EMG BIOFEEDBACK, INDICATIONS AND CONTRAINDICATIONS, ELECTRODE APPLICATION SITES
Electromyography Biofeedback (EMG BFB) was approved by the Food and Drug Administration in the USA in 1991. It has been effectively used since 1992 without secondary effects or complications. This is the most frequently used biofeedback method in the treatment of various neurologic and neuromuscular disorders. The EMG biofeedback can be used to increase activity in weak or paretic muscle or it can be used to facilitate a reduction in tone is a spastic one.
Table of Contents
ToggleElectromyography (EMG) is an instrument that records the electrical activity of the muscles. It is a diagnostic procedure to assess the health of muscles and the nerve cells that control them, the conducting function of nerves. When muscles are active, they produce an electrical current. The current is usually proportional to the level of muscle activity. The EMG signal is a biomedical signal that measures the electrical current generated in muscles during its contraction representing neuromuscular activities. The electromyography signal records can be significantly affected by physiological parameters of the muscle, temperature, muscle cross-section area, and length. The EMG signal analysis is in clinical diagnosis and biomedical application and can be used to detect abnormal electrical activity of muscles. It can also be used to detect weakness as opposed to weakness from reduced use because of pain or lack of motivation, to isolate the level of nerve irritation or injury.
EMG biofeedback is the process of measuring and transforming the physiological information from muscle into visual and audio signals. The EMG biofeedback can be used to increase activity in weak or paretic muscle or it can be used to facilitate a reduction in tone is a spastic one.
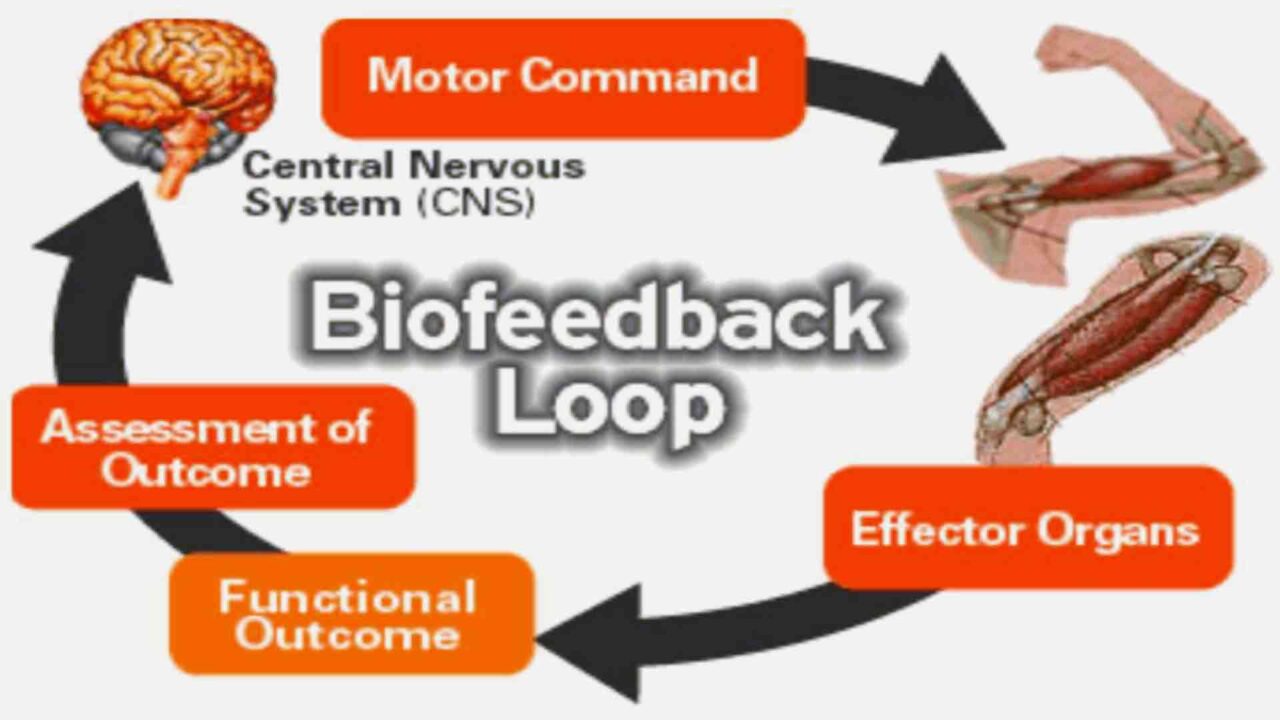
EMG Biofeedback Loop
During an injury, not only are bones, ligaments, and muscles hurt, but special nerve receptors are hurt as well. These receptors, found in muscle, send information back to the brain about where the bodies’ joints are while in motion, and how hard they are working. If these receptors are not retrained during rehabilitation, injury is much more likely to reoccur. It has been shown that EMG biofeedback is useful in both musculoskeletal and neurological rehabilitation.
