Home Neurofeedback for Disorders
In recent years, the field of neuroscience has witnessed a remarkable advancement in therapeutic techniques, and one approach that stands out is Home Neurofeedback. This innovative method offers the convenience of receiving neurofeedback therapy in the comfort of one’s home. Neurofeedback, also known as EEG biofeedback, involves real-time monitoring and regulation of brain activity to address various disorders and promote overall well-being. This article delves into the application of Home Neurofeedback across different health conditions, exploring its efficacy, benefits, and potential impact on individuals seeking alternative and accessible treatment options. From anxiety and attention disorders to sleep disturbances and beyond, Home Neurofeedback opens new doors for personalized, effective, and convenient brain-focused therapies.
Table of Contents
Toggle- Home Neurofeedback for Disorders
- The Science Behind Home Neurofeedback
- Neurofeedback Protocols for Various Pathological States
- 1. Alpha Training Protocol
- 2. Alpha-Theta Training Protocol
- 3. SMR (Sensorimotor Rhythm) Training Protocol
- 4. Beta Training Protocol
- 5. Theta/Beta Training:
- 6. SCP (Slow Cortical Potential) Training
- 7. Gamma Training:
- 8. Low Beta Training:
- 9. Theta Training:
- 10. Alpha-Asymmetry Training:
- 11. SMR-Theta Training:
- 12. Slow Wave Training:
- 13. Alpha-Theta-Gamma Training:
- 14. High Beta Training:
- 15. Alpha Peak Frequency Training:
- Pathological States Where Home Neurofeedback can be used
- Home Neurofeedback for Anxiety and Stress Disorders
- Home Neurofeedback for Panic Disorder
- Home Neurofeedback and Attention Disorders
- Home Neurofeedback for Dyscalculia
- Home Neurofeedback for Dyslexia
- Home Neurofeedback and Sleep Disturbances
- Home Neurofeedback and Mood Disorders
- Home Neurofeedback for Bipolar Disorder
- Home Neurofeedback for Obsessive-Compulsive Disorder (OCD)
- Home Neurofeedback for Chronic Pain
- Home Neurofeedback for Migraine Disorders
- Home Neurofeedback for Fibromyalgia
- Home Neurofeedback for Traumatic Brain Injury (TBI)
- Home Neurofeedback for Substance Use Disorders (SUD)
- Home Neurofeedback for Autistic Spectrum Disorder (ASD)
- Home Neurofeedback for Borderline Personality Disorder (BPD)
- Home Neurofeedback for Eating Disorders
- Home Neurofeedback for Tinnitus
- Home Neurofeedback for Specific Phobias
- Home Neurofeedback for Schizophrenia
- Home Neurofeedback for Chronic Fatigue Syndrome (CFS)
- Home Neurofeedback for Irritable Bowel Syndrome (IBS)
- Home Neurofeedback for Post-Traumatic Stress Disorder (PTSD)
- Home Neurofeedback for Parkinson’s Disease
- Home Neurofeedback for Multiple Sclerosis (MS)
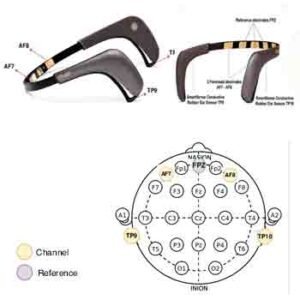
- Home Neurofeedback devices
- Neurofeedback Personal Use Device Classification in Accordance with Brain Region Electrode Placement
Neurofeedback is a noninvasive, drug-free approach that helps individuals observe and regulate their brain activity in real time. This approach uses electroencephalography (EEG) technology to measure brainwave patterns, providing valuable insights into brain function. Through visual or auditory feedback, participants can learn to modulate their brainwaves. As a result, they enhance cognitive performance, emotional regulation, and mental well-being.
The allure of Home Neurofeedback lies not only in its remarkable effectiveness but also in the accessibility and convenience it offers. Traditionally, neurofeedback therapy was available only in specialized clinics, requiring frequent visits that could be logistically challenging and time-consuming. However, recent advancements in EEG technology have led to the development of portable, user-friendly home neurofeedback devices that enable individuals to embark on their neurofeedback journey within the comfort of their living spaces. This paradigm shift has opened new horizons for personalized brain training, making neurofeedback accessible to a broader population and paving the way for empowering self-guided therapies.
The Science Behind Home Neurofeedback
To understand the impact of Home Neurofeedback, it is crucial to delve into the scientific principles that underpin this innovative approach. The brain’s complex network of neurons communicates through electrical impulses, creating distinct brainwave patterns associated with different mental states and functions. These brainwave frequencies can be categorized into bands, such as delta, theta, alpha, beta, and gamma, each serving a specific role in cognitive and emotional processing.
Neurofeedback training therapy operates on the principle of neuroplasticity, which is the brain’s ability to reorganize and adapt its neural connections in response to new experiences and learning. By monitoring brain activity through EEG, neurofeedback training provides individuals with real-time information about their brainwave patterns associated with specific mental states and functions.
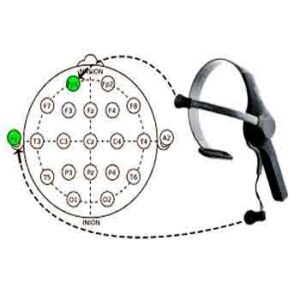
During a neurofeedback session, electrodes on the scalp measure these brainwave patterns, transmitting the data to a computer interface. Participants are then presented with real-time feedback, often visual cues or sounds, representing their brainwave activity. As individuals learn to recognize and modulate their brainwave patterns through positive reinforcement, they can achieve desired mental states and emotional balance. Over time, this process facilitates lasting changes in the brain’s neural connectivity, improving self-regulation and resilience against various disorders.
Neurofeedback Protocols for Various Pathological States
While neurofeedback training protocols can vary depending on the specific needs of individuals, some standard techniques are used for various pathological states:
1. Alpha Training Protocol
The Alpha Training protocol aims to increase the production of alpha brainwaves (8-12 Hz), promoting relaxation and calmness. It is beneficial for individuals experiencing anxiety, stress, and insomnia, as it helps induce a state of deep relaxation and tranquility.
Electrode Placement involves positioning on the occipital region of the scalp, specifically over the occipital cortex (O1 and O2).
2. Alpha-Theta Training Protocol
Alpha-theta training combines alpha and theta brainwave activity to induce deep relaxation and heightened awareness. This protocol is used for various conditions, including anxiety, PTSD, addiction disorders, substance use disorders, trauma-related disorders, and emotional regulation. It aims to increase alpha waves (associated with relaxation) and theta waves (linked to subconscious processing) while decreasing beta waves (related to conscious arousal). The combination of alpha and theta training can help individuals process emotional trauma and achieve a state of deep relaxation.
Electrode Placement involves positioning over the occipital cortex (Oz), temporal cortex (T3, T4), and parietal cortex (Pz).
3. SMR (Sensorimotor Rhythm) Training Protocol
SMR training targets the sensorimotor rhythm (12-15 Hz) and improves attention and focus. It is commonly used for conditions like attention deficit hyperactivity disorder (ADHD) and cognitive enhancement. Moreover, enhancing the sensorimotor rhythm allows individuals to experience better cognitive control and reduced impulsivity.
Electrode Placement involves positioning over the central cortex, specifically on C3 and C4, which are situated above the sensorimotor areas.
4. Beta Training Protocol
Beta Training aims to increase beta brainwave activity (15-18 Hz), which is associated with alertness and cognitive focus. It is used for conditions such as depression, attention deficits, and cognitive enhancement. Beta training focuses on increasing beta waves associated with alertness and mental functioning. This protocol can help boost mood and mental performance.
Electrode Placement involves positioning over the frontal cortex (Fz, F3, F4), central cortex (C3, C4), and parietal cortex (Pz).
5. Theta/Beta Training:
Theta/Beta training aims to reduce symptoms of anxiety and stress by increasing beta brainwave activity (15-18 Hz) and decreasing theta brainwave activity (4-8 Hz). It is commonly used for anxiety disorders and post-traumatic stress disorder (PTSD). As a result, individuals can experience relief from anxiety and improved emotional regulation.
Electrode Placement involves positioning over the frontal cortex (Fz, F3, F4), central cortex (C3, C4), and parietal cortex (Pz).
6. SCP (Slow Cortical Potential) Training
SCP training involves regulating slow cortical potentials, which are brainwave shifts associated with cognitive and motor functions. It targets these potentials to regulate cortical excitability and reduce the occurrence of seizures or migraines. Moreover, it is used for various conditions, including traumatic brain injury (TBI), epilepsy, migraines, and attention deficits. As a result, individuals may experience improved brain function and fewer symptoms.
Electrode Placement involves positioning over the frontal cortex (Fz, F3, F4), central cortex (C3, C4), and parietal cortex (Pz).
7. Gamma Training:
Gamma training targets gamma brainwave activity (25-100 Hz), associated with higher cognitive functions and information processing. Moreover, it is used for cognitive enhancement and may benefit conditions involving cognitive deficits. As a result, individuals can experience improved mental performance and better information processing.
Electrode Placement involves positioning over the frontal cortex (Fz, F3, F4), central cortex (C3, C4), and parietal cortex (Pz).
8. Low Beta Training:
Low-beta training targets the low-beta brainwave range (12-15 Hz) and improves focus and cognitive performance. It is commonly used for conditions such as ADHD and cognitive enhancement. As a result, individuals may experience better attention and mental clarity.
Electrode Placement involves positioning over the frontal cortex (Fz, F3, F4), central cortex (C3, C4), and parietal cortex (Pz).
9. Theta Training:
Theta training focuses on increasing theta brainwave activity (4-8 Hz), associated with deep relaxation and creativity. Moreover, it is used for stress reduction, creative enhancement, and emotional regulation. As a result, individuals can achieve greater relaxation and enhance their creative abilities.
Electrode Placement involves positioning over the frontal cortex (Fz, F3, F4), central cortex (C3, C4), and parietal cortex (Pz).
10. Alpha-Asymmetry Training:
Alpha-asymmetry training aims to balance alpha brainwave activity between the left and right hemispheres of the brain. It is commonly used for conditions like depression and emotional dysregulation. As a result, individuals may experience improved emotional balance and mood stability.
Electrode Placement involves positioning over the frontal cortex (F3, F4), central cortex (C3, C4), and parietal cortex (Pz).
11. SMR-Theta Training:
SMR-Theta training combines SMR and theta brainwave activity to improve focus and relaxation. It is commonly used for conditions involving stress reduction and cognitive enhancement. As a result, individuals can experience enhanced mental clarity and reduced stress levels.
Electrode Placement involves positioning over the central cortex (C3, C4), parietal cortex (Pz), and occipital cortex (Oz).
12. Slow Wave Training:
Slow-wave training focuses on increasing slow-wave brain activity (1-4 Hz), associated with deep sleep and relaxation. Moreover, it is used for conditions involving sleep disturbances and insomnia. As a result, individuals can experience improved sleep quality and greater relaxation.
