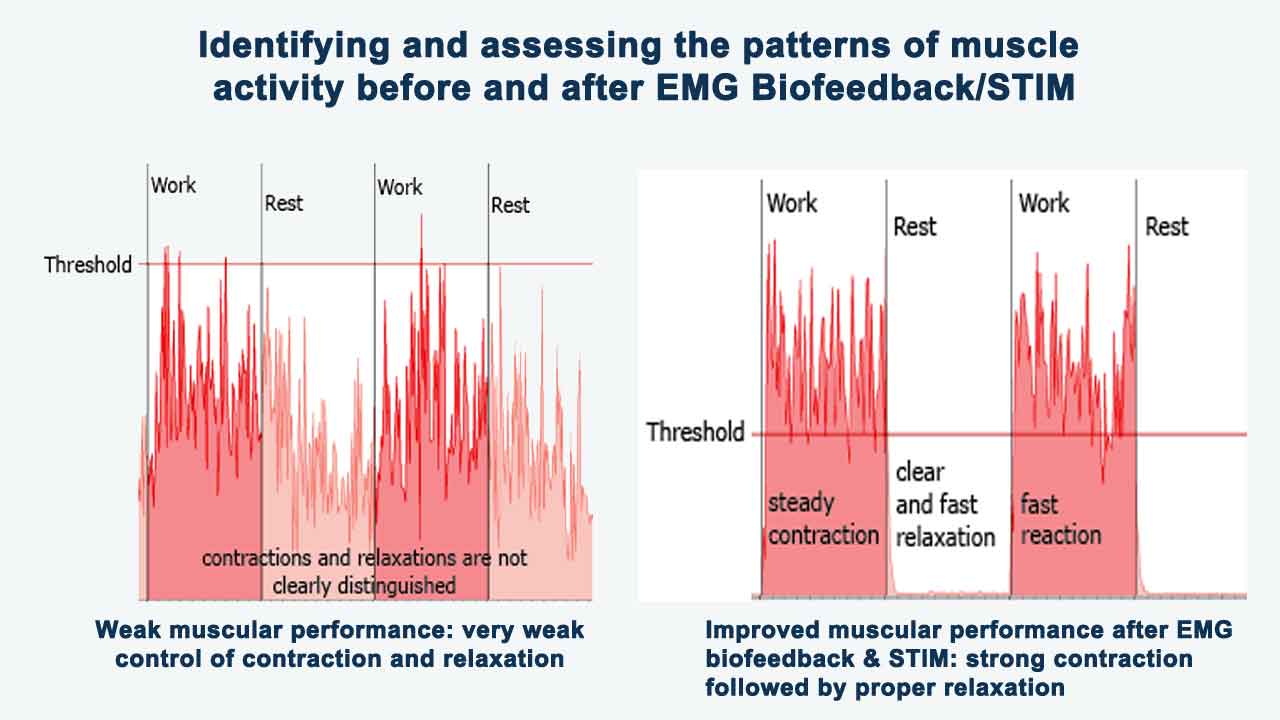
2. Identify Patterns:
• Identify patterns of muscle activity and assess how well you can control and modulate your muscle function.
Step 5: Progress Monitoring
1. Adjust Training Plan:
• Based on the analysis of the data, adjust the biofeedback training plan to address specific areas of improvement or challenges.
2. Set Goals:
• Set realistic goals for muscle control and function. This may involve increasing muscle strength, reducing tension, or improving coordination.
Step 6: Regular Evaluation
Follow-Up Sessions:
• Schedule regular follow-up sessions to reassess progress and make any necessary adjustments to the biofeedback training plan.
By following these steps, users can effectively harness the power of EMG biofeedback devices to enhance muscle control, rehabilitation, and overall well-being.
How to choose right EMG biofeedback device
Choosing the right EMG (Electromyography) biofeedback device involves considering various factors to ensure that the device meets your specific needs and requirements. Here are key considerations to help guide your decision:
1. Professional Guidance:
Consult with a healthcare professional, such as a physical therapist, occupational therapist, or physician, before selecting an EMG biofeedback device. Their expertise can help identify the most suitable device based on your condition and goals.
2. Intended Use:
Define the primary purpose for using the EMG biofeedback device. Whether it’s for rehabilitation, sports performance, stress management, or another application, choose a device that aligns with your specific goals.