Indication for EMG Biofeedback use
EMG biofeedback used
- to facilitate muscle contractions,
- to promote increased motor recruitment and improve poor mechanics,
- to regain neuromuscular control,
- to retrain joints’ function after injury,
- to improve posture,
- to improve gait patterns,
- to improve balance
- to decrease muscle spasm,
- to calm down over-active muscles,
- to promote relaxation
EMG biofeedback devices use surface electrodes to detect electrical activity in skeletal muscle. They can be used one of two ways:
• To retrain injured muscles
• To calm down overactive muscles
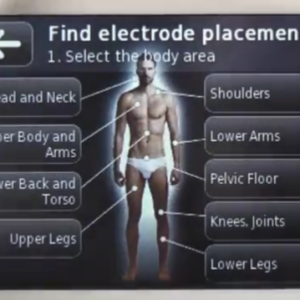
Skin Preparation and Electrode Placement Sites for EMG Biofeedback
Proper skin preparation and electrode positioning are essential elements in acquiring quality EMG measurements.
While there are no general rules for skin preparations, the type of application and signal quality sought usually determines the extent of skin preparation. For example, given a targeted test condition if the movement is somewhat static or slow-moving and only qualitative reading is desired, a simple alcohol swab around the area of interest is sufficient. However, if dynamic conditions present risk of the introduction of movement artifacts like in walking, running or