Electrode Placement involves positioning over the central cortex (C3, C4), parietal cortex (Pz), and occipital cortex (Oz).
13. Alpha-Theta-Gamma Training:
Alpha-theta-gamma training combines alpha, theta, and gamma brainwave activity to induce deep relaxation and heightened cognitive processing. It is commonly used for conditions involving cognitive enhancement and peak performance. As a result, individuals can experience improved mental clarity and optimal performance in various activities.
Electrode Placement involves positioning over the occipital cortex (Oz), temporal cortex (T3, T4), and parietal cortex (Pz).
14. High Beta Training:
High beta training focuses on increasing high beta brainwave activity (20-30 Hz), associated with cognitive focus and motor coordination. Moreover, it is used for conditions involving cognitive enhancement and motor skill improvement. As a result, individuals can experience enhanced focus and better coordination in their activities.
Electrode Placement involves positioning over the frontal cortex (Fz, F3, F4), central cortex (C3, C4), and parietal cortex (Pz).
15. Alpha Peak Frequency Training:
Alpha Peak Frequency Training aims to increase the individual’s dominant alpha brainwave frequency. It is commonly used for conditions involving cognitive enhancement and peak performance. As a result, individuals can experience improved mental clarity and optimal performance in various tasks.
Electrode Placement involves positioning over the occipital cortex (Oz), temporal cortex (T3, T4), and parietal cortex (Pz).
Note: Experienced healthcare professionals should determine the selection of specific neurofeedback protocols and electrode placements based on each individual’s unique needs and responses to treatment. Neurofeedback should be considered part of a comprehensive treatment plan, not a standalone intervention for these conditions.
Pathological States Where Home Neurofeedback can be used
Home Neurofeedback for Anxiety and Stress Disorders
Anxiety disorders represent a widespread mental health challenge, affecting millions of individuals worldwide. Characterized by excessive worry, fear, and physical symptoms like rapid heartbeat and sweating, anxiety can significantly impair daily functioning and diminish overall quality of life. Fortunately, Home Neurofeedback has emerged as a promising intervention for alleviating anxiety symptoms.
Neurofeedback has shown effectiveness in reducing symptoms of anxiety disorders, including generalized anxiety, social anxiety, and post-traumatic stress disorder (PTSD). Specifically, the neurofeedback approach for anxiety and stress disorders aims to reduce excessive anxiety and stress responses by promoting relaxation, emotional regulation, and cognitive control. By training individuals to achieve calmer brainwave patterns, neurofeedback can help reduce overactivity in regions associated with anxiety responses. As a result, individuals may experience greater emotional stability and improved coping mechanisms.
Neurofeedback protocols for anxiety and stress disorders typically involve training individuals to increase alpha brainwave activity (8-12 Hz) and decrease beta brainwave activity (15-18 Hz). Alpha brainwaves are associated with a relaxed and calm state, while reducing beta brainwaves can help reduce overactive cognitive processes linked to anxiety and stress.
Standard neurofeedback protocols for Generalized Anxiety Disorder
- Alpha-Theta Neurofeedback: This protocol enhances the balance between alpha and theta brainwave frequencies. By increasing alpha activity (associated with relaxation) and reducing excessive theta activity (associated with rumination and overthinking), individuals may experience a calmer and more centered state of mind, reducing anxiety symptoms.
- SMR (Sensorimotor Rhythm) Neurofeedback: The SMR protocol aims to increase the SMR brainwave frequency (12-15 Hz) while decreasing higher beta frequencies. SMR neurofeedback has been associated with improved emotional stability and reduced anxiety levels.
- Alpha Neurofeedback: This protocol focuses on increasing alpha brainwave activity related to a relaxed and alert state. By enhancing alpha rhythms, individuals may experience reduced anxiety and improved stress management.
- Low-Beta Neurofeedback: This protocol targets low-beta brainwave frequencies (15-18 Hz) to promote relaxation and reduce stress and anxiety.
- Alpha-Theta-Alpha Neurofeedback: This protocol combines both alpha and theta training to achieve a more profound state of relaxation and emotional regulation.
Electrode Application Brain Region:
The electrode placement for anxiety and stress disorders neurofeedback protocol includes the frontal cortex (Fz, F3, F4) and central cortex (C3, C4). These regions are chosen because they involve emotional regulation and cognitive processing. The goal is to train the brain to achieve a balanced state of relaxation and alertness, helping individuals better cope with anxiety and stress triggers.
Placement of Electrodes:
Fz: Positioned at the midline of the forehead (frontal cortex).
F3 and F4: Positioned on the left and right sides of the forehead, respectively (frontal cortex).
C3 and C4: Positioned on the left and right sides of the head, slightly above the ears (central cortex).
During the neurofeedback session, individuals receive real-time feedback about their brainwave activity, usually through auditory or visual cues. The feedback may be in the form of calming sounds or images when the desired alpha brainwave activity increases and stress-inducing sounds or images when beta brainwave activity rises. Over time, with repeated sessions, individuals learn to self-regulate their brain activity, reducing anxiety and stress responses in real-life situations.
It’s essential to note that individual responses to neurofeedback may vary, and practitioners can adapt the protocol based on each person’s specific needs and brainwave patterns. Additionally, neurofeedback for anxiety and stress disorders is often used as part of a comprehensive treatment plan, which may include psychotherapy, relaxation techniques, and lifestyle changes. As a result, individuals may experience more effective management of their symptoms.Professional guidance from qualified healthcare providers is crucial to ensure the safe and effective use of neurofeedback for anxiety and stress management.
Home Neurofeedback for Panic Disorder
Panic disorder involves sudden and intense fear responses. Moreover, neurofeedback has been explored as an adjunctive treatment for this condition. By targeting brainwave patterns associated with heightened arousal and panic attacks, neurofeedback may help individuals achieve a calmer and more controlled state of mind. As a result, they can experience reduced panic symptoms and improved emotional regulation.
The “Beta Training” neurofeedback protocol is frequently utilized for panic disorder. This protocol aims to increase beta brainwave activity (15-18 Hz) to enhance alertness and cognitive control, thereby reducing the frequency and intensity of panic attacks.
Standard neurofeedback protocols for Panic Disorder:
- Alpha-Theta Neurofeedback: This protocol enhances the balance between alpha and theta brainwave frequencies. Alpha brainwaves are associated with a relaxed and calm state, while theta brainwaves are related to emotional processing. By increasing alpha and reducing excessive theta activity, individuals may experience reduced anxiety and panic symptoms.
- SMR (Sensorimotor Rhythm) Neurofeedback: The SMR protocol aims to increase the SMR brainwave frequency (12-15 Hz) while reducing higher beta frequencies. SMR neurofeedback has been associated with improved emotional stability and reduced anxiety levels, which may help individuals with Panic Disorder manage their panic symptoms.
- Alpha Neurofeedback: This protocol focuses on increasing alpha brainwave activity related to a relaxed and alert state. By enhancing alpha rhythms, individuals may experience reduced anxiety and improved emotional control during panic attacks.
- Z-Score Neurofeedback: Z-score neurofeedback is a more individualized approach that compares an individual’s brainwave activity to a normative database. This allows personalized training to target specific dysregulated brainwave patterns associated with Panic Disorder.
- Alpha-Theta-Alpha Neurofeedback: This protocol combines both alpha and theta training to achieve a deeper state of relaxation and emotional regulation, potentially helping individuals with Panic Disorder manage their anxiety and panic symptoms more effectively.
Electrode Application Brain Regions:
Frontal cortex (Fz, F3, F4), central cortex (C3, C4), and parietal cortex (Pz).
It’s essential to remember that neurofeedback for Panic Disorder is just one component of a comprehensive treatment plan. Other therapeutic approaches include cognitive-behavioral therapy (CBT), medication (if a qualified healthcare professional prescribes it), and lifestyle changes. Healthcare providers often recommend these options to address panic symptoms effectively. By integrating these strategies, individuals may better manage their symptoms.
Home Neurofeedback and Attention Disorders
Attention disorders, including Attention Deficit Hyperactivity Disorder (ADHD), pose significant challenges for individuals of all ages. Difficulty sustaining attention, impulsivity, and hyperactivity can interfere with academic, professional, and personal pursuits. While conventional treatments often involve medication, Home Neurofeedback offers a non-pharmacological alternative that addresses the root causes of attention disorders.
Neurofeedback is widely used as a non-pharmacological intervention for ADHD. By promoting better regulation of brain activity, especially in areas responsible for attention and impulse control, neurofeedback can improve focus and behavior in individuals with ADHD.
The neurofeedback protocol for Attention Deficit Hyperactivity Disorder (ADHD)
It aims to improve attention, focus, and impulse control in individuals with ADHD. It typically involves training individuals to increase sensorimotor rhythm (SMR) brainwave activity (12-15 Hz) while reducing theta brainwave activity (4-8 Hz). SMR brainwaves are associated with a state of calm focus. Reducing theta brainwaves can help reduce distractibility and impulsivity, which is often observed in individuals with ADHD. Below are some standard neurofeedback protocols that practitioners commonly use for ADHD:
- Beta/SMR Neurofeedback: This protocol focuses on enhancing beta brainwave activity (associated with focus and alertness) while also targeting the sensorimotor rhythm (SMR) frequency range (12-15 Hz). SMR neurofeedback improves attention and focus. By increasing beta and SMR activity, individuals with ADHD may experience improved attention and reduced hyperactivity.
- Theta/Beta Neurofeedback: This protocol aims to reduce theta brainwave activity (related to daydreaming and inattentiveness) and increase beta brainwave activity. Individuals may experience enhanced attention and cognitive control by decreasing theta and increasing beta.
- Alpha-Theta Neurofeedback: This protocol combines both alpha and theta training. It aims to increase alpha brainwave activity (associated with relaxation and calmness) while also targeting theta brainwave activity. The alpha-theta neurofeedback protocol may be beneficial for individuals with ADHD who experience both attention difficulties and anxiety.
- Slow Cortical Potential (SCP) Neurofeedback: SCP neurofeedback focuses on training slow cortical potentials, which are very slow electrical brainwave shifts. This protocol aims to improve cortical arousal and overall attention regulation.
- Z-Score Neurofeedback: Z-score neurofeedback is a more individualized approach that compares an individual’s brainwave activity to a normative database. This allows personalized training to target specific dysregulated brainwave patterns associated with ADHD.
Electrode Application Brain Region:
The electrode placement for ADHD neurofeedback protocol targets the central cortex (C3, C4), including the brain’s sensorimotor areas.
Placement of Electrodes:
C3: Positioned on the left side of the head, slightly above the left ear (central cortex).
C4: Positioned on the right side of the head, slightly above the right ear (central cortex).
During the neurofeedback session, individuals receive real-time feedback about their brainwave activity, typically through visual or auditory cues. For example, calming sounds or images may be presented when SMR brainwave activity increases and alerting cues may be given when theta brainwave activity decreases. The goal is to help individuals learn to self-regulate their brain activity, leading to improved attention and impulse control in daily life.
