Migraine is a debilitating illness with long-term consequences for the brain. Research has explored the origins of migraine and suggests that it is an electrical phenomenon initiated in the occipital cortex. Assessments of the brain using the EEG have found abnormal electrical activity supporting this idea. Neurofeedback for migraines is a treatment targeting electrical firing patterns in the brain. Many research data have shown that Neurofeedback therapy for migraines successfully suppresses abnormal brain wave activity, leading to a significant decrease in migraine frequency and improvement in associated psychoneurological states such as anxiety, depression, and sleep.
Table of Contents
Toggle- WHAT IS MIGRAINE? CAUSES, SYMPTOMS, AND PATHOPHYSIOLOGY.
- WHAT KIND OF CHANGES IN THE BRAIN CAUSE THE MIGRAINE?
- WHAT EEG CHANGES CAN BE OBSERVED IN PEOPLE WITH MIGRAINES?
- How Neurofeedback Training Manage Migraines?
- Electrode Placement and Detailed Neurofeedback Protocols for Migraine Management
- How effective is neurofeedback for migraines?
- Best Home Neurofeedback Device
- Effective Use of Various Biofeedback Modalities for Migraine Management
WHAT IS MIGRAINE? CAUSES, SYMPTOMS, AND PATHOPHYSIOLOGY.
Migraine is a severe health problem, the second most common primary headache, affecting 3-10 to 30-38% of the world’s population and negatively affecting quality of life. It is a disabling neurological condition characterized by episodic attacks of usually unilateral headache, with a pulsating character and light and sound intolerance, associated with nausea and vomiting.
The tendency to suffer from migraine has a genetic component, but a series of internal and external factors can trigger attacks.
Migraine is a disease with many faces. The most common form is migraine without aura, occurring in about 80% of patients, while migraine with aura occurs in about 20% of the patients.
Migraines cost 5 billion euros annually in the European Union and about 29 billion in the USA, including expenses for diagnosis, treatment, reduced productivity, and work absences.
The incidence of migraine before puberty is more significant in boys than in girls. It grows up to 12 years in both sexes and is the highest in the age range of 30–40. After puberty, the ratio changes and increases in favor of women, and with 40, it is 3.5:1. After age 40, migraine symptoms generally become less severe, except for women in perimenopause, and it is rare for migraine headaches to begin in a person’s fifties.
Migraine trigger checklist

The main symptoms of migraine are recurring, severe, most often localized in one half of the head (hemicrania), and throbbing headache, which can last from 4 to 72 hours. It usually begins in the temporal region, in the eyeballs, or in the frontal region. Pain may also occur in the face and neck. A migraine attack may cause visual disturbances, heightened sensitivity in the hands, dizziness, tinnitus, and increased sensitivity to light or noise. At the end of an attack, nausea and vomiting may occur.
There are migraines with and without aura. Aura is a complex of neuropsychological symptoms that anticipate the onset of pain, become the first signs of a migraine, or develop simultaneously with a headache. A spasm of cerebral vessels, occurring in the initial stage of an attack, causes these symptoms.
Symptoms associated with Migraine are:
- Severe pain in the head or eyes;
- Being worse on one side of the head;
- Nausea
- Vomiting;
- Dizziness ;
- Perceiving an aura;
- Blurred or tunnel vision;
- Seeing auras;
- Photophobia (sensitivity to light);
- Phonophobia (sensitivity to sound);
- Osmophobia (sensitivity to smells);
- Poor concentration;
- Ringing in the ears;
- Sweating;
- Feeling very hot or very cold;
- Abdominal pain (which can sometimes cause diarrhea);
- A frequent need to urinate.