other planned accelerated movements, thorough preparation is required. Skin preparation for surface electrodes usually involves removing the patient’s hair around the electrode site to improve electrode adhesion.
Cleaning the skin then involves one of the following methods:
- Strict use of alcohol swabs to clean the skin surface which is often sufficient in static EMG measurements.
- Use of fine sandpaper to abrade the skin surface combined with alcohol swabbing to clean the dead skin, oil and or dirt to lower skin impedance.
- Use of special abrasive and conductive pastes to remove dead skin and lower skin impedance.
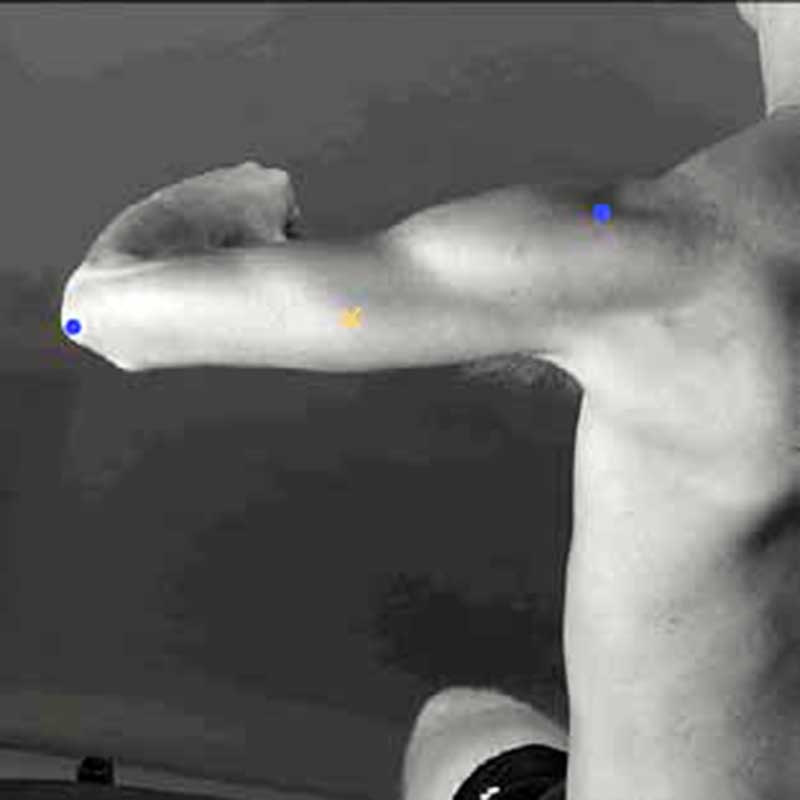