The neurofeedback protocol for ADHD may vary based on the individual’s specific symptoms and brainwave patterns. Other brain regions or frequencies may be targeted depending on the person’s unique needs. Additionally, neurofeedback is often used as part of a comprehensive treatment approach for ADHD.
Home Neurofeedback for Dyscalculia
Dyscalculia is a specific learning disability that affects a person’s ability to understand and work with numbers. The neurofeedback protocol for dyscalculia aims to improve numerical processing and mathematical skills by targeting brainwave activity associated with cognitive functions related to numerical processing and spatial awareness.
The neurofeedback protocol for dyscalculia
It may vary based on the individual’s unique needs and brainwave patterns. However, a common approach is to train individuals to increase beta brainwave activity (15-18 Hz) and decrease theta brainwave activity (4-8 Hz). Beta brainwaves are associated with cognitive focus and attention while reducing theta brainwaves can help improve executive functions and working memory in mathematical tasks.
Electrode Application Brain Region:
The electrode placement for the dyscalculia neurofeedback protocol typically involves targeting the frontal cortex (Fz, F3, F4) and central cortex (C3, C4). These brain regions are involved in executive functions and numerical processing.
Electrode placement sites:
Fz: Positioned at the midline of the forehead (frontal cortex).
F3 and F4: Positioned on the left and right sides of the forehead, respectively (frontal cortex).
C3 and C4: Positioned on the left and right sides of the head, slightly above the ears (central cortex).
During the neurofeedback session, individuals receive real-time feedback about their brainwave activity, typically through visual or auditory cues. For example, positive reinforcement may be given when beta brainwave activity increases during numerical tasks, and corrective cues may be presented when theta brainwave activity rises, indicating reduced attention or cognitive load.
It is important to remember that dyscalculia is a complex learning disorder. Furthermore, neurofeedback is often used as part of a comprehensive intervention plan, which may include educational support, specialized tutoring, and targeted mathematical training. In addition, professional guidance from qualified healthcare providers and educational specialists is crucial to ensure the safe and effective use of neurofeedback for dyscalculia management. Moreover, the neurofeedback protocol should be tailored to each individual’s specific learning challenges and responses to treatment.
Home Neurofeedback for Dyslexia
Dyslexia is a specific learning disability that affects reading, spelling, and writing skills. The neurofeedback protocol for dyslexia aims to improve reading and language processing by targeting brainwave activity associated with phonological awareness, attention, and language processing.
The specific neurofeedback protocol for dyslexia
It may vary based on the individual’s unique needs and brainwave patterns. However, a common approach is to train individuals to increase alpha brainwave activity (8-12 Hz) and decrease theta brainwave activity (4-8 Hz). Alpha brainwaves are associated with relaxed alertness and improved attention, while reducing theta brainwaves can help enhance cognitive focus and phonological processing in reading and language tasks.
Electrode Application Brain Region:
The electrode placement for dyslexia neurofeedback protocol typically involves targeting the frontal cortex (Fz, F3, F4) and temporal cortex (T3, T4). These brain regions involve attention, language processing, and phonological awareness.
Placement of Electrodes:
Fz: Positioned at the midline of the forehead (frontal cortex).
F3 and F4: Positioned on the left and right sides of the forehead, respectively (frontal cortex).
T3 and T4: Positioned on the left and right sides of the head, slightly above the ears (temporal cortex).
During the neurofeedback session, individuals receive real-time feedback about their brainwave activity, typically through visual or auditory cues. For example, positive reinforcement may be given when alpha brainwave activity increases during reading or language tasks, and corrective cues may be presented when theta brainwave activity rises, indicating reduced attention or phonological processing.
It is important to remember that dyslexia is a complex learning disorder. Furthermore, neurofeedback is often used as part of a comprehensive intervention plan, which may include specialized reading instruction, educational support, and targeted language training. In addition, professional guidance from qualified healthcare providers and educational specialists is crucial to ensure the safe and effective use of neurofeedback for dyslexia management. Moreover, the neurofeedback protocol should be tailored to each individual’s specific reading challenges and responses to treatment.
Home Neurofeedback and Sleep Disturbances
In today’s fast-paced world, sleep disturbances have become increasingly prevalent, affecting countless individuals’ physical and mental well-being. Insomnia, sleep apnea, and restless leg syndrome are just a few examples of sleep disorders that can significantly impact overall health and daytime functioning. For those seeking natural and non-invasive solutions, Home Neurofeedback holds considerable promise.
Neurofeedback can benefit sleep disorders, such as insomnia. Neurofeedback can improve sleep quality and help individuals fall asleep more easily by training the brain to achieve relaxed and balanced brainwave patterns.
The neurofeedback protocol for insomnia
It aims to improve sleep quality and promote relaxation by training individuals to achieve a state of calmness and reduce brainwave activity associated with wakefulness. Specifically, the protocol typically involves increasing alpha brainwave activity (8-12 Hz) and decreasing beta brainwave activity (15-18 Hz) to induce a relaxed and drowsy state. As a result, this approach promotes better sleep initiation and maintenance.
Below are some standard neurofeedback protocols used for sleep disorders:
- Alpha-Theta Neurofeedback: This protocol enhances the balance between alpha and theta brainwave frequencies. Alpha brainwaves are associated with a relaxed and drowsy state, while theta brainwaves are related to the early stages of sleep. Individuals may experience improved sleep initiation and quality by increasing alpha and theta activity.
- SMR (Sensorimotor Rhythm) Neurofeedback: The SMR protocol aims to increase the SMR brainwave frequency (12-15 Hz) while reducing higher beta frequencies. SMR neurofeedback has been associated with improved sleep patterns and reduced sleep disturbances.
- Delta Neurofeedback: This protocol targets delta brainwave frequencies (0.5-4 Hz) associated with deep sleep. Individuals may experience improved sleep depth and restorative sleep by enhancing delta activity.
- Alpha Spindles Neurofeedback: Alpha spindles are short bursts of alpha brainwave activity during non-REM sleep. This protocol aims to increase alpha spindle occurrences linked to better sleep quality and cognitive performance.
- Z-Score Neurofeedback: Z-score neurofeedback is a more individualized approach that compares an individual’s brainwave activity to a normative database. This allows personalized training to target specific dysregulated brainwave patterns related to sleep disorders.
Electrode Application Brain Region:
The electrode placement for the insomnia neurofeedback protocol includes the frontal cortex (Fz, F3, F4) and central cortex (C3, C4). These brain regions are chosen because they are involved in emotional regulation and cognitive control, essential for promoting relaxation and sleep preparation.
Placement of Electrodes:
Fz: Positioned at the midline of the forehead (frontal cortex).
F3 and F4: Positioned on the left and right sides of the forehead, respectively (frontal cortex).
C3 and C4: Positioned on the left and right sides of the head, slightly above the ears (central cortex).
During the neurofeedback session, individuals receive real-time feedback about their brainwave activity, usually through visual or auditory cues. For example, calming sounds or images may be presented when alpha brainwave activity increases and alerting cues may be given when beta brainwave activity decreases. The objective is to help individuals learn to self-regulate their brain activity, leading to a more relaxed state conducive to falling asleep and staying asleep.
It is important to note that insomnia can have various underlying causes. Neurofeedback often plays a crucial role in a comprehensive treatment approach that includes sleep hygiene practices, relaxation techniques, and addressing any underlying psychological or medical factors contributing to insomnia. Moreover, professional guidance from qualified healthcare providers is crucial to ensure the safe and effective use of neurofeedback for insomnia management. Additionally, the neurofeedback protocol should be tailored to each individual’s specific sleep patterns and responses to treatment.
Home Neurofeedback and Mood Disorders
Mood disorders, encompassing conditions like Major Depressive Disorder (MDD), Persistent Depressive Disorder (PDD) or Dysthymia, Cyclothymic Disorder, Disruptive Mood Dysregulation Disorder (DMDD), and bipolar disorder, profoundly affect emotional well-being and life satisfaction. While traditional treatments often involve medication and therapy, Home Neurofeedback presents a complementary approach to bolster emotional resilience and promote a positive outlook.
Studies exploring the efficacy of neurofeedback in mood disorders have shown encouraging outcomes. Individuals can develop greater emotional control and stability by targeting specific brainwave patterns associated with mood regulation and emotional processing. Moreover, the convenience of home neurofeedback allows individuals to integrate brain training into their daily routines. As a result, this approach may help reduce the severity and frequency of mood swings and depressive episodes.
The neurofeedback protocol for mood disorders
This protocol alleviates depressive symptoms by promoting relaxation, emotional regulation, and cognitive balance. Typically, it involves training individuals to increase alpha brainwave activity (8-12 Hz) while decreasing beta brainwave activity (15-18 Hz). Since alpha brainwaves are associated with calm and relaxation, individuals may experience improved mood and emotional stability. Reducing beta brainwaves can help reduce rumination and overactive cognitive processes, often seen in individuals with depression.
Below are some standard neurofeedback protocols used for mood disorders:
- Alpha-Theta Neurofeedback: This protocol enhances the balance between alpha and theta brainwave frequencies. Alpha brainwaves are associated with a relaxed and calm state, while theta brainwaves are related to emotional processing. Individuals may experience improved emotional regulation and mood stability by increasing alpha and reducing excessive theta activity.
- SMR (Sensorimotor Rhythm) Neurofeedback: The SMR protocol aims to increase the SMR brainwave frequency (12-15 Hz) while reducing higher beta frequencies. SMR neurofeedback has been associated with improved emotional stability and decreased anxiety levels, which can be beneficial for individuals with mood disorders.
- Alpha Neurofeedback: This protocol focuses on increasing alpha brainwave activity related to a relaxed and alert state. By enhancing alpha rhythms, individuals may experience reduced anxiety and improved mood.
- Z-Score Neurofeedback: Z-score neurofeedback is a more individualized approach that compares an individual’s brainwave activity to a normative database. This allows personalized training to target specific dysregulated brainwave patterns associated with mood disorders.
- Alpha-Theta-Alpha Neurofeedback: This protocol combines both alpha and theta training to achieve a deeper state of relaxation and emotional regulation, potentially helping individuals with mood disorders manage their emotions more effectively.
Electrode Application Brain Region:
The electrode placement for mood disorders neurofeedback protocol includes the frontal cortex (Fz, F3, F4) and central cortex (C3, C4). These regions are chosen because they involve emotional processing and cognitive control. The goal is to train the brain to achieve a balanced state of relaxation and mental flexibility, which may help reduce symptoms of depression.
Placement of Electrodes:
Fz: Positioned at the midline of the forehead (frontal cortex).
F3 and F4: Positioned on the left and right sides of the forehead, respectively (frontal cortex).
Placing electrodes at these specific sites targets brain activity in the prefrontal region, which plays a significant role in mood regulation, emotional processing, and cognitive functions associated with depressive disorders. By focusing on this area, practitioners aim to enhance the effectiveness of the neurofeedback treatment.
C3 and C4: Positioned on the left and right sides of the head, slightly above the ears (central cortex). These electrode sites are relevant because they are closer to the motor cortex and have been associated with emotional regulation and mood.