3. Type of Feedback:
Determine the type of feedback that suits your preferences and requirements. EMG biofeedback devices can provide visual, auditory, or tactile feedback. Consider which mode would be most effective for your training and rehabilitation needs.
4. Ease of Use:
Select a device with user-friendly features and controls. Consider factors such as the device’s interface, setup process, and the clarity of feedback. Devices with intuitive designs are generally more accessible to users.
5. Portability:
Assess whether you need a portable device for use at home or on the go. Portable EMG biofeedback devices are suitable for individuals who require flexibility in their training routine.
6. Number of Channels:
Consider the number of channels the device offers. Multi-channel devices allow for the simultaneous monitoring of multiple muscle groups, providing a more comprehensive view of muscle activity.
7. Adjustable Sensitivity:
Opt for a device that allows you to adjust sensitivity levels. This feature is valuable for tailoring the device to your specific needs and ensuring accurate readings.
8. Customization Options:
Look for devices that offer customization options for feedback parameters, such as threshold levels and visual/audio cues. The ability to tailor the device to your requirements enhances its effectiveness.
9. Data Storage and Analysis:
Evaluate whether the device can store and analyze session data. This feature can be beneficial for tracking progress over time and adjusting your training plan accordingly.
10. Compatibility:
Ensure that the EMG biofeedback device is compatible with your existing devices, such as smartphones, tablets, or computers. Compatibility with popular operating systems and devices can enhance the user experience.
11. Battery Life:
Consider the battery life of the device, especially if you plan to use it for extended periods. Longer battery life reduces the frequency of recharging or replacing batteries.
12. Cost and Value:
Compare the costs of different EMG biofeedback devices and weigh them against the features offered. Consider the value provided in terms of functionality, durability, and overall effectiveness.
13. User Reviews:
Read user reviews and testimonials to gain insights into the experiences of others who have used the specific EMG biofeedback device you are considering. This can provide valuable information about the device’s performance and user satisfaction.
Remember to prioritize safety and effectiveness, and when in doubt, seek professional advice to ensure that the chosen EMG biofeedback device is suitable for your individual needs and health status.
Main type of EMG Biofeedback device
There are various types of EMG biofeedback devices available, each with its own set of features, advantages, and limitations. Here are some main types of EMG biofeedback devices along with their pros and cons.
1. Surface Electromyography (sEMG) Biofeedback Devices:
• Pros:
• Non-invasive: sEMG devices are typically non-invasive and easy to use.
• Versatility: Suitable for various applications, including muscle rehabilitation, sports training, and stress management.
• Real-time Feedback: Provides real-time feedback on muscle activity, aiding in immediate adjustments.
• Cons:
• Surface Sensitivity: This may be affected by factors such as skin impedance and movement artifacts.
• Single Muscle Focus: Some devices may focus on monitoring a single muscle group at a time.
2. Needle EMG Biofeedback Devices:
• Pros:
• High Precision: Provides detailed and precise information about muscle activity.
• Deep Muscle Monitoring: Can access deeper muscles for monitoring.
• Clinical Use: Commonly used in clinical settings for diagnostic purposes.
• Cons:
• Invasive: Requires insertion of needle electrodes into the muscle, which may be uncomfortable.
• Limited for Home Use: Not practical for regular home-based rehabilitation or training.
3. Wireless EMG Biofeedback Devices:
• Pros:
• Portability: Allows for greater flexibility and mobility during use.
• Convenience: No cumbersome wires, making it more user-friendly.
• Ease of Use: Convenient for home-based applications.
• Cons:
• Battery Dependency: Requires regular charging or battery replacement.
• Signal Interference: Potential for signal interference in wireless transmission.
4. Multichannel EMG Biofeedback Devices:
• Pros:
• Comprehensive Monitoring: Can simultaneously monitor multiple muscle groups.
• Detailed Analysis: Provides a more comprehensive view of muscle coordination.
• Versatility: Useful in rehabilitation and sports training for addressing complex movement patterns.
• Cons:
• Cost: Multichannel devices may be more expensive than single-channel counterparts.
• Complexity: May have a steeper learning curve for users due to the increased number of channels.
5. Combined EMG Biofeedback and other modalities Biofeedback Devices:
• Pros:
• Integrated Monitoring: Combines EMG with other biofeedback modalities (e.g., temperature, heart rate) for a holistic approach.