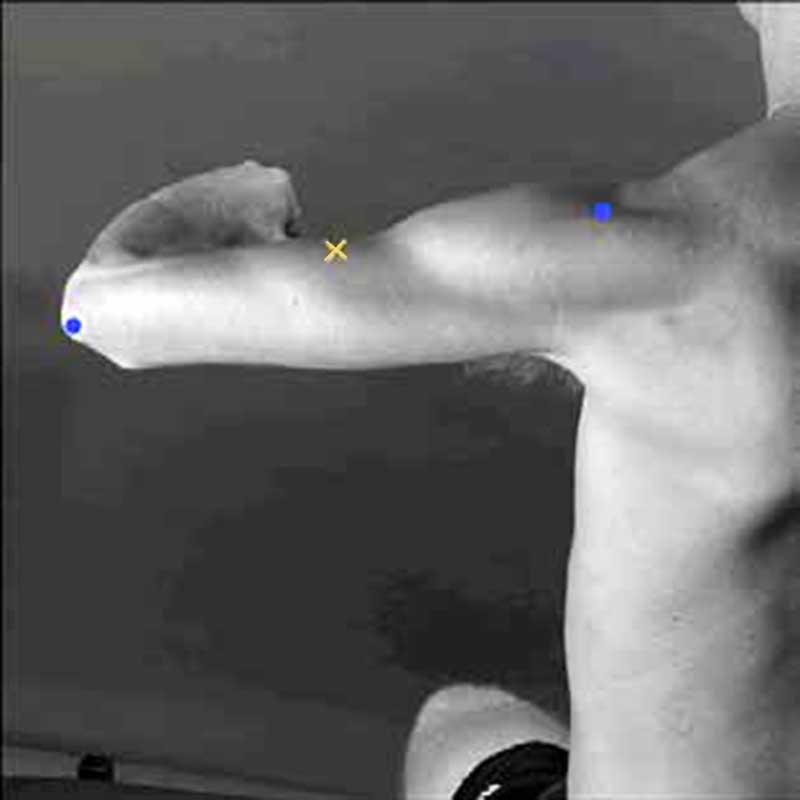
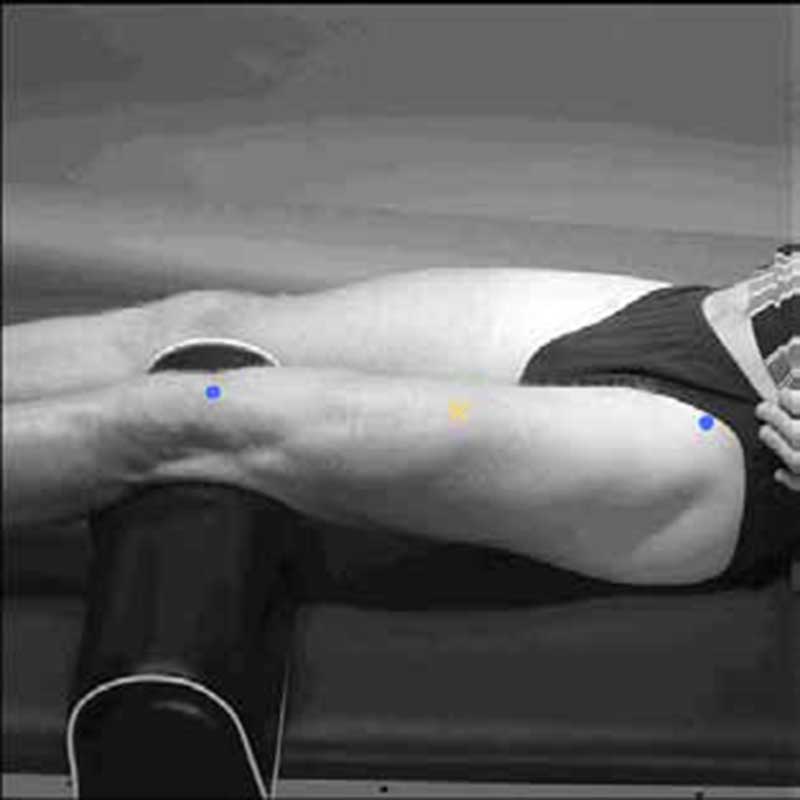
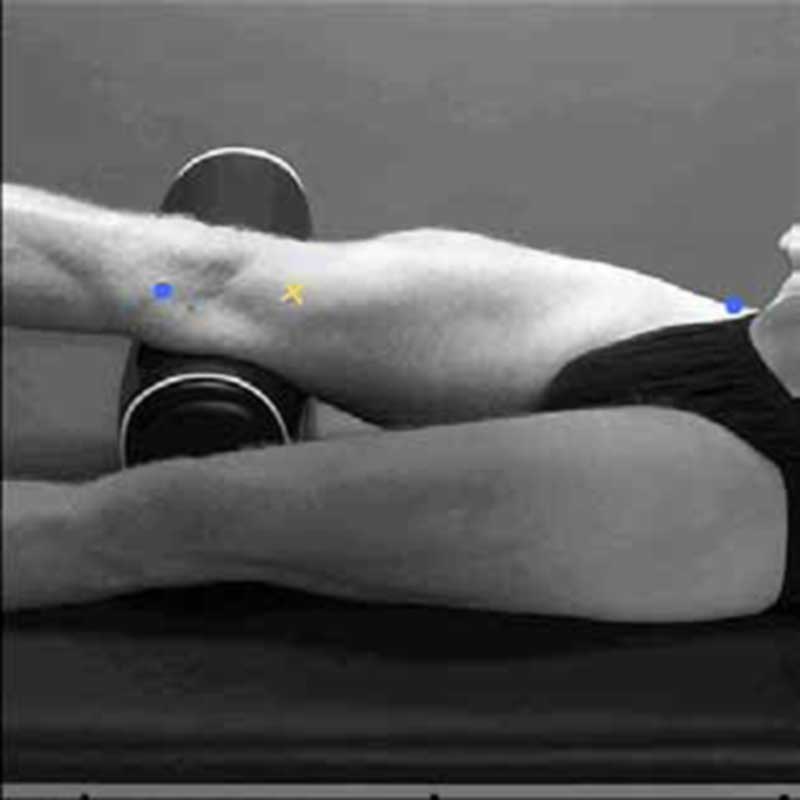
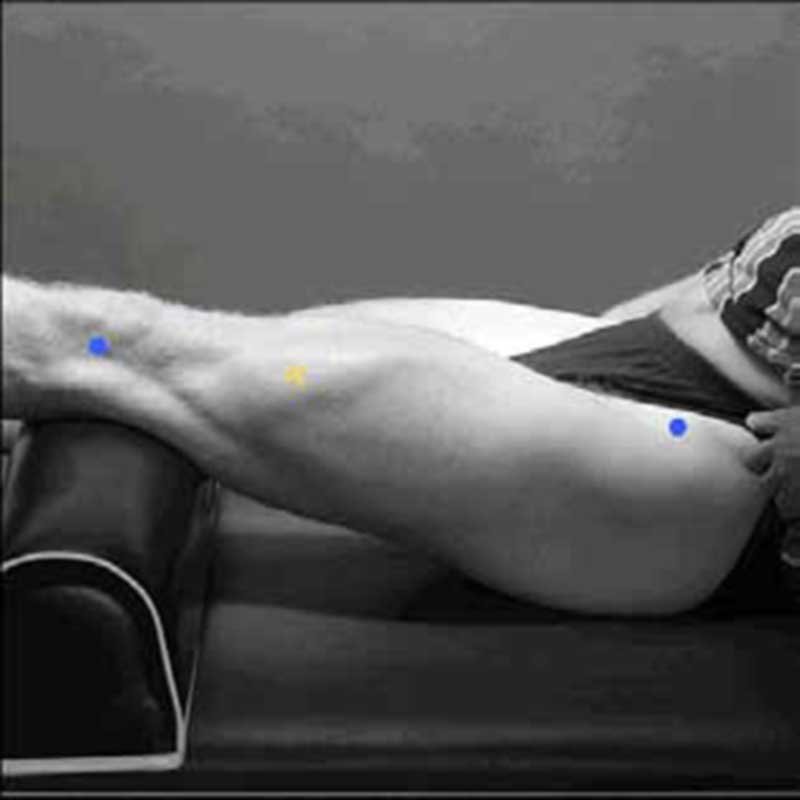
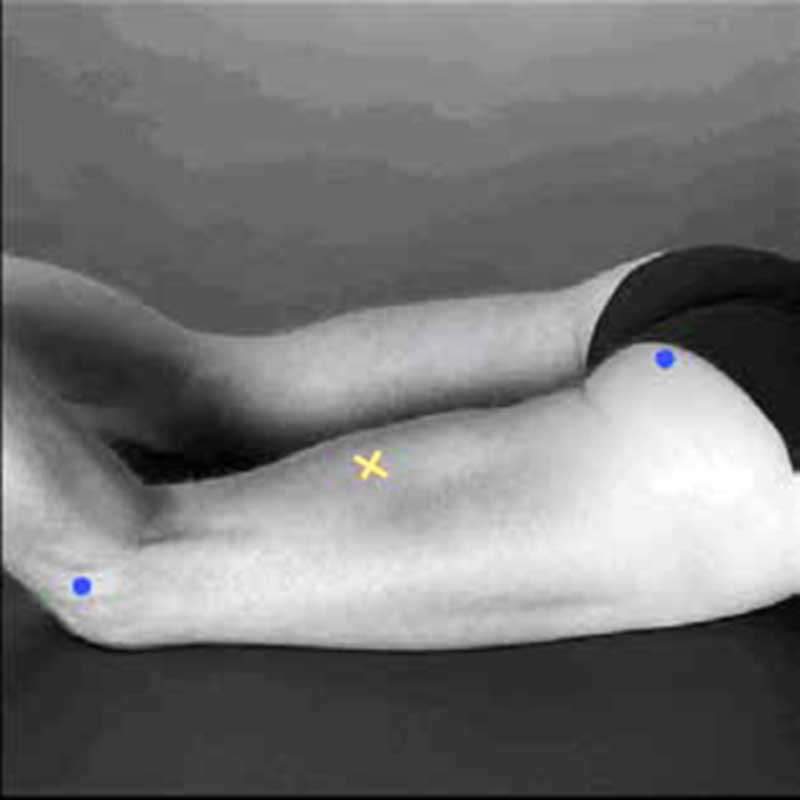
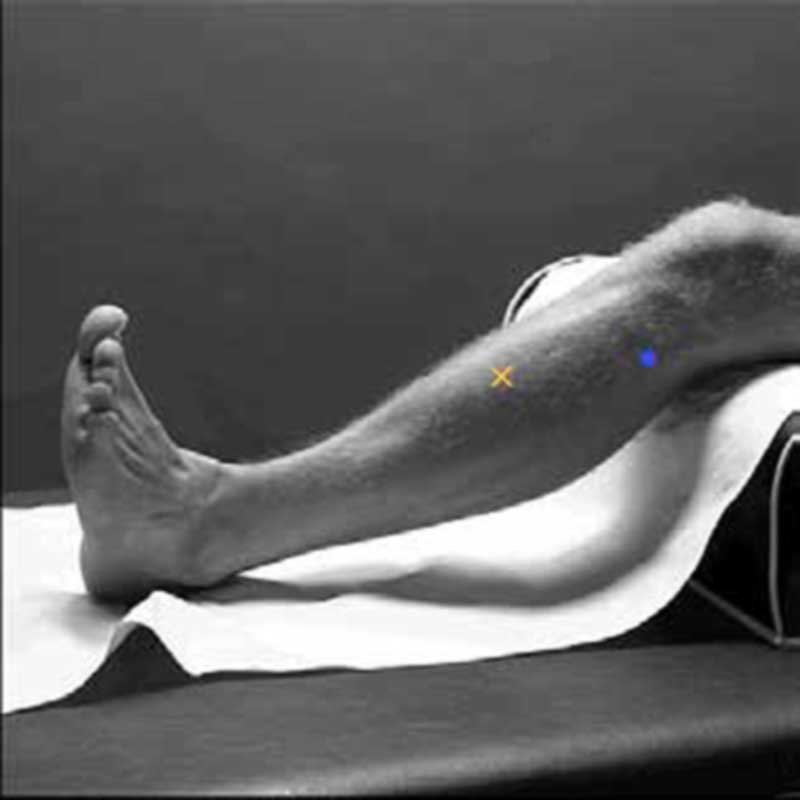
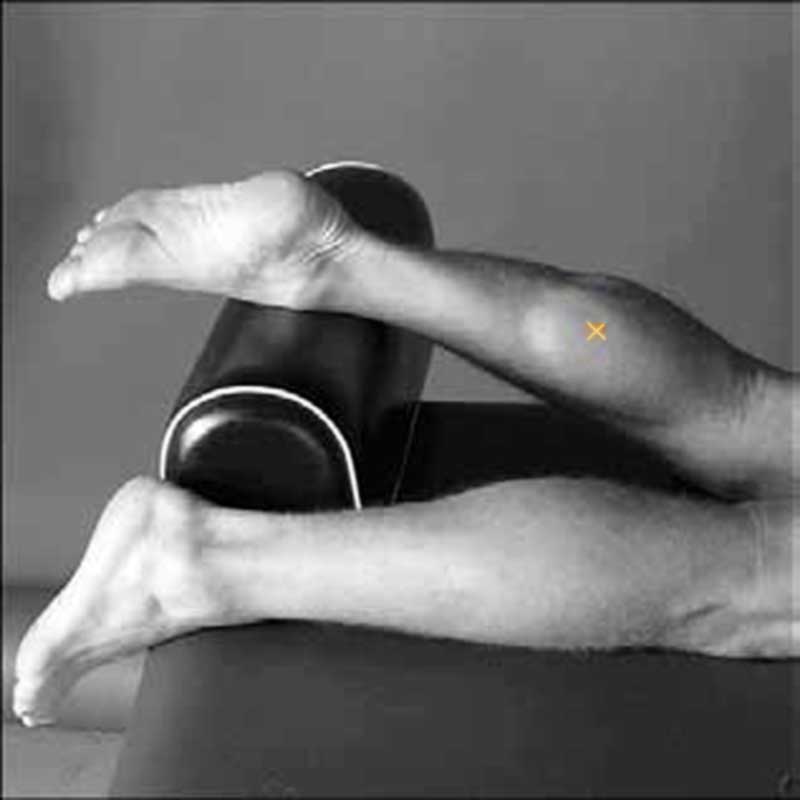
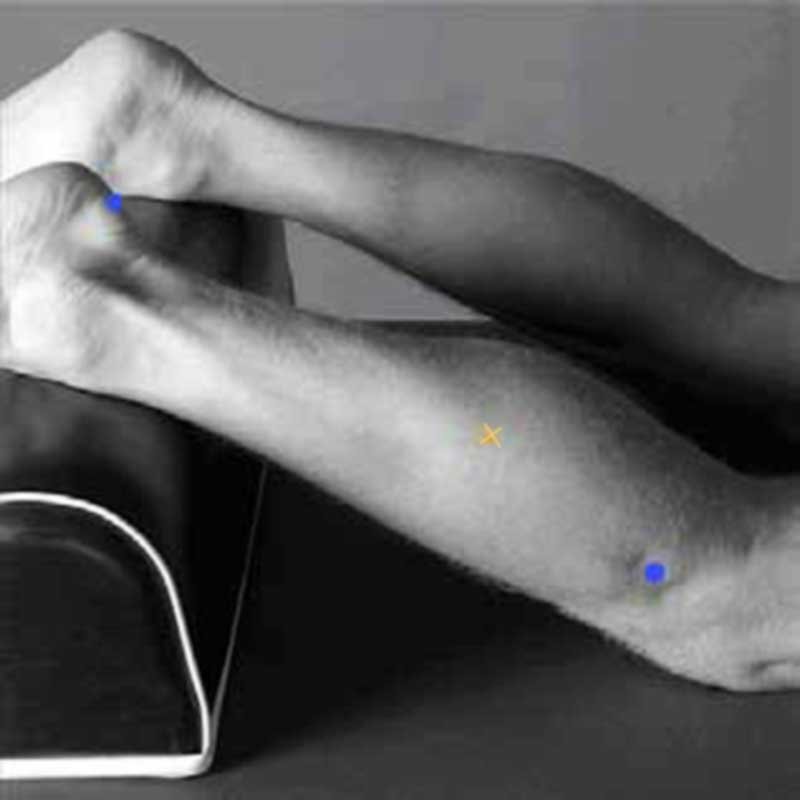
The picture shows recommended differential electrode placement sites for both fine wire and surface EMG. These sites are well defined and are known as anatomical landmark sites.
The placements of these differential electrode pairs are always along the direction of the muscle fibers under study.