The pathogenesis of migraine
The Evolving Understanding of Migraine Pathogenesis
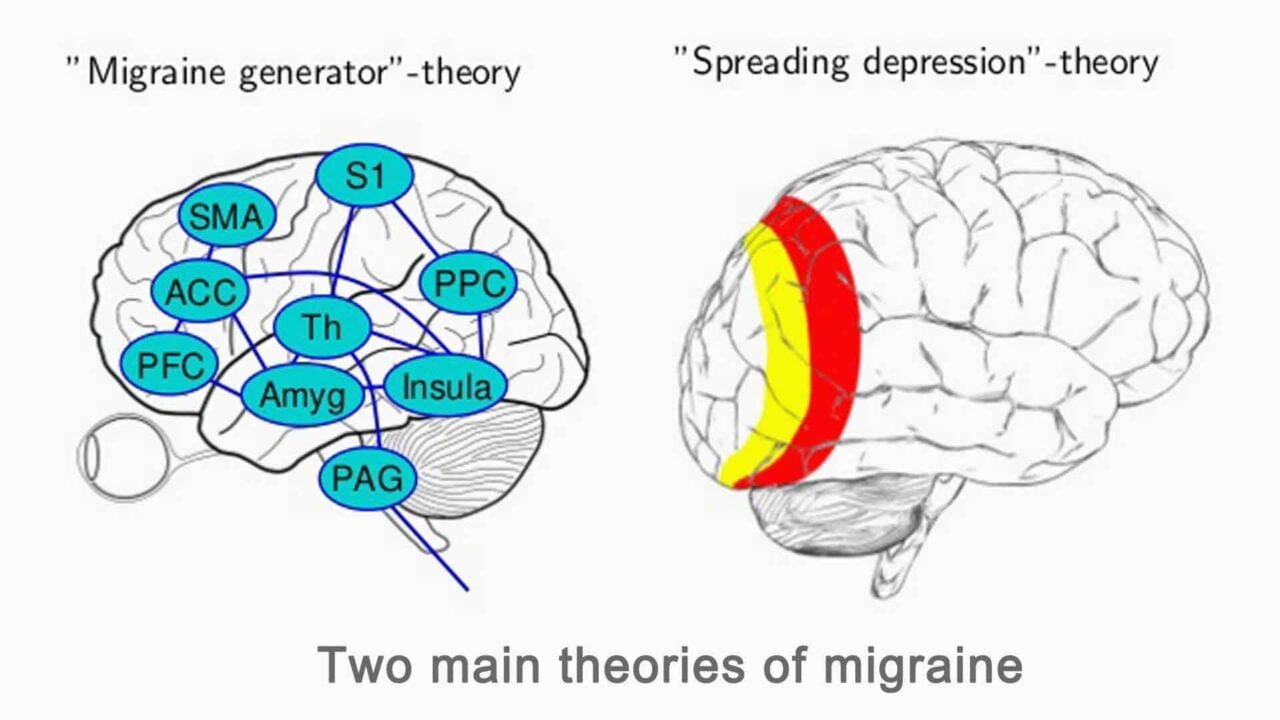
The pathogenesis of migraine has long been a subject of discussion among scientists.
The vascular theory states that intracranial vasodilation after vasoconstriction causes typical headaches and triggers the aura. However, new research has debunked this theory. Despite emerging findings, scientists still struggle to clarify the exact mechanisms and genetic determinants.
For years, people believed cerebral vasoconstriction triggered the aura before headaches. Now, researchers understand that neural dysfunction, not ischemia from vasoconstriction, causes the aura.
The frequency with which migraine attacks occur may vary from once in a lifetime to almost daily, an indication that the degree of migraine predisposition differs individually.
Triggers, Vulnerability, and the Phases of Migraine
It is necessary to consider both the factors that influence the threshold of a person’s susceptibility to a migraine attack and also the mechanisms that trigger the attack and the associated symptoms.
Acute migraine attacks occur in the context of an individual’s inherent level of vulnerability. The greater the vulnerability/lower the threshold, the more frequent attacks occur. Internal or environmental triggers initiate attacks when they are sufficiently intense, activating a series of events that culminate in a migraine headache. Many migraineurs experience vague vegetative or affective symptoms as much as 24 hours before the onset of a migraine attack. This phase is called the prodrome and should not be confused with the aura phase.
The aura phase consists of focal neurological symptoms that persist for up to one hour. Symptoms may include visual, sensory, or language disturbance, as well as symptoms localizing to the brainstem.