• Comprehensive Feedback: Provides a broader range of physiological information for a more holistic view.
• Cons:
• Complexity: Integration of multiple feedback modalities may increase device complexity.
• Cost: Combined devices may be more expensive than single-modal devices.
6. Wearable EMG Biofeedback Devices:
• Pros:
• Convenience: Can be worn discreetly throughout the day.
• Long-Term Monitoring: Suitable for continuous monitoring over extended periods.
• Integration with Smart Devices: Some devices can sync with smartphones or smartwatches for data tracking.
• Cons:
• Limited Precision: May sacrifice some precision compared to traditional devices.
• Battery Life: Dependent on battery life, which may require regular charging.
Choosing the right type of EMG biofeedback device depends on your specific needs, preferences, and the intended application. It’s advisable to consult with healthcare professionals to determine the most appropriate device for your circumstances.
Role and Types of Muscle Stimulation in EMG Biofeedback Devices
In the context of EMG (Electromyography) biofeedback devices, “STIM” typically refers to electrical stimulation or neuromuscular electrical stimulation (NMES). NMES involves the application of electrical currents to stimulate nerves and induce muscle contractions. This can be integrated into EMG biofeedback devices to enhance rehabilitation and recovery.
Muscular stimulation, particularly in the context of electrotherapy or neuromuscular electrical stimulation (NMES), can be classified based on various factors.
1. Functional Classification:
• a. NMES (Neuromuscular Electrical Stimulation):
Description: Involves the use of electrical currents to stimulate nerves and induce muscle contractions.
Mechanism: NMES delivers electrical impulses to the nerves, causing muscle contractions. This mimics the natural electrical signals from the nervous system, promoting muscle activation.
Applications: Muscle strengthening, motor re-education, rehabilitation after injury or surgery.
Indication for Use:
• Muscle Strengthening: Helps individuals with muscle weakness or atrophy to build strength.
• Motor Re-Education: Facilitates the relearning of motor patterns after injury or surgery.
• Pain Management: Can be used for pain relief by promoting blood circulation and reducing muscle spasms.
• b. FES (Functional Electrical Stimulation):
Description: Applies electrical stimulation during functional activities, often synchronized with movement.
Mechanism: FES involves the application of electrical stimulation to activate specific muscles during functional activities. It is often synchronized with movement.
Applications: Gait training, upper extremity function restoration.
Indication for Use:
• Gait Training: Helps individuals with walking impairments by stimulating appropriate muscles during specific phases of gait.
• Upper Extremity Function: Assists in restoring arm and hand function in conditions like stroke or spinal cord injury.
• c. Russian Stimulation:
Description: High-frequency alternating current NMES, primarily used for muscle strengthening.
Mechanism: Russian stimulation is a type of NMES with a high-frequency alternating current. It is often used for muscle strengthening and endurance.
Applications: Building muscle mass, sports training.
Indication for Use:
• Muscle Strengthening: Particularly effective for building muscle mass and strength.
• Sports Training: Used in athletic settings to enhance muscle performance.
• d. TENS (Transcutaneous Electrical Nerve Stimulation):
• Mechanism: TENS stimulates sensory nerves to reduce the perception of pain. It does not induce muscle contractions.
• Indication for Use:
• Pain Management: Alleviates pain by modulating pain signals sent to the brain.
• Symptomatic Relief: Can be used for various conditions, including chronic pain and musculoskeletal disorders.
e. ETS – EMG triggered stimulation
• Mechanism:
EMG-triggered stimulation (ETS) is a technique that involves using electromyography (EMG) signals to trigger and control electrical stimulation of muscles.
• Indication for Use:
• Rehabilitation of weak muscles in patients with stroke and/or paresis, with motor recovery and improvement in muscle strength
• Treatment of stress and urge urinary stress incontinence, with an improvement of symptoms, reduction in leakage, and improvement in bladder control
• Reduction in symptoms in patients with faecal incontinence
2. Purpose Classification
• a. Muscle Activation and Strengthening:
Stimulation Type: NMES, Russian Stimulation.
Applications: Building muscle mass, improving strength and endurance.
How it Works: Electrical stimulation induces muscle contractions, promoting muscle activation and strengthening.
