
HRV Biofeedback Healing Mind & Body
Heart Rate Variability (HRV) Biofeedback has emerged as a promising therapeutic approach for managing various pathological states and disorders. This innovative technique, often called heart rate variability biofeedback, involves training individuals to consciously regulate their heart rate patterns through controlled breathing and mindfulness practices. By engaging in HRV biofeedback training, individuals can enhance their autonomic nervous system function, significantly improving mental and physical health. As research continues to unveil the benefits of HRV biofeedback, healthcare professionals increasingly recognize its potential in addressing a wide range of conditions, including anxiety, depression, chronic pain, and cardiovascular diseases. This article explores the efficacy of HRV biofeedback in treating these disorders and highlights its role in fostering overall well-being.
Table of Contents
Toggle- HRV Biofeedback Healing Mind & Body
- Stress-Proof Your Heart with HRV Biofeedback
- Physiology of Heart Rate Variability. Baroreflex.
- Physiology of Heart Rate Variability (HRV). Autonomic Nervous System
- The Role of the Sinoatrial Node and Interbeat Intervals
- HRV Biofeedback Training
- FAQs: HRV Biofeedback Healing Mind & Body
- HRV Biofeedback Home-Use Device
- HeartMath Inner Balance for Focus & Calm
- BioSignals 5 Biofeedback Sensors Device
As human beings age or suffer an illness, the total variability in heart rate is reduced, and the risk of illness and death increases. Several clinical findings show the importance of the changes in the heart’s rhythms. Decreased variability may predict sudden infant death. Lower variability in heart rate predicts a greater risk for further cardiac symptoms and death after a heart attack. Clinical depression also lowers heart rate variability and increases the risk of coronary artery disease. Heart rate variability has become a useful prognostic index or marker for morbidity and mortality.
Stress-Proof Your Heart with HRV Biofeedback
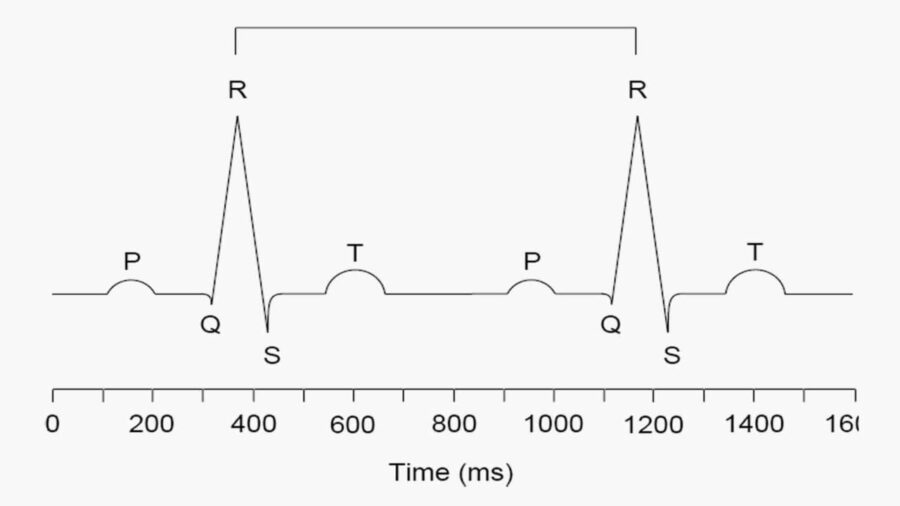
Heart rate variability refers to the changes in the interval or distance between one heartbeat and the next, measured in milliseconds. The interbeat interval (IBI) is the time between one R wave (or heartbeat) and the next, in milliseconds. The IBI is highly variable within any given period. HRV is typically quantified by measuring the interval between successive R-wave peaks (RR intervals) in the electrocardiogram (ECG).
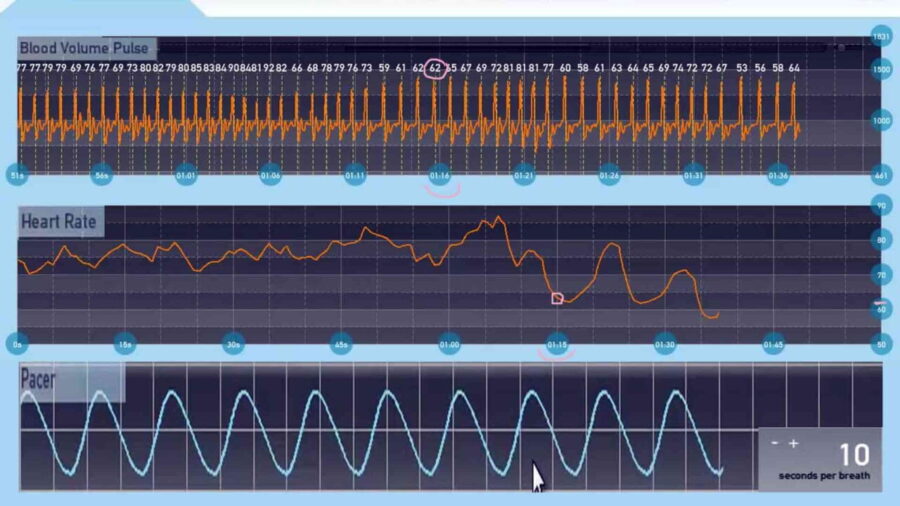
Regular exercise increases heart rate variability. Scientific studies on heart rate variability are relatively recent. Furthermore, only in the past ten years have researchers been able to train individuals to modify their heart rhythm variability through biofeedback training. Researchers subsequently labeled this cardiorespiratory intervention as HRV biofeedback, respiratory sinus arrhythmia (RSA) biofeedback, or resonance frequency feedback (RFF). The procedure of HRV biofeedback consists of feeding back the beat-by-beat heart rate data during slow breathing maneuvers so that the participant tries to maximize RSA.