Within an hour of the resolution of the aura symptoms, the typical migraine headache usually appears with its unilateral throbbing pain and associated nausea, vomiting, photophobia, or phonophobia. Without treatment, the headache may persist for up to 72 hours before ending in a resolution phase often characterized by deep sleep.
Genetic Factors and the Familial Nature of Migraine
For up to twenty-four hours after the spontaneous throbbing has resolved, many patients may experience malaise, fatigue, and transient return of the head pain in a similar location for a few seconds or minutes following coughing, sudden head movement, or Valsalva movements. This phase is sometimes referred to as the migraine hangover (postdrome).
Researchers increasingly recognize that many individuals inherit their vulnerability to migraines.
Migraine is, in essence, a familial episodic disorder whose key marker is a headache, with certain associated features. One of the most critical aspects of the pathophysiology of migraine is the inherited nature of the disorder. It is clear from clinical practice that many patients have first-degree relatives who also suffer from migraines. Reports indicate that parents have transmitted migraines to their children since the seventeenth century, and numerous studies have documented a positive family history.
Researchers have assigned familial hemiplegic migraine (FHM) to chromosome 19p13 in approximately 50% of the documented families.
The biological basis for the linkage to chromosome 19 is mutations involving the Ca 2.1 (P/Q) type voltage-gated calcium channel CACNA1A gene. Dysfunction of these channels might impair serotonin release and predispose patients to migraine or impair their self-aborting mechanism.
Migraine aura
A migraine aura is a focal neurological disturbance manifesting as visual, sensory, or motor symptoms. Visual aura occurs in about 30% of patients and is driven by neural activity. It affects the visual field, indicating the involvement of the visual cortex, starting at the center and propagating to the periphery at a speed of 3 mm/min. Blood flow studies in patients have also shown that focal hyperemia precedes the spreading of oligemia. However, some researchers conclude that the aberrant firing of neurons evokes migraine aura.
Shown is the entire hemisphere from a posterior-medial view. The aura-related changes appeared first in the extrastriatal cortex. The spread of the aura began and was most systematic in the representation of the lower visual field, becoming less regular as it progressed into the representation of the upper visual field.
WHAT KIND OF CHANGES IN THE BRAIN CAUSE THE MIGRAINE?
The study of the anatomy and physiology of pain-producing structures in the cranium and the central nervous system’s modulation of input has led to the conclusion that migraine involves alterations in the subcortical aminergic sensory modulatory systems that influence the brain widely.
Available research data has shown that no structural differences have been found in individuals with migraine compared to individuals without migraine. This research suggests that migraine is an electrical phenomenon initiated within the cortex of the brain. This phenomenon is known as Cortical Spreading Depression (CSD), a wave of electrophysiological hyperactivity that spreads forward through the brain from the occipital lobes. This wave affects the cortex in several ways: altering the electrical polarity of neurons, decreasing blood flow and associated levels of oxygen in the cortex, and altering the degree of vasodilation within the vascular system of the cortex. These changes release of nerve irritating chemicals into the brain. These chemicals irritate the pain, transmitting the “trigeminal” nerve system in the meninges, the sensitive membranes that cover the brain. The result is severe blinding pain.