- Electrodes should be placed as near to the muscle being monitored as possible,
- Electrodes should be parallel to the direction of the muscle fibers,
- The spacing of the electrodes is critical to reducing extraneous electrical activity (noise).
When required, placement of the reference electrode is typically more proximal and away from the differential electrodes, preferably on electrically neutral tissue (say over a bony joint).
Recommended differential electrode placement sites for both fine wire and surface EMG
Biceps Bracchi
| Anatomy | |
| Subdivision | Short and Long head |
| Function | Elbow flexion |
| Placement | |
| Start position | Flexed elbow at a right angle, the dorsal side of the forearm in a horizontal downward position |
| Location | Line medial acromion – fossa cubit, at 1/3 from fossa cubit (elbow pit) |
| Orientation | Parallel to line acromion – fossa cubit |
| Test | Flex the elbow, while applying pressure to the forearm in the direction of extension |
Triceps Bracchi (long head)
| Anatomy | |
| Subdivision | Long head |
| Function | Elbow extension, adduction, shoulder extension |
| Placement | |
| Start position | The shoulder at 90° abduction with arm 90° flexed, the palm of the hand pointing downward |
| Location | At 50% of line posterior crista of acromion – olecranon, 2 fingers medial to this line |
| Orientation | Parallel to line posterior crista of acromion – olecranon |
| Test | Extend the elbow while applying pressure to the forearm in the direction of flexion |
Triceps Bracchi (lateral head)
| Anatomy | |
| Subdivision | Lateral head |
| Function | Elbow extension |
| Placement | |
| Start position | The shoulder at 90° abduction with arm 90° flexed, the palm of the hand pointing downward |
| Location | At 50% of line posterior crista of acromion – olecranon, 2 finger lateral to this line |
| Orientation | Parallel to line posterior crista of acromion – olecranon |
| Test | Extend the elbow while applying pressure to the forearm in the direction of flexion |
Rectus Femoris
| Anatomy | |
| Subdivision | |
| Function | Extension of the knee joint and flexion of the hip joint |
| Placement | |
| Start position | Sitting on the table, knees in slight flexion, upper body slightly bend backward |
| Location | At 50% of line anterior spina iliaca superior -superior part of the patella |
| Orientation | Parallel to line anterior spina iliaca superior -superior part of the patella |
| Test | Extend knee while pressing against the leg above the ankle in the direction of flexion |
Vastus Medialis
| Anatomy | |
| Subdivision | |
| Function | Extension of the knee joint |
| Placement | |
| Start position | Sitting on the table, knees in slight flexion, upper body slightly bend backward |
| Location | At 80% of line anterior spina iliaca superior -anterior border of the medial ligament |
| Orientation | Almost perpendicular to line anterior spina iliaca superior – anterior border of the medial ligament |
| Test | Extend knee while pressing against the leg above the ankle in the direction of flexion |
Vastus Lateralis
| Anatomy | |
| Subdivision | |
| Function | Extension of the knee joint |
| Placement | |
| Start position | Sitting on the table, knees in slight flexion, upper body slightly bend backward |
| Location | At 2/3 of line anterior spina iliaca superior – lateral side of the patella |
| Orientation | In the direction of muscle fiber |
| Test | Extend knee while pressing against the leg above the ankle in the direction of flexion |
Biceps Femoris
| Anatomy | |
| Subdivision | Long head (LH) and short head |
| Function | Flexion and lateral rotation of the knee joint. LH also extends lateral rotation of hip joint |
| Placement | |
| Start position | Lying on the belly, thigh down on the table, knees flexed, thigh in slight lateral rotation, leg in slight lateral rotation with respect to the thigh |
| Location | At 50% of line ischial tuberosity – lateral epicondyle of the tibia |
| Orientation | Parallel to line ischial tuberosity – lateral epicondyle of the tibia |
| Test | Press against the leg proximal to the ankle in the direction of knee extension |
Tibialis Anterior
| Anatomy | |
| Subdivision | |
| Function | Dorsiflexion of ankle joint, inversion of the foot |
| Placement | |
| Start position | Supine or sitting |
| Location | At 1/3 of line tip of fibula – the tip of medial malleolus |
| Orientation | Parallel to line tip of fibula – the tip of medial malleolus |
| Test | Support leg just above the ankle joint with ankle joint in dorsiflexion and the foot in inversion without extension of the big toe. Apply pressure against the medial side, dorsal surface of the foot in direction of plantar flexion of ankle joint and eversion of the foot. |
Soleus
| Anatomy | |
| Subdivision | |
| Function | Plantar flexion of ankle joint |
| Placement | |
| Start position | Sitting with knee approx. 90° flexed and heel/foot on the floor |
| Location | At 2/3 of line medial condylis of the femur – medial malleolus |
| Orientation | Parallel to line medial condylis – medial malleolus |
| Test | Put hand on the knee and push knee down while asking subject to lift heel from the floor |
Gastrocnemius Medialis
| Anatomy | |
| Subdivision | Medialis |
| Function | Flexion of ankle joint, flexion knee joint |
| Placement | |
| Start position | Lying on the belly, knee extended, foot projecting over the end of the table |
| Location | At most prominent bulge of muscle |
| Orientation | Parallel to the lower leg |
| Test | Plantar flexion of foot with emphasis on pulling heel upward more than pushing forefoot down. Apply pressure against the forefoot as well as calcaneus |
Gastrocnemius Lateralis
| Anatomy | |
| Subdivision | Lateralis |
| Function | Flexion of ankle joint, flexion of knee joint |
| Placement | |
| Start position | Lying on the belly, knee extended, foot projecting over the end of the table |
| Location | At 1/3 of line head of fibula – heel |
| Orientation | Parallel to line head of fibula – heel |
| Test | Plantar flexion of foot with emphasis on pulling heel upward more than pushing forefoot down. Apply pressure against the forefoot as well as calcaneus |
APPLICATIONS & BENEFITS OF EMG
Medical
- Orthopedic
- Surgery
- Functional neurology
- Gait and posture analysis
Rehabilitation
- Post-surgery/accident
- Neurological rehabilitation
- Physical therapy
- Active training therapy
Ergonomics
- Analysis of demand
- Risk prevention
- Ergonomics design
- Product certification
Sport science
- Biomechanics
- Movement analysis
- Athletes strength training
- Sports rehabilitation
Practical medical applications of EMG biofeedback involves it use in pre/post-surgical assessment and treatment, prevention or retardation of muscle atrophy, increasing local blood circulation, relaxation of muscle spasms, maintaining or increasing range of motion, and muscle re-education and rehabilitation.