During the neurofeedback session, individuals receive real-time feedback about their brainwave activity, typically through visual or auditory cues. For example, calming sounds or images may be presented when alpha brainwave activity increases, and stress-inducing cues may be given when beta brainwave activity rises. The objective is to help individuals learn to self-regulate their brain activity, leading to reduced depressive symptoms and a more balanced emotional state.
Home Neurofeedback for Bipolar Disorder
Bipolar disorder involves mood swings between depressive and manic states. As a potential adjunctive therapy, neurofeedback has been explored for individuals with bipolar disorder. Targeting specific brainwave patterns associated with mood regulation and emotional stability may help stabilize mood swings and improve emotional resilience.
For bipolar disorder, a neurofeedback protocol called “Alpha Training” may be employed. This protocol focuses on increasing alpha brainwave activity (8-12 Hz) to promote relaxation and emotional stability, which can be beneficial in managing mood swings characteristic of bipolar disorder.
Neurofeedback protocols for bipolar disorder aim to target specific brainwave patterns associated with mood regulation and emotional processing. Neurofeedback can be used as a complementary approach to help individuals with bipolar disorder. Still, it is essential to consult with a qualified healthcare professional or neurofeedback practitioner to determine the most appropriate protocol for individual needs. It’s crucial to note that bipolar disorder is a severe and complex mental health condition. Therefore, neurofeedback should be part of a comprehensive treatment plan alongside other evidence-based therapies and medications a qualified healthcare provider prescribes. By integrating these approaches, individuals can effectively manage their symptoms.
Since bipolar disorder involves both depressive and manic episodes, neurofeedback protocols need to be carefully tailored to the individual’s current mood state and specific symptoms.
General considerations for Neurofeedback protocol in bipolar disorder
Below are some general considerations for neurofeedback protocols used for bipolar disorder:
- Alpha-Theta Neurofeedback: This protocol enhances the balance between alpha and theta brainwave frequencies. Alpha brainwaves are associated with a relaxed and calm state, while theta brainwaves are related to emotional processing. By increasing alpha and reducing excessive theta activity, individuals may experience improved emotional regulation during both depressive and manic states.
- Z-Score Neurofeedback: Z-score neurofeedback is a more individualized approach that compares an individual’s brainwave activity to a normative database. This allows for personalized training to target specific dysregulated brainwave patterns associated with bipolar disorder. This approach can be handy for addressing different brainwave patterns during depressive and manic episodes.
- Alpha-Theta-Alpha Neurofeedback: This protocol combines both alpha and theta training to achieve a deeper state of relaxation and emotional regulation. It can be beneficial for individuals with bipolar disorder, as it may help them manage emotional instability during both depressive and manic episodes.
- Bipolar-Specific Protocols: Some neurofeedback practitioners may use specialized protocols designed explicitly for individuals with bipolar disorder. These protocols may involve a combination of different brainwave frequencies and vary depending on the individual’s symptoms and mood state.
Electrode Application Brain Regions:
Frontal cortex (Fz, F3, F4), central cortex (C3, C4), and parietal cortex (Pz).
Again, it’s crucial to emphasize that neurofeedback should be used as part of a comprehensive treatment plan for bipolar disorder and should not replace standard medical care or other evidence-based therapies. If you or someone you know is dealing with bipolar disorder and considering neurofeedback, it is essential to work closely with a qualified mental health professional or neurofeedback practitioner to create a personalized and safe treatment plan. Neurofeedback should always be conducted under the guidance and supervision of a trained professional.
Home Neurofeedback for Obsessive-Compulsive Disorder (OCD)
Neurofeedback has shown promise as a supplementary treatment for OCD. By targeting brainwave patterns associated with obsessive thoughts and compulsive behaviors related to OCD, neurofeedback can help individuals gain better control over their intrusive thoughts and reduce the frequency and intensity of compulsive actions.
For OCD, a specific neurofeedback protocol known as “Theta/Beta Training” is often utilized.
This protocol encourages the individual to increase their beta brainwave activity (12-15 Hz) while decreasing theta brainwave activity (4-8 Hz). By doing so, it aims to promote cognitive flexibility and emotional regulation and reduce obsessive thought patterns, which are common in individuals with OCD, leading to symptom relief.
Neurofeedback protocols for OCD:
- Alpha-Theta Neurofeedback: This protocol enhances the balance between alpha and theta brainwave frequencies. Alpha brainwaves are associated with a relaxed and calm state, while theta brainwaves are related to emotional processing. By increasing alpha and reducing excessive theta activity, individuals may experience improved emotional regulation and reduced anxiety related to obsessive thoughts.
- Alpha Neurofeedback: This protocol focuses on increasing alpha brainwave activity related to a relaxed and alert state. By enhancing alpha rhythms, individuals may experience reduced anxiety and improved emotional control, potentially helping to manage OCD symptoms.
- SMR (Sensorimotor Rhythm) Neurofeedback: The SMR protocol aims to increase the SMR brainwave frequency (12-15 Hz) while reducing higher beta frequencies. SMR neurofeedback has been associated with improved emotional stability and decreased anxiety levels, which can be beneficial for individuals with OCD.
- Z-Score Neurofeedback: Z-score neurofeedback is a more individualized approach that compares an individual’s brainwave activity to a normative database. This allows for personalized training to target specific dysregulated brainwave patterns associated with OCD.
- Alpha-Theta-Alpha Neurofeedback: This protocol combines both alpha and theta training to achieve a deeper state of relaxation and emotional regulation, potentially helping individuals with OCD manage their anxiety and obsessive thoughts.
Electrode Application Brain Regions:
Frontal cortex (Fz, F3, F4), central cortex (C3, C4), and parietal cortex (Pz).
It’s essential to remember that neurofeedback for OCD is just one component of a comprehensive treatment plan.
Other therapeutic approaches, including cognitive-behavioral therapy (CBT), exposure and response prevention (ERP), medication (when prescribed by a qualified healthcare professional), and lifestyle changes, may also enhance the effective management of OCD symptoms.
Home Neurofeedback for Chronic Pain
Neurofeedback has been explored as a complementary approach for managing chronic pain conditions. By altering pain perception and modulating brain responses to pain signals, it may contribute to pain relief and increased pain tolerance.
Neurofeedback protocols for chronic pain aim to target specific brainwave patterns associated with pain perception and pain modulation. Neurofeedback can be used as a complementary approach to help individuals with chronic pain conditions. It is essential to note that neurofeedback for chronic pain should be part of a comprehensive pain management plan, which may include other medical treatments, physical therapy, and lifestyle changes.
The neurofeedback protocol for chronic pain aims to reduce pain perception and improve pain management by targeting brainwave activity associated with pain processing and emotional regulation. This protocol typically involves training individuals to increase sensorimotor rhythm (SMR) brainwave activity (12-15 Hz) and decrease theta brainwave activity (4-8 Hz). SMR brainwaves are associated with a state of calm focus while reducing theta brainwaves can help reduce pain perception and emotional distress related to chronic pain.
Neurofeedback protocols for chronic pain:
- Alpha-Theta Neurofeedback: This protocol enhances the balance between alpha and theta brainwave frequencies. Alpha brainwaves are associated with relaxation and pain relief, while theta brainwaves are related to emotional processing. Individuals may experience pain relief and improved emotional well-being by increasing alpha and reducing excessive theta activity.
- SMR (Sensorimotor Rhythm) Neurofeedback: The SMR protocol aims to increase the SMR brainwave frequency (12-15 Hz) while reducing higher beta frequencies. SMR neurofeedback has been associated with improved pain modulation and pain management.
- Beta Neurofeedback: This protocol focuses on increasing beta brainwave activity related to alertness and cognitive function. By enhancing beta rhythms, individuals may experience increased pain tolerance and improved cognitive coping with chronic pain.
- Z-Score Neurofeedback: Z-score neurofeedback is a more individualized approach that compares an individual’s brainwave activity to a normative database. This allows personalized training to target specific dysregulated brainwave patterns associated with chronic pain.
- Connectivity Neurofeedback: This protocol focuses on training specific brain regions or brainwave connectivity patterns associated with pain modulation and processing.
Electrode Application Brain Region:
The electrode placement for chronic pain neurofeedback protocol targets the central cortex (C3, C4), including the brain’s sensorimotor areas.
Placement of Electrodes:
C3: Positioned on the left side of the head, slightly above the left ear (central cortex).
C4: Positioned on the right side of the head, slightly above the right ear (central cortex).
During the neurofeedback session, individuals receive real-time feedback about their brainwave activity, typically through visual or auditory cues. For example, calming sounds or images may be presented when SMR brainwave activity increases, and stress-inducing cues may be given when theta brainwave activity decreases. The goal is to help individuals self-regulate their brain activity, reduce pain perception, and improve pain management.
It is essential to remember that chronic pain is a complex condition. Neurofeedback is often used as part of a comprehensive pain management plan, which may include other pain-relief techniques.
Home Neurofeedback for Migraine Disorders
Stress and emotional factors often trigger or exacerbate migraines. Neurofeedback has been investigated as a non-pharmacological intervention for migraines. Neurofeedback may reduce migraine frequency and intensity by targeting brainwave patterns linked to pain processing and cortical excitability.
The neurofeedback protocol commonly used for migraines is “Alpha-Theta Training.” This protocol aims to promote relaxation, reduce stress, and alleviate migraine-related symptoms by guiding individuals to increase alpha and theta brainwave activity. The Alpha-Theta protocol seeks to reduce migraine frequency and intensity by directing individuals to achieve a state of deep relaxation through increased alpha and theta brainwave activity.
Neurofeedback protocols for migraine
- Alpha-Theta Neurofeedback: This protocol enhances the balance between alpha and theta brainwave frequencies. Alpha brainwaves are associated with a relaxed and calm state, while theta brainwaves are related to emotional processing. By increasing alpha and reducing excessive theta activity, individuals may experience reduced stress and anxiety, which can trigger migraines.
- Beta Neurofeedback: This protocol targets beta brainwave frequencies (15-18 Hz) associated with alertness and focus. By enhancing beta activity, individuals may experience improved cognitive function and reduced sensitivity to migraine triggers.
- Slow Cortical Potential (SCP) Neurofeedback: SCP neurofeedback focuses on training slow cortical potentials, which are very slow electrical brainwave shifts. This protocol aims to improve cortical arousal and overall brain regulation, potentially reducing the frequency and intensity of migraines.
- Z-Score Neurofeedback: Z-score neurofeedback is a more individualized approach that compares an individual’s brainwave activity to a normative database. This allows personalized training to target specific dysregulated brainwave patterns associated with migraines.
5. Temperature Training—Temperature Biofeedback: In addition to brainwave training, some neurofeedback protocols may also incorporate temperature training. This involves biofeedback of skin temperature, as changes in peripheral blood flow have been associated with migraines. By learning to regulate skin temperature, individuals may gain more control over migraine triggers.
Electrode Application Brain Regions:
Occipital cortex (Oz), temporal cortex (T3, T4), and parietal cortex (Pz).