Consequences of migraine to the brain are:
- impaired ability in tests of short and long-term memory,
- small areas of stroke-like damage to the brain,
- with a high frequency of Migraine (more than three attacks per month) show significantly more areas of damage than those with fewer attacks,
- with a history of Migraines longer than 15 years were found to have more changes in the brain than those with a shorter history,
- higher frequency migraines show abnormalities in both white and gray matter of the brain,
- people with migraine are more at risk for future strokes,
- show a predilection toward damage in the following sites:
– frontal lobe
– limbic system
– parietal lobes
– brainstem
– cerebellum
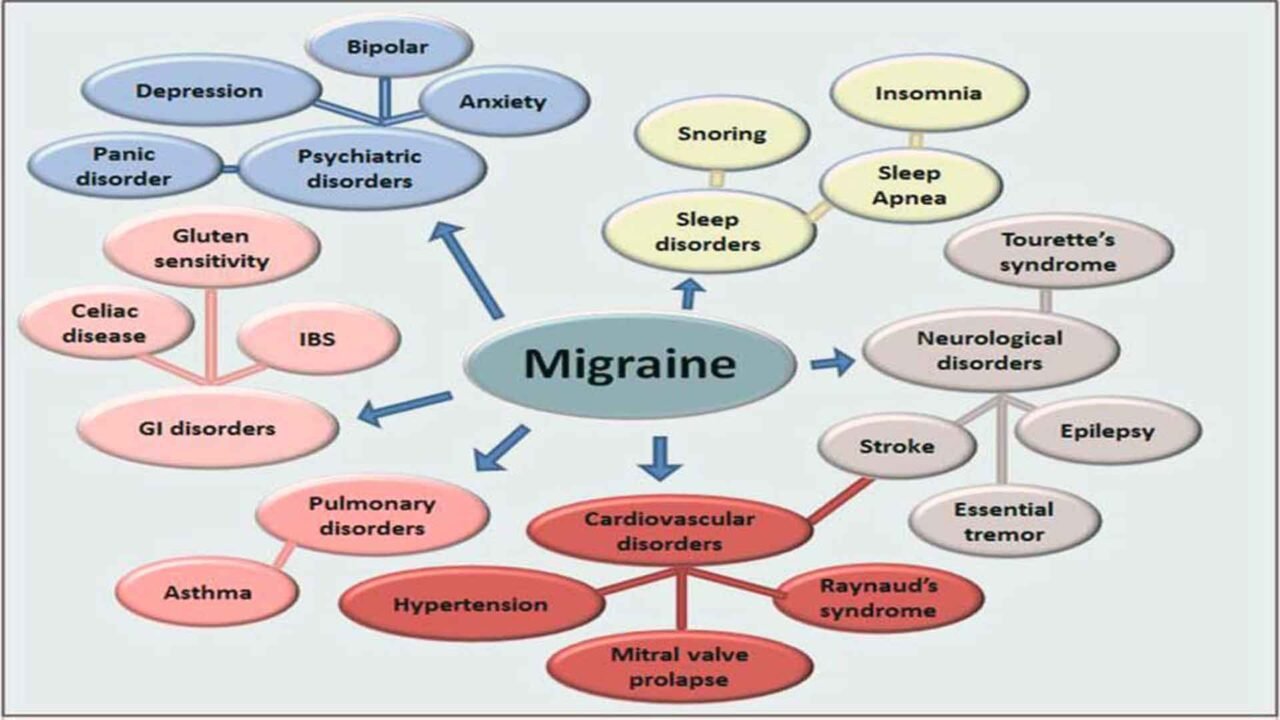
Chronic migraine comorbidities
WHAT EEG CHANGES CAN BE OBSERVED IN PEOPLE WITH MIGRAINES?
EEG Anomalies and Their Relationship to Migraine
There are two ways in which anomalies in the EEG have been associated with migraine: via the relationship of migraine to seizure activity and as a function of slow brain waves found elsewhere in the brain. Migraine and epilepsy frequently coexist and are often difficult to differentiate. Both migraine and seizure-prone individuals show abnormal occipital discharges that are typically high voltage (200–300 mV), with a diphasic morphology and a unilateral or bilateral occipital and posterior-temporal distribution.
Abnormal EEG Activity and Neurofeedback Applications
Migraine has been associated with abnormal EEG activity elsewhere in the brain. Both unilateral and bilateral increased delta wave activity has been recorded during a hemiplegic migraine and attacks of migraine with disturbed consciousness. It is shown that in the waking, non-migraine state, there are slow waves in the theta range (48 hertz). Neurofeedback therapy for migraines has been used to target and suppress this slow-wave activity in both adults and children, resulting in a concomitant reduction in the frequency and intensity of migraines. Some research has shown that neurofeedback blood flow-up training in the frontal cortex results in a 70% reduction in the frequency of migraines compared with a 50% reduction using medication alone. NFB training is also associated with decreases in anxiety, depression, and improved sleep, each of which has been associated with migraines.