Stroke victims and individuals diagnosed with incontinence (lack of voluntary control of excretory functions) typically undergo training regimens that enable them to regain functional control over specific muscles. The electrical activity normally presents during a patient’s muscle contraction and relaxation cycle is often characteristically different or much weaker and harder to detect on damaged muscle sites. Through the careful and skilled placement of certain electrodes onto specific electrode sites, EMG biofeedback provides the patient and therapist with objective information about the subject’s muscle activity in real-time. The EMG user directly benefits from the instant feedback increasing his/her self-awareness of the muscular activity under direct conscious control and accelerates the therapist’s instruction to the patient to improve the patient’s ability to complete specific movements.
The conditions listed below can benefit from EMG biofeedback:
- Muscle atrophy or weakness due to disease or injury ( Stroke, Spinal cord injury, Chronic musculoskeletal injury, ),
- Joint contracture,
- Balance and mobility disorders,
- Trunk muscle re-education,
- Respiratory muscle control,
- Hypertension,
- Idiopathic Reynaud’s disease,
- Posture pathology, scoliosis, osteochondrosis,
- Club-foot
- Pain,
- Cauda equina syndrome with neurogenic bladder,
- Incontinence
– Anal sphincter spasm.
– Atonic bladder,
– Extrinsic urethral sphincter’s deficiency,
– Urethral instability.
– Fecal incontinence,
– Specific and non-specific acute urinary retention,
– Incomplete bladder emptying,
– Urgency urinary incontinence,
– Female stress urinary incontinence,
– Female and male mixed urinary incontinence,
– Urinary incontinence without voiding desire,
– Post-micturition dribbling,
– Nocturnal enuresis,
– Continuous leakage and urinary frequency,
Contraindication for EMG biofeedback performance
- If the patient is prohibited from moving the joint or isometric contractions, then EMG BFB should not be used,
- Unhealed tendon grafts,
- Avulsed tendon,
- A third-degree tear of muscle fibers,
- Unstable fracture,
- Injury to joint structure, ligaments, capsule, or articulating surface.
EMG BIOFEEDBACK HOME USE DEVICES
There are many kinds of electromyographic biofeedback devices. The most complicated is usually found in therapeutic and clinical settings, and are administered with the help of a doctor or other healthcare professional who can help you get the most out of it.
But there are also smaller, less powerful (but still helpful) devices that you can purchase and use as part of a daily regimen to help you train your body to overcome your unconscious muscular reactions to the stress and anxiety of modern life.
The uses of electromyographic biofeedback aren’t limited to just stress and stress-related conditions. They also help those suffering from chronic migraines, and assist with psychological therapies such as mindfulness meditation. There are even athletes who have been experimenting with electromyographic biofeedback therapies to help them achieve new heights of physical fitness. EMG biofeedback home use device can be used to solve muscular rehab problems.
NeuroTrac® Simplex
NeuroTrac® Simplex is a single channel EMG unit that suitable for diagnosing, monitoring, and treating a wide range of muscle problems.
• Suitable for diagnosing, monitoring and treating a wide range of muscle problems
• Single Channel EMG unit
• The optional multilingual computer database system
• Structured protocols for consistency of patient progress reports (software)
• Used as an EMG biofeedback training aid or diagnostic tool
• Measures EMG from 0.2µV to 2000µV Accurately
• Designed for a wide range of physiotherapy applications such as incontinence, shoulder and neck pains, patellofemoral pain, repetitive strain injury, stroke plus much more
• Used as a learning tool for both patients and therapists with emphasis on improving rehabilitation techniques
• Produces and prints comprehensive patient progress reports of work/rest averages, onset contraction and muscle release times, peak values, work/rest average deviations (with optional software)
• Ability to lock the unit
• Records EMG statistics
• User-friendly
• Compact, light and reliable
• Easy to use optional software available
• Low-cost high quality and very accurate
You can power on this easy to use Biofeedback unit and the real-time EMG will be continuously measured. You can press the START button to begin the Work/Rest program. Here you will be prompted to contract and relax muscles. When the session is finished, the statistics will be displayed on the LCD: work time, rest time, onset and release time. One easy to use the customizable program, where you can use the default settings or change: work time, rest time, number of repetitions, etc.