It’s important to remember that neurofeedback for migraine disorders is just one component of a comprehensive treatment plan. Other interventions, such as medication (if prescribed by a qualified healthcare professional), lifestyle modifications, and identifying and avoiding migraine triggers, may also be recommended to manage migraines effectively.
Home Neurofeedback for Fibromyalgia
Fibromyalgia is associated with chronic pain and sensitization of the nervous system. Neurofeedback has been studied as a complementary approach to fibromyalgia management. Modulating brainwave patterns associated with pain perception and stress responses may contribute to pain relief and enhanced coping mechanisms.
If neurofeedback is considered part of a comprehensive treatment plan for fibromyalgia, a qualified neurofeedback practitioner may design individualized protocols based on the person’s specific symptoms and brainwave patterns. The goal may be to target brainwave frequencies associated with pain perception, stress, relaxation, and sleep to improve pain management, stress reduction, and overall well-being.
In cases of fibromyalgia, a neurofeedback protocol known as “SMR (Sensorimotor Rhythm) Training” is often applied. By increasing SMR brainwave activity (12-15 Hz), this protocol aims to reduce pain perception and improve the overall management of fibromyalgia symptoms.
Electrode Application Brain Regions:
- Central cortex (C3, C4),
- parietal cortex (Pz), and
- occipital cortex (Oz).
It’s important to understand that fibromyalgia is a complex condition with multiple contributing factors, and there is no one-size-fits-all approach to its management. In addition to neurofeedback, a comprehensive treatment plan for fibromyalgia may include other interventions such as medication (if prescribed by a healthcare professional), physical therapy, exercise, cognitive-behavioral therapy (CBT), and lifestyle changes.
Home Neurofeedback for Traumatic Brain Injury (TBI)
TBI often results in disrupted brain functioning, affecting cognitive abilities. Neurofeedback has been explored as part of neurorehabilitation programs for individuals recovering from traumatic brain injuries. EEG biofeedback may enhance mental functions and aid in rehabilitation by promoting brainwave patterns that aid in cognitive recovery and neural regeneration.
Neurofeedback can be part of a comprehensive rehabilitation approach to help individuals with TBI manage symptoms and support brain healing. As with any medical treatment, it is crucial to consult with a qualified healthcare professional or neurofeedback practitioner experienced in TBI to determine the most appropriate protocol for individual needs.
In cases of TBI, the “SCP (Slow Cortical Potential) Training” neurofeedback protocol is frequently employed. This protocol trains individuals to self-regulate their cortical excitability by producing slow cortical potential shifts. The goal is to facilitate neuroplasticity and promote brain healing and cognitive recovery.
Neurofeedback protocols for Traumatic Brain Injury
- Connectivity Training: This protocol enhances communication and connectivity between brain regions. It aims to improve neural network functioning and coordination, which may help cognitive and motor function after TBI.
- Symmetry Training: This protocol balances brainwave activity between the left and right hemispheres. After TBI, brain function can be imbalanced, and symmetry training seeks to restore equilibrium.
- SMR (Sensorimotor Rhythm) Neurofeedback: The SMR protocol aims to increase the SMR brainwave frequency (12-15 Hz) while reducing higher beta frequencies. SMR neurofeedback has been associated with improved cognitive function and motor skills, which can benefit individuals with TBI.
- Alpha-Theta Neurofeedback: This protocol combines both alpha and theta training to achieve a state of relaxation and emotional regulation. It may help with stress reduction and emotional healing, which can be valuable during the recovery process after TBI.
- Slow Cortical Potential (SCP) Neurofeedback: SCP neurofeedback focuses on training slow cortical potentials, which are very slow electrical brainwave shifts. This protocol aims to improve cortical arousal and overall brain function after TBI.
- Z-Score Neurofeedback: Z-score neurofeedback is a more individualized approach that compares an individual’s brainwave activity to a normative database. This allows for personalized training to target specific dysregulated brainwave patterns associated with TBI.
Electrode Application Brain Regions:
- Frontal cortex (Fz, F3, F4),
- central cortex (C3, C4),
- and parietal cortex (Pz).
The neurofeedback protocols used for TBI may vary based on the severity of the injury, the specific cognitive and motor deficits, and the individual’s response to treatment. Neurofeedback for TBI is often used in conjunction with other therapies, such as physical therapy, occupational therapy, speech therapy, and cognitive rehabilitation, to support the overall recovery process.
Home Neurofeedback for Substance Use Disorders (SUD)
Substance use disorders are often associated with imbalances in emotional regulation and impulsivity. Neurofeedback has been utilized in addiction treatment programs. By training individuals to achieve more stable brainwave patterns, particularly in regions involved in impulse control and reward processing, neurofeedback can help reduce cravings and improve self-regulation in those with substance use disorders.
Neurofeedback protocols for Substance Use Disorders (SUD) aim to target specific brainwave patterns and neurophysiological dysregulation associated with addiction and substance abuse. Neurofeedback can be used as a complementary approach to help individuals with SUD by promoting self-regulation and addressing underlying neurological factors that contribute to addictive behaviors.
For substance use disorders, the “Alpha-Theta Training” neurofeedback protocol is often applied. This protocol involves guiding individuals to achieve a state of deep relaxation and heightened awareness by increasing both alpha (8-12 Hz) and theta (4-8 Hz) brainwave activity. The aim is to address underlying emotional imbalances and support addiction recovery.
Neurofeedback protocols for Substance Use Disorders
- Alpha-Theta Neurofeedback: This protocol enhances the balance between alpha and theta brainwave frequencies. Alpha brainwaves are associated with a relaxed and calm state, while theta brainwaves are related to emotional processing. By increasing alpha and reducing excessive theta activity, individuals may experience improved emotional regulation and stress reduction, which can be beneficial in managing cravings and triggers associated with substance use.
- SMR (Sensorimotor Rhythm) Neurofeedback: The SMR protocol aims to increase the SMR brainwave frequency (12-15 Hz) while reducing higher beta frequencies. SMR neurofeedback has been associated with improved emotional stability and decreased anxiety levels, which can help individuals with SUD manage emotional triggers that may lead to substance use.
- Theta Suppression: This protocol trains individuals to suppress excessive theta brainwave activity, which may be linked to impulsivity and emotional dysregulation commonly observed in SUD.
- Z-Score Neurofeedback: Z-score neurofeedback is a more individualized approach that compares an individual’s brainwave activity to a normative database. This allows personalized training to target specific dysregulated brainwave patterns associated with SUD.
- Alpha-Theta-Alpha Neurofeedback: This protocol combines alpha and theta training to achieve a deeper state of relaxation and emotional regulation. It could potentially help individuals with SUD manage emotional distress and enhance self-regulation skills.
Electrode Application Brain Regions:
Frontal cortex (Fz, F3, F4), central cortex (C3, C4), and parietal cortex (Pz).
It’s important to note that neurofeedback for Substance Use Disorders is often used as part of a comprehensive treatment plan that may include other interventions, such as counseling, behavioral therapies, support groups, and medical treatments. Neurofeedback can be a valuable tool in addressing neurophysiological aspects of addiction and supporting individuals in their recovery journey.
Home Neurofeedback for Autistic Spectrum Disorder (ASD)
Difficulties in social interaction and communication characterize ASD. While not a primary treatment, neurofeedback has been studied as a complementary therapy for individuals with ASD. By focusing on brainwave patterns associated with social cognition and emotional regulation, neurofeedback may assist in improving social interaction and communication skills.
Neurofeedback protocols for ASD may vary depending on an individual’s specific symptoms. However, a common approach involves “Sensorimotor Rhythm (SMR) Training.” By encouraging individuals to enhance their SMR brainwave frequency (12-15 Hz), this protocol aims to improve attention, focus, and motor skills in individuals with ASD.
Neurofeedback protocols for ASD:
- Sensorimotor Rhythm (SMR) Neurofeedback: The SMR protocol aims to increase the SMR brainwave frequency (12-15 Hz) while reducing higher beta frequencies. SMR neurofeedback may promote focus, attention, and motor control in individuals with ASD.
- Theta/Beta Neurofeedback: This protocol aims to reduce theta brainwave activity (related to daydreaming and inattentiveness) and increase beta brainwave activity. By decreasing theta and increasing beta, individuals with ASD may experience enhanced attention and cognitive control.
- Alpha-Theta Neurofeedback: This protocol combines both alpha and theta training. It aims to increase alpha brainwave activity (associated with relaxation and calmness) while also targeting theta brainwave activity. The alpha-theta neurofeedback protocol may be beneficial for individuals with ASD who experience both attention difficulties and anxiety.
- Z-Score Neurofeedback: Z-score neurofeedback is a more individualized approach that compares an individual’s brainwave activity to a normative database. This allows personalized training to target specific dysregulated brainwave patterns associated with ASD.
- Connectivity-Guided Neurofeedback: This protocol focuses on enhancing the connectivity and coordination between different brain regions in individuals with ASD. It aims to promote better communication within the brain networks associated with social interaction and cognitive processing.
Electrode Application Brain Regions: Central cortex (C3, C4), parietal cortex (Pz), and occipital cortex (Oz).
Neurofeedback for ASD is often used as part of a comprehensive treatment plan that may include other interventions, such as behavioral therapies, speech and language therapy, occupational therapy, and educational support.
Home Neurofeedback for Borderline Personality Disorder (BPD)
BPD is characterized by emotional instability and impulsive behaviors. While not a primary treatment, neurofeedback has been investigated as a potential adjunctive therapy for BPD. By focusing on brainwave patterns linked to emotional regulation and impulsivity, neurofeedback may assist in reducing emotional instability and impulsive behaviors.
The “Theta/Beta Training” neurofeedback protocol may be implemented for BPD. This protocol encourages individuals to increase beta brainwave activity (12-15 Hz) while decreasing theta brainwave activity (4-8 Hz) to support emotional regulation and reduce impulsivity.
Neurofeedback protocols that may be used in conjunction with other therapeutic interventions for individuals with BPD
- Alpha-Theta Neurofeedback: This protocol enhances the balance between alpha and theta brainwave frequencies. Alpha brainwaves are associated with a relaxed and calm state, while theta brainwaves are related to emotional processing. By increasing alpha and reducing excessive theta activity, individuals with BPD may experience improved emotional regulation and reduced emotional reactivity.
- SMR (Sensorimotor Rhythm) Neurofeedback: The SMR protocol aims to increase the SMR brainwave frequency (12-15 Hz) while reducing higher beta frequencies. SMR neurofeedback has been shown to promote emotional stability and reduce anxiety, which may be beneficial for individuals with BPD who experience emotional dysregulation and intense mood swings.
- Alpha Neurofeedback: This protocol focuses on increasing alpha brainwave activity related to a relaxed and focused state. By enhancing alpha rhythms, individuals may experience improved emotional control and a sense of inner calm.
- Low-Beta Neurofeedback: Low-beta brainwave frequencies (15-18 Hz) are targeted in this protocol to promote relaxation and reduce stress and anxiety, which can be helpful for individuals with BPD who often experience intense emotional distress.
- Z-Score Neurofeedback: Z-score neurofeedback is a more individualized approach that compares an individual’s brainwave activity to a normative database. This allows for personalized training to target specific dysregulated brainwave patterns associated with BPD symptoms.