Emerging Tools and EEG Patterns in Migraine Research
Newer methods, such as EEG frequency analysis and topographic brain mapping, are promising tools in this field. So far, mostly small studies have been published with somewhat inconsistent results. A pattern of increased alpha rhythm variability (and/or asymmetry) in the headache-free phase seems to emerge, however. A topographic brain mapping study has reported significant asymmetry of alpha and theta during headache.
The EEG patterns observed in migraine patients seem to suggest a possible physiological connection between sleep, hyperventilation, and migraine.
EEG activity seems to change shortly before the attack. This suggests that migraineurs are most susceptible to attack when anterior QEEG delta power and posterior alpha asymmetry values are high.
Occipitoparietal and temporal alpha power were more asymmetric before the attack compared with the interictal baseline
Different studies found increased power in 19 cortical areas in the delta (1.5-3.5 Hz), theta (4.0-7.5 Hz), and high-frequency beta (21-30 Hz) bands. Multiple types of research have shown significant abnormalities in the high-frequency beta band (21-30 Hz) in the parietal, central, and frontal regions.
How Neurofeedback Training Manage Migraines?
Despite a large number of medications being used to treat migraine today, only 20% of patients report their effectiveness. Many develop resistance to medications, and therefore, the dose of the drug is gradually increasing, which is required to achieve the effect of relieving headaches. Often, the medication is accompanied by side effects.
Changes in the biological parameters of brain activity and brain waves are often recorded in patients with migraines. Neurofeedback is a recently developed technology for treating migraines based on recording these changes in brain wave activity and transmitting information about the condition through audio and video signals to the patient. Based on these audio and video signals, the patient learns how to manage his condition to regulate brain wave activity and normalize it. Normalization of wave activity leads to a significant decrease in both the frequency and intensity of headaches. At first, these changes are not stable but gradually become stable and permanent. It becomes possible (after about ten sessions of treatment) to manage the condition without the support of special equipment and computer programs.
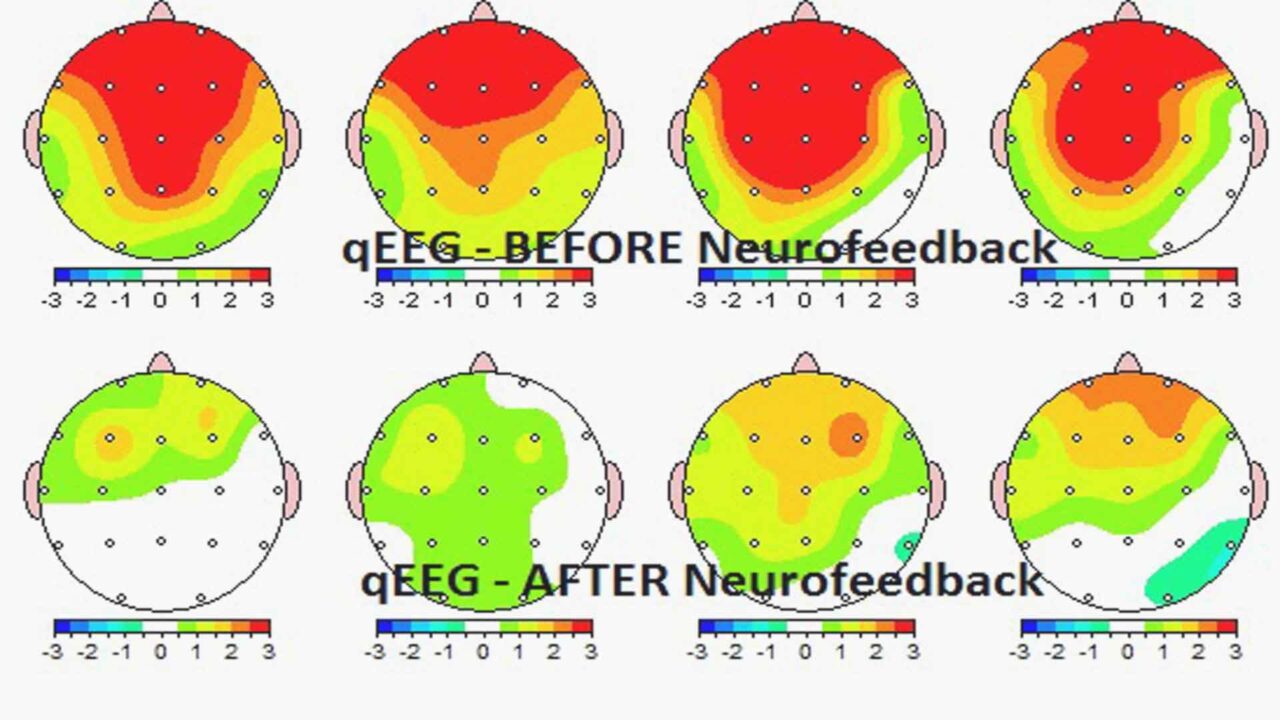
Migraine research points to electrophysiological anomalies in the brain as correlates of migraine headaches. Neurofeedback, as a therapy, is specifically designed to target dysregulated firing patterns in the brain. Research has demonstrated the ability of NFB to successfully treat anomalous brainwave patterns in various conditions, most specifically with migraines.