Contribution to Healing: Enhances muscle mass, strength, and endurance, particularly in cases of muscle atrophy or weakness.
• b. Motor Re-Education:
• Stimulation Type: NMES, FES.
• Applications: Relearning optimal movement patterns after injury or surgery.
• How it Works: Stimulating specific muscles aids in relearning optimal movement patterns.
• Contribution to Healing: Supports the rehabilitation process after injuries, surgeries, or neuromuscular disorders.
• c. Pain Management:
• Stimulation Type: TENS (Transcutaneous Electrical Nerve Stimulation).
• Applications: Symptomatic relief for various pain conditions.
• How it Works: TENS modulates pain signals, providing symptomatic relief.
• Contribution to Healing: Helps manage pain during rehabilitation, facilitating increased mobility and exercise.
d. Circulation improvement:
• How it Works: Stimulation can enhance blood flow to the stimulated area.
• Contribution to Healing: Promotes oxygen and nutrient delivery, accelerating the healing process and reducing inflammation.
3. Frequency Classification:
• a. Low-Frequency Stimulation:
• Frequency Range: Typically below 10 Hz.
• Applications: Muscle relaxation, pain relief.
• b. Medium-Frequency Stimulation:
• Frequency Range: Around 50-100 Hz.
• Applications: Muscle strengthening, endurance training.
• c. High-Frequency Stimulation:
• Frequency Range: Above 100 Hz.
• Applications: Russian Stimulation for muscle hypertrophy, certain pain management protocols.
4. Clinical Setting Classification:
• a. Home-Use Devices:
• Description: Compact, user-friendly devices suitable for home-based rehabilitation.
• Applications: Post-surgical recovery, muscle strengthening at home.
• b. Clinical-Grade Devices:
• Description: Professional-grade devices used in clinical settings.
• Applications: Rehabilitation in physical therapy clinics, hospitals.
5. Specific Application Classification:
• a. Gait Training Devices:
• Description: Typically FES devices are designed for improving gait in individuals with mobility impairments.
• Applications: Rehabilitation after stroke, spinal cord injury.
• b. Post-Surgical Rehabilitation Devices:
• Description: NMES devices for recovery facilitating, preventing muscle atrophy, and promoting recovery after surgery.
• Applications: Orthopedic surgeries, joint replacements.
• c. Sports Training Devices:
• Description: Russian Stimulation devices used for sports-specific muscle training.
• Applications: Athletic performance enhancement, muscle conditioning.
d. Neurological Conditions:
• Description: FES for gait training, NMES for motor re-education.
• Applications: Assists individuals with neurological conditions in improving mobility and function.
e. Orthopedic Injuries:
• Description: NMES for muscle strengthening, TENS for pain management.
• Applications: Supports rehabilitation after orthopedic injuries, reducing pain and promoting muscle recovery.
f. Chronic Pain Management:
• Description: TENS for pain modulation.
• Applications: Offers symptomatic relief for individuals with chronic pain conditions.
6. Mode of Operation Classification:
• a. Asynchronous Stimulation:
• Description: Continuous stimulation without synchronization with movement.
• Applications: Muscle activation, pain relief.
• b. Synchronous Stimulation:
• Description: Stimulation synchronized with specific movements or functional tasks.
• Applications: Functional electrical stimulation during gait, and specific motor tasks.
These classifications help categorize muscular stimulation based on its intended purpose, frequency characteristics, clinical settings, and specific applications. The selection of the appropriate type of stimulation depends on individual needs, conditions, and treatment goals, and it should be guided by healthcare professionals.
The integration of electrical stimulation in EMG biofeedback devices provides a comprehensive approach to neuromuscular rehabilitation and contributes significantly to the healing and recovery process.
Contraindication for Neuromuscular Electrical Stimulation (NMES)
Neuromuscular Stimulation should not be used by:
• Patients fitted with demand-style cardiac pacemakers
• During pregnancy (unless medically advised)
• Patients with undiagnosed pain conditions
• Do not place electrodes:
– Over carotid sinus nerves
– Over larynx or trachea
– Inside mouth
– On anesthetized or desensitized skin
– Do not drive a vehicle while the device is stimulating and attached to your body
– Do not apply stimulation across or through the head, directly on the eyes, covering the mouth, on the front of the neck (especially the carotid sinus), or via electrodes placed on the chest and upper back or crossing over the heart.