Electrode Application Brain Regions: Frontal cortex (Fz, F3, F4), central cortex (C3, C4), and parietal cortex (Pz).
It’s essential to emphasize that neurofeedback for Borderline Personality Disorder should be integrated into a comprehensive treatment plan that includes psychotherapy, medication (if prescribed by a qualified healthcare professional), and other evidence-based interventions. Neurofeedback can be a helpful adjunct to traditional therapies, but it should not replace essential treatments for BPD.
Home Neurofeedback for Eating Disorders
Eating disorders can also be referred to as “feeding disorders” or “eating and feeding disorders” in specific contexts. These terms describe a group of mental health conditions that involve disturbances in eating habits and behaviors. While “eating disorders” is the commonly used term, “feeding disorders” is sometimes used in a medical context when referring to eating difficulties in infants and young children that may be related to problems with food intake or swallowing.
Here are the main types of eating disorders and their alternative names:
- Anorexia Nervosa: Also known as anorexia or restrictive eating disorder.
- Bulimia Nervosa: Sometimes referred to as bulimia or binge-purge disorder.
- Binge Eating Disorder (BED): Often called binge eating or compulsive overeating.
- Avoidant/Restrictive Food Intake Disorder (ARFID): Previously known as selective eating disorder or feeding disorder of infancy or early childhood.
- Other Specified Feeding or Eating Disorder (OSFED): Also called atypical eating disorder or eating disorder not otherwise specified (EDNOS).
The specific neurofeedback protocols used for eating disorders may vary depending on the individual’s symptoms and underlying issues.
Neurofeedback protocols that may be applied in the context of eating disorders
- Alpha-Theta Neurofeedback: This protocol enhances the balance between alpha and theta brainwave frequencies. By increasing alpha (associated with relaxation) and reducing excessive theta activity (related to emotional processing and rumination), individuals with eating disorders may experience improved emotional regulation and decreased anxiety, which can be beneficial in managing disordered eating behaviors.
- SMR (Sensorimotor Rhythm) Neurofeedback: SMR training focuses on increasing the SMR brainwave frequency (12-15 Hz) while reducing higher beta frequencies. SMR neurofeedback has been associated with improved emotional stability and decreased anxiety, which may be helpful for individuals struggling with emotional dysregulation and stress-related eating patterns.
- Alpha Neurofeedback: This protocol targets enhancing alpha brainwave activity linked to a relaxed and alert state. By promoting a state of calmness and reducing hyperarousal, alpha neurofeedback may help individuals with eating disorders cope with triggers and emotional challenges associated with their condition.
- Low-Beta Neurofeedback: This protocol focuses on low-beta brainwave frequencies (15-18 Hz) to promote relaxation and reduce stress and anxiety. This can be beneficial for individuals with eating disorders who experience heightened anxiety and tension.
- Alpha-Theta-Alpha Neurofeedback: Combining alpha and theta training, this protocol aims to achieve a deeper state of relaxation and emotional regulation, which may assist individuals in managing emotional triggers and disordered eating behaviors.
It’s essential to emphasize that neurofeedback should only be used as part of a comprehensive treatment plan for eating disorders, which may include psychotherapy, nutritional counseling, medical support, and other evidence-based interventions.
Anorexia Nervosa
Anorexia nervosa is characterized by distorted body image and restrictive eating behaviors. The primary treatment approach for Anorexia Nervosa typically involves a multidisciplinary approach, including medical, psychological, and nutritional interventions. Psychotherapy, particularly cognitive-behavioral therapy (CBT) and family-based therapy (FBT) is commonly used to address the underlying psychological and behavioral aspects of the disorder.
Neurofeedback is a technique that aims to train individuals to self-regulate their brainwave patterns, and it has been used in various mental health conditions. However, its role in the treatment of Anorexia Nervosa is not well-established, and research on its effectiveness for this specific eating disorder is limited.
The Alpha-Theta protocol aims to address emotional imbalances and support emotional regulation by guiding individuals to achieve a state of deep relaxation through increased alpha and theta brainwave activity.
Neurofeedback Protocol: “Alpha-Theta Training”
Electrode Application Brain Regions: Frontal cortex (Fz, F3, F4), central cortex (C3, C4), and parietal cortex (Pz).
Bulimia Nervosa
Bulimia Nervosa is a complex eating disorder characterized by recurrent episodes of binge eating followed by compensatory behaviors such as self-induced vomiting, excessive exercise, or the misuse of laxatives. It is essential to understand that neurofeedback is not a standalone or first-line treatment for eating disorders like Bulimia Nervosa, and it should always be used as part of a comprehensive treatment plan.
While there may not be standardized neurofeedback protocols tailored explicitly for Bulimia Nervosa, neurofeedback can be incorporated as a part of an integrative treatment approach for individuals with eating disorders. The primary goal of neurofeedback in this context would be to address underlying emotional dysregulation, anxiety, and stress, which may contribute to disordered eating behaviors.
Neurofeedback protocols that might be considered as part of a comprehensive treatment plan for individuals with Bulimia Nervosa
- Emotion Regulation Training: Neurofeedback protocols that focus on increasing alpha brainwave activity, which is associated with relaxation and emotional regulation, may benefit individuals with Bulimia Nervosa by helping them manage emotional dysregulation and anxiety.
- Anxiety Reduction: Targeting beta and SMR (Sensorimotor Rhythm) brainwave frequencies may help reduce anxiety levels, which can be a common feature in eating disorders.
- Self-Regulation: Neurofeedback can enhance self-regulation skills, assisting individuals in managing impulses and developing coping strategies for stressful situations.
The Alpha protocol aims to enhance relaxation and emotional balance by increasing alpha brainwave activity (8-12 Hz).
Neurofeedback Protocol: “Alpha Training”
Electrode Application Brain Regions: Frontal cortex (Fz, F3, F4), central cortex (C3, C4), and parietal cortex (Pz).
Home Neurofeedback for Tinnitus
Tinnitus is the perception of noise or ringing in the ears when no external sound is present. It can be a challenging condition to manage, and while neurofeedback may not cure tinnitus, it may help some individuals find relief and improve their quality of life.
Neurofeedback has been studied as a noninvasive treatment for tinnitus, a condition characterized by persistent ringing in the ears. By targeting brainwave patterns linked to auditory processing and relaxation, neurofeedback may help individuals manage tinnitus-related distress.
In cases of tinnitus, the “Alpha-Theta Training” neurofeedback protocol is commonly used. This protocol aims to alleviate the distress associated with tinnitus by guiding individuals to achieve a state of deep relaxation and heightened awareness through increased alpha and theta brainwave activity.
Neurofeedback protocols for tinnitus:
- Alpha-Theta Neurofeedback: This protocol enhances the balance between alpha and theta brainwave frequencies. Alpha brainwaves are associated with relaxation and a calm state of mind, while theta brainwaves are linked to deep relaxation and a meditative state. By increasing alpha and theta activity, individuals with tinnitus may experience reduced stress and improved emotional coping, which can help decrease the perception of tinnitus sounds.
- Alpha Neurofeedback: This protocol specifically targets alpha brainwave activity to increase alpha frequencies. This can promote relaxation and reduce the emotional distress associated with tinnitus.
- Z-Score Neurofeedback: Z-score neurofeedback is a more individualized approach that compares an individual’s brainwave activity to a normative database. This allows personalized training to target specific dysregulated brainwave patterns related to tinnitus.
- Neurofeedback for Auditory Cortex Training: Some neurofeedback protocols specifically target the auditory cortex, the part of the brain responsible for processing sound. Feedback related to auditory brainwave activity aims to retrain the brain’s response to tinnitus sounds and reduce their impact.
- Tinnitus Pitch-Matching Neurofeedback: This protocol involves matching the pitch of the tinnitus sound and providing real-time feedback to the individual. The goal is to help the brain habituate to the tinnitus sound, making it less noticeable and bothersome over time.
Electrode Application Brain Regions: Temporal cortex (T3, T4), parietal cortex (Pz), and occipital cortex (Oz).
It’s important to note that neurofeedback for tinnitus may not work for everyone, and individual responses to the treatment can vary. Additionally, neurofeedback should be considered part of a comprehensive treatment plan for tinnitus, including other interventions, such as sound therapy, cognitive-behavioral therapy, and lifestyle changes.
Home Neurofeedback for Specific Phobias
Specific phobias involve intense fear responses to specific triggers.
Neurofeedback protocols for specific phobias aim to address the brainwave patterns and physiological responses associated with fear and anxiety related to the specific phobia. EEG Biofeedback can be used as a complementary approach to help individuals with specific phobias, such as fear of heights, flying, spiders, or public speaking.
Neurofeedback has been explored as a supplementary therapy for specific phobias. By targeting brainwave patterns associated with fear responses, neurofeedback may aid in desensitization and reduce the intensity of phobic reactions.
The “Alpha-Theta Training” neurofeedback protocol may be employed for specific phobias. By encouraging individuals to enter a state of deep relaxation and increased receptivity through alpha and theta brainwave activity, this protocol aims to facilitate desensitization and reduce the intensity of phobic reactions.
Neurofeedback protocols for specific phobias
- Alpha-Theta Neurofeedback: This protocol enhances the balance between alpha and theta brainwave frequencies. Alpha brainwaves are associated with relaxation and calmness, while theta brainwaves are related to a dream-like state. By increasing alpha and theta activity, individuals may experience reduced anxiety and improved emotional regulation when facing a phobic stimulus.
- SMR (Sensorimotor Rhythm) Neurofeedback: The SMR protocol aims to increase the SMR brainwave frequency (12-15 Hz) while reducing higher beta frequencies. SMR neurofeedback has been associated with reduced anxiety levels and improved emotional stability, making it beneficial for individuals with specific phobias.
- Z-Score Neurofeedback: Z-score neurofeedback is a more individualized approach that compares an individual’s brainwave activity to a normative database. This allows personalized training to target specific dysregulated brainwave patterns related to a phobia.
- Heart Rate Variability (HRV) Biofeedback: While not a direct neurofeedback protocol, HRV biofeedback is often used with neurofeedback for specific phobias. HRV biofeedback focuses on enhancing heart rate variability, which can help regulate the autonomic nervous system’s response to stress and anxiety.
- Alpha Spindles Neurofeedback: Alpha spindles are short bursts of alpha brainwave activity during non-REM sleep. This protocol aims to increase alpha spindle occurrences, which are linked to relaxation and emotional regulation. This could potentially assist individuals in managing their anxiety during phobic situations.
Electrode Application Brain Regions: Frontal cortex (Fz, F3, F4), central cortex (C3, C4), and parietal cortex (Pz).
It’s important to note that neurofeedback for a specific phobia is part of a comprehensive treatment plan that may include other interventions, such as exposure therapy, cognitive-behavioral therapy (CBT), and desensitization techniques.