After performing diagnostic scanning and obtaining brain mapping patterns of migraine patients, some clinicians provide neurofeedback training with an increase of SMR and low beta (12-15 Hz) and decreased theta (4-7Hz) and high beta (21-30 Hz) at each affected site; 5 sessions for each affected site.
qEEG Before and after Neurofeedback for Migraines
Electrode Placement and Detailed Neurofeedback Protocols for Migraine Management
Key Electrode Sites for Migraine Neurofeedback
1. Fz (Frontal Midline):
- Location: Frontal lobe, on the midline, 20% of the distance from the nasion (bridge of the nose).
- Relevance: This site is associated with emotional regulation and autonomic control. Targeting this site can help manage stress and reduce the frequency and intensity of migraines.
2. Cz (Central Midline):
- Location: The scalp vertex, halfway between the nasion and inion and equally spaced between the left and right preauricular points (just above the ears).
- Relevance: The central region is involved in general arousal regulation and is often used as a reference or active site for enhancing overall neural stability.
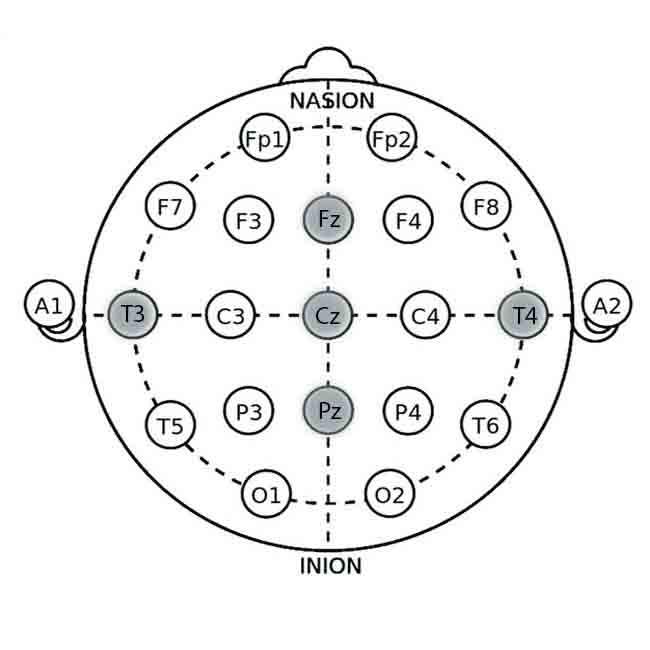
3. Pz (Parietal Midline):
- Location: Parietal lobe, on the midline, 50% of the distance from the nasion to the inion.
- Relevance: Involved in sensory processing and pain perception. Targeting Pz can help modulate sensory processing related to migraine pain.
4. T3 (Left Temporal Lobe):
- Location: Temporal lobe, 20% above the preauricular point.
- Relevance: This area is associated with stress and emotional regulation. Training in this area can help manage triggers related to emotional stress.