• Skin irritation from the treatment of NMS or EMG itself does not generally occur. However, rubber electrodes may irritate some skin types, therefore, in this case, we recommend using hypoallergenic self-adhesive electrodes.
• The patient should only use the unit for what it was prescribed for
• Do not immerse the unit in water or any other liquid substance
• Do not use stimulation on your facial area unless you are under strict guidance from a qualified clinician.
• Do not apply stimulation across or through the head, directly on the eyes, covering the mouth, on the front of the neck (especially the carotid sinus), or via electrodes placed on the chest and upper back or crossing over the heart.
EMG Biofeedback Device for Use at Home
NeuroTrac® Simplex is a single-channel EMG biofeedback device suitable for diagnosing, monitoring, and treating various neuromuscular problems.
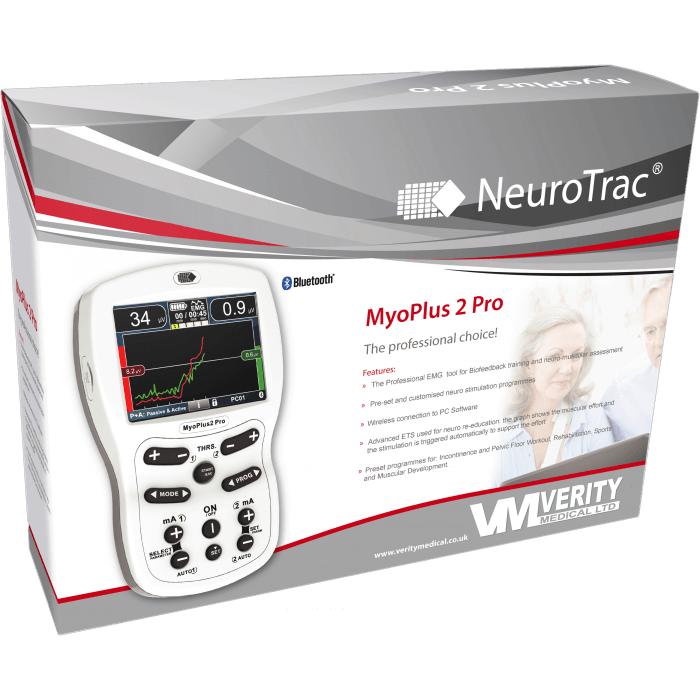
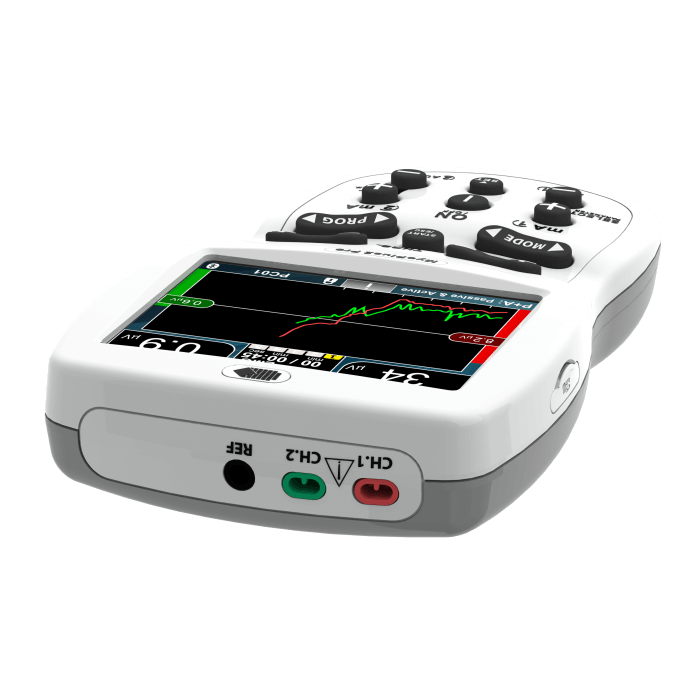
NeuroTrac MyoPlus2 Pro is a new and improved touch-screen with a full-color display EMG and EMS biofeedback device. The new user-friendly interface makes it a self-explanatory unit with interactive learning on the go, including electrode placement, running EMG graphs as well as many other helpful tools.
NeuroTrac MyouPlus Pro