Home Neurofeedback for Schizophrenia
Schizophrenia involves cognitive deficits and sensory processing difficulties. Schizophrenia is a chronic and debilitating condition that requires comprehensive treatment approaches, including medication, therapy, and psychosocial support. As a complementary approach, neurofeedback has been investigated for individuals with schizophrenia. By targeting brainwave patterns related to cognitive function and sensory integration, neurofeedback may assist in enhancing cognitive abilities and sensory processing/ integration.
Neurofeedback protocols for schizophrenia would be highly individualized and may target specific brainwave patterns or brain regions associated with cognitive and emotional dysregulation. Some researchers have explored protocols aimed at enhancing connectivity between brain regions or reducing excessive delta and theta activity, which can be present in individuals with schizophrenia.
In cases of schizophrenia, a neurofeedback protocol known as “SCP (Slow Cortical Potential) Training” may be utilized. This protocol focuses on training individuals to regulate their cortical excitability by producing slow cortical potential shifts, which can support cognitive functioning and sensory integration. SCP neurofeedback is a type of neurofeedback training that targets slow electrical brainwave shifts in the cortical regions of the brain. The goal is to improve cortical arousal and self-regulation, which may have potential implications for cognitive and emotional functioning, including symptoms related to schizophrenia.
Electrode Application Brain Regions: Frontal cortex (Fz, F3, F4), central cortex (C3, C4), and parietal cortex (Pz).
Some studies have explored using SCP neurofeedback as an adjunctive treatment for schizophrenia, but researchers have found the results limited and mixed. Some studies have reported positive effects on cognitive functioning, attention, and symptom reduction, while others have not found significant improvements.
Home Neurofeedback for Chronic Fatigue Syndrome (CFS)
Chronic Fatigue Syndrome (CFS), also known as myalgic encephalomyelitis (ME), is a long-term condition with a wide range of symptoms. The most common symptom is extreme tiredness. ME/CFS can affect anyone, including children. CFS is characterized by extreme fatigue and cognitive difficulties. Neurofeedback has been studied as a potential adjunctive therapy for CFS. By focusing on brainwave patterns associated with energy regulation and cognitive functioning, neurofeedback may contribute to symptom relief and improved mental clarity.
A neurofeedback protocol called “Alpha Training” may be employed for CFS. By increasing alpha brainwave activity (8-12 Hz), this protocol aims to enhance relaxation and cognitive clarity, which can be beneficial in managing CFS-related symptoms.
General neurofeedback approach for CFS
While there isn’t a standardized neurofeedback protocol for CFS/ME, some general approaches might be considered:
- Practitioners commonly use Alpha-Theta Neurofeedback to promote relaxation and reduce stress and anxiety. Because CFS/ME involves fatigue and often includes anxiety symptoms, they can consider this protocol to help individuals manage their stress response effectively.
- SMR (Sensorimotor Rhythm) Neurofeedback: SMR neurofeedback has improved attention and focus. Since cognitive symptoms are prevalent in CFS/ME, SMR neurofeedback may help individuals enhance their mental abilities.
- Low-Beta Neurofeedback: Low-beta training may help with cognitive functions and emotional regulation, which can benefit individuals with CFS/ME who experience brain fog and mood disturbances.
- Heart Rate Variability (HRV) Training: While not strictly neurofeedback, HRV biofeedback focuses on increasing heart rate variability, which can positively influence the autonomic nervous system and stress response. This technique may help individuals with CFS/ME manage symptoms related to autonomic dysfunction.
Electrode Application Brain Regions: Frontal cortex (Fz, F3, F4), central cortex (C3, C4), and parietal cortex (Pz).
It’s essential to note that individual responses to neurofeedback may vary, and the optimal protocol for CFS/ME may depend on the person’s unique symptoms and neurophysiological characteristics. Neurofeedback practitioners typically conduct an individualized assessment and design a personalized treatment plan based on each client’s specific needs.
It’s important to emphasize that neurofeedback should not be considered a standalone treatment for CFS/ME. CFS/ME is a complex and multifaceted condition that requires a comprehensive and multidisciplinary approach. Qualified healthcare professionals experienced in managing CFS/ME should work with individuals to explore evidence-based treatments tailored to their specific needs.
Home Neurofeedback for Irritable Bowel Syndrome (IBS)
Stress and emotional factors often influence IBS, and researchers have explored neurofeedback as part of integrative therapies for managing it. By targeting brainwave patterns associated with stress and gastrointestinal regulation, neurofeedback may help reduce the severity of IBS symptoms and enhance coping mechanisms.
The neurofeedback protocol commonly used for IBS is “Theta/Beta Training.” This protocol encourages individuals to increase beta brainwave activity (12-15 Hz) while decreasing theta brainwave activity (4-8 Hz), aiming to reduce stress and promote gastrointestinal regulation to alleviate IBS symptoms.
Neurofeedback protocols for IBS
- Alpha-Theta Neurofeedback: This protocol enhances the balance between alpha and theta brainwave frequencies. Alpha brainwaves are associated with a relaxed state, while theta brainwaves are related to emotional processing. By increasing alpha and reducing excessive theta activity, individuals with IBS may experience reduced stress and anxiety, which can help manage IBS symptoms.
- Heart Rate Variability (HRV) Biofeedback: HRV biofeedback focuses on training individuals to regulate their heart rate variability, which measures the variation in time between heartbeats. Improving HRV can promote relaxation and reduce stress, potentially benefiting individuals with IBS.
- Slow Cortical Potential (SCP) Neurofeedback: SCP neurofeedback targets slow cortical potentials, which are very slow electrical brainwave shifts. This protocol aims to improve cortical arousal and emotional regulation, which may help individuals manage stress-related IBS symptoms.
- Z-Score Neurofeedback: Z-score neurofeedback is a more individualized approach that compares an individual’s brainwave activity to a normative database. This allows personalized training to target specific dysregulated brainwave patterns associated with stress and emotional dysregulation in IBS.
Electrode Application Brain Regions: Central cortex (C3, C4), parietal cortex (Pz), and occipital cortex (Oz).
The specific neurofeedback protocol used for IBS may vary based on individual needs and the practitioner’s approach. Additionally, to achieve comprehensive symptom relief, other aspects of IBS management, such as dietary modifications, lifestyle changes, and medical treatments, must be addressed.
Home Neurofeedback for Post-Traumatic Stress Disorder (PTSD)
PTSD is often characterized by hyperarousal and flashbacks. The neurofeedback protocol for Post-Traumatic Stress Disorder (PTSD) aims to address the specific brainwave patterns and physiological responses associated with trauma and stress. Neurofeedback for PTSD is a complementary therapeutic approach.
The Theta/Beta neurofeedback protocol in PTSD aims to reduce hyperarousal and promote emotional regulation by encouraging individuals to increase beta brainwave activity (12-15 Hz) while decreasing theta brainwave activity (4-8 Hz).
Neurofeedback protocols for PTSD
- Alpha-Theta Neurofeedback: This protocol trains alpha and theta brainwave frequencies. Alpha brainwaves are associated with a relaxed and calm state, while theta brainwaves are related to deep relaxation and emotional processing. Alpha-theta neurofeedback may help individuals with PTSD by promoting relaxation and emotional regulation, reducing hyperarousal and anxiety.
- Heart Rate Variability (HRV) Biofeedback: HRV biofeedback is a form of neurofeedback that focuses on regulating heart rate variability, which is the variation in time between successive heartbeats. PTSD often disrupts autonomic nervous system activity, but HRV biofeedback can help individuals restore a more balanced and adaptive autonomic response.
- Slow Cortical Potential (SCP) Neurofeedback: SCP neurofeedback trains slow cortical potentials, which are very slow electrical brainwave shifts. This protocol aims to improve cortical arousal and attention regulation in individuals with PTSD.
- Z-Score Neurofeedback: Z-score neurofeedback is an individualized approach that compares an individual’s brainwave activity to a normative database. It allows for personalized training to target specific dysregulated brainwave patterns associated with PTSD.
- Respiration-Biofeedback: This protocol focuses on regulating respiration patterns, which can help individuals with PTSD manage stress and anxiety and improve emotional regulation.
Electrode Application Brain Regions: Frontal cortex (Fz, F3, F4), central cortex (C3, C4), and parietal cortex (Pz).
Neurofeedback for PTSD is often part of a comprehensive treatment plan that may include other interventions, such as trauma-focused therapies (e.g., cognitive-behavioral therapy), eye movement desensitization and reprocessing (EMDR), and medication (if prescribed by a qualified healthcare professional).
Home Neurofeedback for Parkinson’s Disease
Movement difficulties and tremors characterize Parkinson’s disease.
Neurofeedback for Parkinson’s Disease is an emerging and experimental therapeutic approach aimed at helping individuals manage some of the symptoms associated with the condition. It’s important to note that Parkinson’s Disease involves complex neurodegeneration, and healthcare providers should consider neurofeedback as a complementary approach to conventional medical treatments rather than as a standalone option.
The Beta neurofeedback protocol for Parkinson’s Disease aims to enhance cognitive functioning and motor control by increasing beta brainwave activity (15-18 Hz).
Neurofeedback Protocol: “Beta Training”.
The specific neurofeedback protocols for Parkinson’s Disease may vary depending on the individual’s symptoms and the neurofeedback practitioner’s approach.
Some potential neurofeedback protocols for Parkinson’s Disease
- SMR (Sensorimotor Rhythm) Neurofeedback: The SMR protocol focuses on increasing the sensorimotor rhythm, a brainwave frequency range (12-15 Hz) associated with motor control and coordination. Enhancing SMR activity may improve motor function and coordination, benefiting Parkinson’s patients.
- Alpha-Theta Neurofeedback: This protocol combines alpha and theta training to promote relaxation and emotional regulation. While Parkinson’s Disease primarily affects motor function, individuals may also experience emotional challenges. Alpha-theta neurofeedback may help address emotional symptoms, such as anxiety and depression, which can be associated with Parkinson’s.
- Beta Neurofeedback: Beta brainwave frequencies (15-30 Hz) are related to alertness and attention. Attention and executive function can be affected in Parkinson’s disease, and beta neurofeedback may help improve attention and focus in some individuals.
Electrode Application Brain Regions: Central cortex (C3, C4), parietal cortex (Pz), and occipital cortex (Oz).
It’s important to emphasize that neurofeedback for Parkinson’s Disease is still an experimental approach. Its effectiveness has not yet been fully established through rigorous clinical trials. Research in this area is ongoing, and outcomes may vary depending on the individual.
Home Neurofeedback for Multiple Sclerosis (MS)
Multiple Sclerosis (MS) involves demyelination of nerve fibers, leading to various neurological symptoms.
Neurofeedback can be a potentially helpful approach for individuals with Multiple Sclerosis (MS) as it aims to improve brain function and address symptoms associated with the condition. However, it’s crucial to recognize that neurofeedback is not a cure for MS, and its effectiveness may vary from person to person. Many people use neurofeedback as a complementary therapy alongside other treatments and lifestyle interventions.
The SCP neurofeedback protocol for Multiple Sclerosis aims to promote neuroplasticity and support cognitive functions by regulating cortical excitability.
Neurofeedback Protocol: “SCP (Slow Cortical Potential) Training.”