5. T4 (Right Temporal Lobe):
- Location: Temporal lobe, analogous to T3 on the right side.
- Relevance: Similar to T3, it helps balance activity related to emotional stress and can assist in reducing migraine frequency.
Neurofeedback Protocols for Migraine
The protocol involves training individuals to increase or decrease specific brainwave activity at the targeted locations to promote relaxation, improve stress management, and reduce migraine symptoms.
Alpha Enhancement Protocol
This protocol focuses on increasing alpha (8-12 Hz) activity to promote relaxation and reduce stress, which are common migraine triggers.
- Target Brainwaves: Alpha waves (8-12 Hz)
- Goal: Increase alpha activity to enhance relaxation and reduce stress-related migraine triggers.
Procedure:
1. Electrode Placement: Place electrodes at Fz and Pz with Cz as the reference.
2. Baseline Recording: Record baseline alpha activity for 5-10 minutes.
3. Feedback Mechanism: Provide real-time feedback using visual (e.g., calming images) or auditory (e.g., soothing sounds) cues. Positive feedback is given when alpha activity increases.
4. Training Sessions: Conduct 20-30 minutes of training sessions, 2-3 times per week, for 20-40 sessions.
5. Progress Monitoring: Assess changes using headache frequency, intensity diaries, and follow-up qEEG.
SMR Training Protocol
This protocol focuses on increasing sensorimotor rhythm (SMR, 12-15 Hz) activity to promote calmness and reduce hyperarousal that can trigger migraines.
- Target Brainwaves: SMR (12-15 Hz)
- Goal: Increase SMR activity to enhance motor inhibition and promote calmness.
Procedure:
1. Electrode Placement: Place electrodes at Cz with reference electrodes at mastoids (A1 and A2).
2. Baseline Recording: Record baseline SMR activity for 5-10 minutes.
3. Feedback Mechanism: Provide real-time feedback using visual or auditory cues. Positive feedback is given when SMR activity increases.
4. Training Sessions: Conduct 20-30 minutes of training sessions, 2-3 times per week, for 20-40 sessions.
5. Progress Monitoring: Monitor changes with headache frequency, intensity diaries, and follow-up qEEG.
Theta/Beta Ratio Training
This protocol aims to balance theta (4-8 Hz) and beta (15-20 Hz) wave activity to improve cognitive control and reduce stress, which can contribute to migraine frequency.
- Target Brainwaves: Theta (4-8 Hz) and Beta (15-20 Hz)
- Goal: Decrease theta activity and increase beta activity to improve cognitive control and reduce stress.
Procedure:
1. Electrode Placement: Place electrodes at T3 and T4 with Cz as the reference.
2. Baseline Recording: Record baseline theta and beta activity for 5-10 minutes.
3. Feedback Mechanism: Provide feedback using visual or auditory stimuli. Positive feedback occurs when theta decreases and beta increases.
4. Training Sessions: Conduct 20-30 minutes of training sessions, 2-3 times per week, for 20-40 sessions.
5. Progress Monitoring: Track progress using headache frequency, intensity diaries, and follow-up qEEG.
Alpha/Theta Training
This protocol focuses on increasing alpha (8-12 Hz) and theta (4-8 Hz) waves to promote relaxation and reduce anxiety, which are common migraine triggers.
- Target Brainwaves: Alpha waves (8-12 Hz) and Theta waves (4-8 Hz)
- Goal: Increase alpha and theta activity to reduce stress and improve emotional regulation.
Procedure:
1. Electrode Placement: Place electrodes at Fz and Cz (reference).
2. Baseline Recording: Record baseline alpha and theta activity for 5-10 minutes.
3. Feedback Mechanism: Use calming visual or auditory feedback. Positive feedback is provided when alpha and theta waves increase.