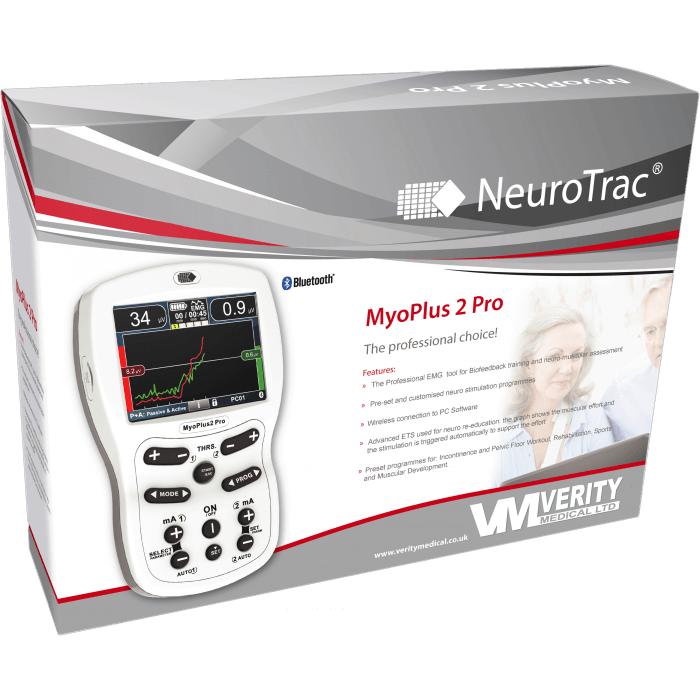
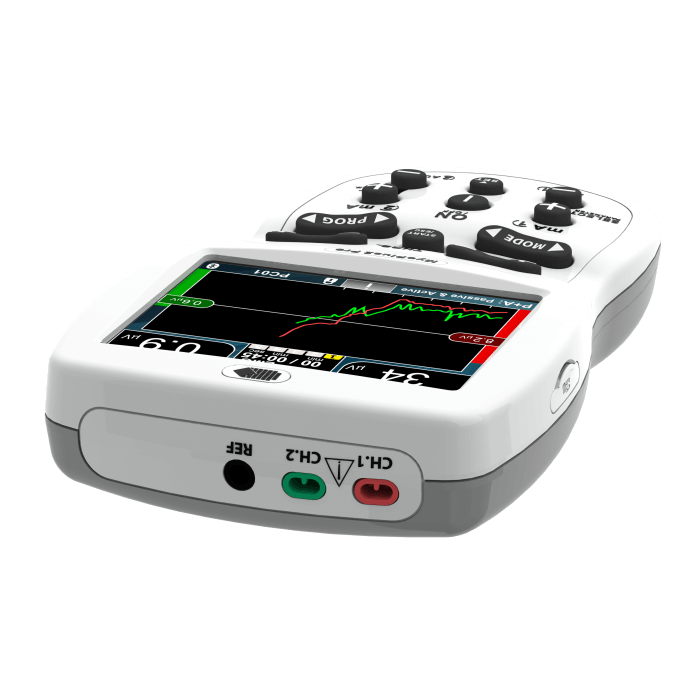
NeuroTrac® MyoPlus2 Pro
NeuroTrac MyoPlus2 Pro is a new and improved touch-screen with a full-color display. The new user-friendly interface makes it a self-explanatory unit with the interactive learning on the go, including electrode placement, running EMG graph as well as many other helpful tools.
• New and Improved touch-screen with a full-color display. The new user-friendly interface makes it a self-explanatory unit with interactive learning on the go, including electrode placement, running EMG graph, EMG biofeedback Games and Templates as well as many other helpful tools.
• Pre-set programs for Incontinence treatment, Sports and muscular development, neuromuscular Rehabilitation.
• Designed for Physiotherapists in mind to be used as a portable tool. Suitable as a personal trainer for in-clinic or home use (under guidance).
• 2 channel EMG (Biofeedback) combined with 2 channels of NMES (stimulation).
• 2 channel ETS (EMG triggered stimulation) with stimulation on 2 channels.
• Simple single-phase or multiphase operation: multiphase allows EMG/ETS/STIM to be combined in one program.
• Multilingual LCD screen and voice prompts for Biofeedback.
• Manual and Automatic threshold control.
• EMG Biofeedback between stimulation (muscle activity and tiredness indication when using muscle stimulation).
• Stand-alone device or used in conjunction with established multilingual software.
• Up to 10 meters of wireless (Bluetooth) connection for NeuroTrac Software.
• For home users: Produces and prints (with the optional PC Software) the comprehensive patient progress reports on a day to day basis providing average readings (2 channels) on work/rest, peak, onset and muscle release times, work and rest deviations and the average mA current.
• Used as a learning tool for both patient and clinician with emphasis on improving treatment techniques in the use of EMG and Neuromuscular stimulation.Model number: MYO220P. This product is available through selected distributors who are able to provide training and support.