Neurofeedback protocol for Multiple Sclerosis
The neurofeedback protocols for Multiple Sclerosis are designed to target brainwave patterns and neural activity related to specific disease symptoms. These protocols may include:
- SMR (Sensorimotor Rhythm) Neurofeedback: SMR training focuses on increasing the SMR brainwave frequency (12-15 Hz) and reducing higher beta frequencies. SMR neurofeedback aims to improve sensorimotor integration and motor function, which can benefit individuals with MS, especially those experiencing motor symptoms and mobility issues.
- Alpha-Theta Neurofeedback: This protocol combines alpha and theta training to promote relaxation and emotional regulation. People may use it to address symptoms related to stress, anxiety, and emotional well-being, which are essential aspects of managing MS.
- Low-beta neurofeedback targets low-beta brainwave frequencies (15-18 Hz) to encourage relaxation and alleviate stress. This can be helpful for individuals with MS who experience muscle tension, spasticity, or pain.
- Cognitive Enhancement Training: This neurofeedback protocol focuses on improving cognitive function, memory, and attention. It may benefit individuals with MS who experience cognitive challenges, such as memory, attention, and processing speed difficulties.
- Practitioners should personalize neurofeedback treatment for MS to address each individual’s specific symptoms and needs. A neurofeedback practitioner may tailor the training protocols based on the person’s unique neurological profile and symptoms.
Electrode Application Brain Regions
Frontal cortex (Fz, F3, F4), central cortex (C3, C4), and parietal cortex (Pz).
It’s important to emphasize that neurofeedback for Multiple Sclerosis should always be conducted under the guidance of a qualified and experienced neurofeedback practitioner or healthcare professional. Additionally, neurofeedback should be part of a comprehensive treatment plan that includes medical management, physical therapy, and other interventions to address the multifaceted challenges of living with MS.
NOTE
It’s important to emphasize that while neurofeedback holds promise for these pathological conditions, it should not be used as a standalone treatment. Instead, it should complement other evidence-based therapies within a comprehensive treatment plan. Moreover, individual responses to neurofeedback can differ, so qualified healthcare professionals must evaluate its effectiveness on a case-by-case basis.
Home Neurofeedback devices
Home neurofeedback devices based on the 10-20 system electrode position have gained popularity for their potential to offer convenient and accessible brain training solutions. These devices use EEG (electroencephalography) technology to provide real-time feedback, allowing individuals to learn how to self-regulate their brainwave patterns. Depending on the design and features, these devices can target various health conditions and promote overall well-being.
When considering a home neurofeedback device, it is essential to assess its features, ease of use, safety, and potential applications for different health conditions.
Home Neurofeedback for Attention, Anxiety, and Sleep Issues
Below are some general considerations and potential health conditions for which these devices can be applied:
- Attention Disorders (e.g., ADHD):
Home neurofeedback devices can assist individuals with attention disorders, like Attention Deficit Hyperactivity Disorder (ADHD), by focusing on specific brainwave frequencies associated with sustained attention and reduced impulsivity. Look for a device with training protocols that target beta and theta frequencies to improve attention and executive function. - Anxiety and Stress:
For anxiety and stress management, neurofeedback devices can target excessive beta activity and promote relaxation through training in alpha and theta frequencies. Seek a device with stress reduction programs and relaxation exercises to foster a calm state of mind. - Sleep Disturbances (e.g., Insomnia):
Home neurofeedback can aid individuals struggling with sleep disturbances by training brainwave patterns associated with deep sleep, such as delta frequencies. Please be on the lookout for a device with sleep-specific protocols to improve sleep quality and duration.
Home Neurofeedback for Mood, Cognitive Function, and Peak Performance
- Mood Disorders (e.g., Depression):
To address mood disorders like depression, neurofeedback can target brainwave frequencies related to mood regulation and emotional processing. Choose a device with mood enhancement programs focusing on alpha and beta frequencies. - Cognitive Enhancement:
Home neurofeedback can enhance cognitive function and memory by targeting specific brainwave frequencies associated with mental processing. Look for a device with cognitive training protocols focusing on gamma and beta frequencies. - Peak Performance (e.g., Sports, Creativity):
Some individuals use neurofeedback to optimize their performance in sports, arts, or creative pursuits. Seek a device with protocols to enhance focus, concentration, and flow states.
Important Features of Home Neurofeedback Devices to Consider:
- Electrode System:
Ensure the home neurofeedback device adheres to the 10-20 system for accurate electrode placement and reliable data collection. - Ease of Use:
Look for a user-friendly device with clear instructions and intuitive interfaces. Avoid complicated setups that may hinder consistent usage. - Real-Time Feedback:
The device should provide real-time feedback through visual, auditory, or tactile cues to help individuals learn to regulate their brainwave patterns effectively. - Customization:
Choose a device with adjustable training protocols to cater to individual needs and target specific health conditions effectively. - Data Analysis and Reporting:
Consider a device that offers data analysis and progress tracking to monitor improvements over time. - Safety:
Ensure the device meets safety standards and is approved for home use.
Conclusion:
Home neurofeedback devices based on the 10-20 system electrode position have the potential to empower individuals in addressing various health conditions and optimizing brain function. Before purchasing a device, carefully assess its features, safety, and potential applications for your specific needs. Keep in mind that while home neurofeedback can be a valuable tool, it’s essential to consult with a qualified healthcare professional for an accurate diagnosis and guidance on using such devices as part of a comprehensive treatment plan.
Neurofeedback Personal Use Device Classification in Accordance with Brain Region Electrode Placement
Comparing the electrode application sites on the brain for these neurofeedback devices – Forbrain, NeuroSky, Mendi, Muse 2, FocusCalm, Neeuro SenzeBand, BrainBit, Sens, and Enobio 20 – provides insights into their EEG recording capabilities and the brain regions they primarily focus on. This comparison is essential as the placement of electrodes impacts the type of brain activity data captured and the specific neurofeedback applications the devices can support. As a general guideline, EEG-based devices typically capture and analyze delta, theta, alpha and beta brainwaves.
Let’s examine the similarities and differences in electrode application sites and function of some home neurofeedback devices:
Brand of Neurofeedback personal device
Electrode Position on brain region
Main function and Neurofeedback protocol
Indication for use
None
Audio-vocal neurofeedback loop
Audio-vocal neurofeedback loop provide auditory feedback
- Speech performance
- Learning disability: Dyslexia
- Logopedic
- Tinnitus
- Post-stroke recovery of the speech
- Auditory feedback-based training to improve attention and memory
Prefrontal cortex (PFC)
Measure blood flow and oxygenation
Not EEG
Measure blood flow and oxygenation in the prefrontal cortex in response to neural activity.
Offers personalized neurofeedback exercises based on the user’s cognitive profile, using real-time feedback to target specific cognitive functions
- Cognitive Enhancement
- Attention Deficits
- Memory Improvement
- Focus Improvement
- ADHD
- Stress Management
- Recovery after Stroke
- HRV training
The Neuro VIZR device harasses specific light frequencies, stimulating targeted brainwave activity.
Non EEG
The Neuro VIZR device utilizes flashing light therapy to optimize brain function and improve mental clarity.
Harsing specific light frequencies stimulates targeted brainwave activity, promoting focus, relaxation, and overall cognitive performance.
- Cognitive Enhancement
- Mental Clarity
- Attention Deficits
- Memory Improvement
- Focus Improvement
- ADHD
- Stress Management
- Recovery after Stroke
Fp1
Basic neurofeedback applications, attention training, meditation, relaxation, and entertainment for educational purposes.
Provides basic neurofeedback protocols with real-time brainwave data and basic mental state monitoring with simple visual and auditory feedback based on attention and relaxation levels.
- Improving academic performance
- Performance Enhancement
- Cognitive Training
- Learning disability: Dyscalculia
- ADHD
- Anxiety and Relaxation
- Sleep Improvement
- Relaxation Therapy
- Stress Management
- Meditation and Mindfulness
- Mood Disorders
Fp1, Fp2, Fpz, TP9, TP10
Attention training and improvement through neurofeedback exercises for individuals with attention deficits.
Incorporates neurofeedback protocols for attention training and focus improvement, with visual feedback to enhance concentration.
- Attention Deficits
- ADHD (Attention Deficit Hyperactivity Disorder)
- Focus Improvement
- Decision making
- Memory
- Meditation
- Relaxation
- Breathing practice
Fp1, Fp2, AF7, AF8, TP9, TP10
Cognitive training, memory enhancement, attention deficits, ADHD, and brainwave-based gaming.
Offers cognitive training programs and brainwave-based games to enhance memory, concentration, and cognitive abilities , with audio and visual real-time feedback
- Cognitive Training
- Memory Enhancement
- Attention Deficits
- ADHD (Attention Deficit Hyperactivity Disorder)
- Meditation
- Breathing practice
- Relaxation
- Brainwave-based Gaming
Fpz, AF7, AF8, TP9, TP10
Provides heart meditation, breath meditation, body meditation, mind meditation.
Utilizes real-time audio feedback to guide users during meditation, helping them focus, calm mental state and reduce mind-wandering.
- Meditation
- Stress Reduction
- Anxiety Management
- Attention Training
- Improve mental wellbeing
- Improve daily mood
- Live a calmer, more relaxed, present life
O1,O2,T3,T4
Personalized neurofeedback protocols for cognitive enhancement, stress management, and memory improvement.
Provides personalized neurofeedback protocols targeting cognitive performance improvement and stress management
- Cognitive Enhancement
- Stress Management
- Memory Improvement
- Wellness
- Mindfulness
- Meditation
- Sleep Disturbance
- Education
- Sport
Fz, Cz, Pz
Sens.ai is the world’s first at-home brain training system to combine state of art neurofeedback with advanced light stimulation technology (transcranial photobiomodulation), heart coherence biofeedback and brain function assessment technology with advanced meditation training options.
Enhanced Neurofeedback protocols, includes 12 neurofeedback programs with real-time audio-visual feedback.
- Cognitive Performance Monitoring and training (concentration, attention, memory, clarity, brightening)
- Stress Level Measurement
- Anxiety
- Focused relaxation
- Deep relaxation
- Sleeping disturbance
- Meditation
Fp1, Fp2, Fz, Cz, Pz, F3, F4, F7, F8, T3, T4, T5, T6, O1, O2
A research-grade EEG device used for advanced brainwave monitoring analysis and training primarily for research and clinical purposes.
With its research-grade capabilities, this tool allows users to design and implement custom neurofeedback protocols for various applications.
- Sports Science
- Emotional Balance
- Attention Deficit Hyperactivity Disorder (ADHD)
- Sleep Disorders
- Mental Health Disorders (e.g., Depression, Anxiety, Schizophrenia)
- Epilepsy and Seizure Disorders
- Alzheimer’s Disease and Dementia
- Parkinson’s Disease
- Stroke Rehabilitation
- Brain Injury Rehabilitation
- Brain Tumors and Brain Cancer
- Traumatic Brain Injury (TBI)
- Multiple Sclerosis (MS)
- Frontal asymmetry