4. Training Sessions: Conduct 20-30 minutes of training sessions, 2-3 times per week, for 20-40 sessions.
5. Progress Monitoring: Monitor changes with headache frequency, intensity diaries, and follow-up qEEG.
Frequently used Neurofeedback Protocol for migraine management as follows:
Left-sided headaches – at C3 (T3)
- down-trained: 2-7 Hz and high-frequency beta
- up-trained: 15-18 Hz
Right-sided headaches – at C4 (T4)
- down-trained: 2-7 Hz and high-frequency beta
- up-trained: 12-15 Hz
The average number of neurofeedback sessions required for a significant change is 20-30. A person can get a neurofeedback session as often as twice a day with at least a two-hour break in between. It is recommended that a person try to do neurofeedback at least two or three times a week until the sessions are completed. Results appear to solidify and happen faster when done more frequently.
How effective is neurofeedback for migraines?
Neurofeedback for migraines can help with dysfunctions in the central nervous system, such as the increased excitability of the cerebral cortex. Because it works directly with the central nervous system, Neurofeedback training can be very effective in stabilizing the excitability of the cerebral cortex, which will result in reduced headaches, less sensitivity, and improvements in other symptoms associated with Migraines.
The researchers concluded that “Neurofeedback appears to be dramatically effective in abolishing or significantly reducing headache frequency in patients with recurrent migraines.”
Walker (Walker, J. E. (2011). QEEG‐Guided Neurofeedback for Recurrent Migraine Headaches. Clinical EEG and Neuroscience, 42(1), 59‐61. doi:10.1177/155005941104200112) examined the effects of neurofeedback therapy versus drug therapy in 71 patients with recurrent migraine headaches. After completing a quantitative electroencephalogram (QEEG) procedure, all results indicated an excess of high-frequency beta activity (21‐30 Hz).
Twenty‐five patients chose to continue with drug therapy for their recurring migraines, while 46 of the 71 patients selected neurofeedback training. Of those who decided on neurofeedback therapy, the majority (54%) reported complete abolishment of their migraines, 39% experienced a significant reduction in migraine frequency of greater than 50%, and 4% experienced a decrease of less than 50%. Only one patient did not report a reduction in headache frequency. The control group of participants who opted to continue drug therapy as opposed to neurofeedback experienced no change in headache frequency (68%), a reduction of less than 50% (20%), or a reduction greater than 50% (8%). Overall, the study demonstrates that neurofeedback is significantly effective in abolishing or substantially reducing the frequency of headaches in patients with recurrent migraines.
Effectiveness of Neurofeedback vs. Drug Management of the Migraine
Neurofeedback Effectiveness for Migraines
Drug Therapy Effectiveness for Migraines
After Neurofeedback for migraines, the reduction in the frequency and intensity of headaches was usually sustained at the 14.5-month follow‐up assessment.
Some of the benefits of neurofeedback for migraines:
- It helps to retrain the brain and optimize the functioning of the entire brain by removing barriers and improving the connections and brainwave activity in a certain region of the brain or among different regions.
- It releases old, stuck, or abnormal patterns to create new, more effective, stronger, and organized patterns.
- Training protocols are generated from the initial QEEG brain mapping. Training involves audiovisual feedback that INVOLUNTARILY teaches the individual to self-regulate the abnormal brain wave patterns presented to them on a computer screen in several ways.
- There are no contraindications or side effects of neurofeedback for migraines.
Effective Use of Various Biofeedback Modalities for Migraine Management
Various modalities of biofeedback, including Electromyography (EMG), Heart Rate Variability (HRV), Temperature, and Galvanic Skin Response (GSR), can also be effectively utilized in the management of migraines.
EMG biofeedback helps individuals become aware of and reduce muscle tension, which can alleviate headache symptoms.
HRV biofeedback trains individuals to regulate their heart rate variability, promoting autonomic balance and reducing stress, a common migraine trigger.
Temperature biofeedback involves monitoring peripheral skin temperature to enhance relaxation and decrease physiological arousal, thus helping to prevent migraines.
GSR biofeedback measures the skin’s electrical conductance, which varies with sweat gland activity, providing insights into stress and arousal levels. By learning to modulate these physiological responses, individuals with migraines can manage their symptoms more effectively, complementing traditional neurofeedback approaches. For more detailed information regarding various biofeedback modalities used in Migraine Management, please visit the Article “Biofeedback for Migraines. How to choose”.














Thank you so much!