Physiology of Heart Rate Variability. Baroreflex.
Breathing Frequencies and HRV Biofeedback
The Baroreflex and Its Effects
People can produce substantial increases in HRV through biofeedback because of ‘‘resonance’’ characteristics in the cardiovascular system. HRV biofeedback training stimulates a particular reflex in the cardiovascular system with a certain rhythm. It is called the ‘‘baroreflex,’’ and it helps to control blood pressure. It also helps to prevent emotional reactivity and promotes breathing efficiency. The baroreflex mediates through the nucleus tractus solitarii, located in the brainstem. This center communicates directly with the amygdala, a center for emotional control, in a pathway extending through the insula. Perhaps it is for this reason that various studies have shown positive HRV biofeedback effects for treating anxiety, phobias, and depression.
When blood pressure goes up, the baroreflex causes the heart rate to go down, and when blood pressure goes down, the heart rate goes up. This causes a rhythm in heart rate fluctuations. The baroreflex system resonates when a person breathes at this exact rhythm (which varies among people, generally between 4.5 and 6.5 times a minute).
How do we find the frequency at which the baroreflex system resonates for each person?
This frequency will produce the most significant swings in heart rate between inhaling and exhaling. To see this frequency, a person should try to breathe at various rates per minute to find the exact frequency at which the cardiovascular system resonates. This will be his/her resonance breathing frequency. This frequency varies from individual to individual, but it is approximately 0.1 Hz or six breaths per minute. The baroreflex system is stimulated and strengthened when people breathe at this frequency. Through projections to other systems in the body (e.g., inflammatory and limbic systems), different events occur that produce the many beneficial effects of HRV biofeedback.
The Role of Breathing in Enhancing Baroreceptor Sensitivity and HRV
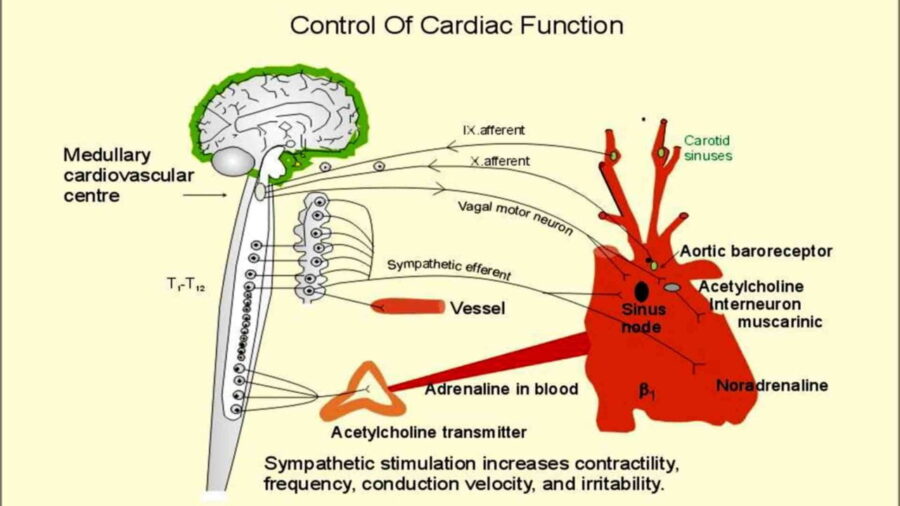
Breathing becomes a natural way to provide external stimulation to increase HRV. Conversely, each breath then stimulates the baroreflex. The baroreflex involves blood pressure sensors called baroreceptors in the aorta and carotid artery. These sensors help modulate fluctuations in blood pressure. Cardiopulmonary and blood pressure sensors (baroreceptors) detect respiratory changes in cardiac filling and arterial pressure. Baroreceptors in the walls of these arteries detect stretching of the arteries as blood pressure increases and signal to the Sinoatrial Node via the parasympathetic nervous system to slow down the heart.
When blood pressure increases, the baroreflex causes immediate decreases in heart rate. As the blood pressure falls, the baroreflex causes immediate increases in heart rate through the sympathetic nervous system. We refer to the ability of blood pressure changes to regulate heart rate as Baroreceptor Sensitivity.
Physiology of Heart Rate Variability (HRV). Autonomic Nervous System
The Influence of the Autonomic Nervous System on Heart Rate Variability
Although numerous physiological and environmental factors influence heart rate variability (HRV), two are particularly prominent and psychophysiologically influential: the influence of the Autonomic Nervous System (ANS) on cardiac activity and the regulation of the ANS by the central autonomic network (CAN). The heart receives innervation from the ANS’s sympathetic and parasympathetic (vagal) branches. These branches exert regulatory influence on heart rate by affecting the activity of the heart’s primary pacemaker, the sinoatrial node.
The Role of the Sinoatrial Node and Interbeat Intervals
The sinoatrial node generates action potentials that travel throughout the cardiac tissue, causing the myocardium (heart muscle) to contract in an orchestrated manner characteristic of a heartbeat. Activation of sympathetic fibers excites the firing rate of the sinoatrial node, resulting in an increased heart rate. In contrast, parasympathetic activation inhibits the pacemaking activity of the sinoatrial node, leading to a decreased heart rate. Essentially, these two autonomic branches regulate the lengths of time between consecutive heartbeats or interbeat intervals (IBI).
Faster heart rates correspond to shorter interbeat intervals, while slower heart rates correspond to longer intervals. The parasympathetic nervous system (PNS) and sympathetic nervous system (SNS) act antagonistically to influence cardiac activity. For example, an increased heart rate may arise from heightened sympathetic activity or decreased parasympathetic inhibition (vagal withdrawal).
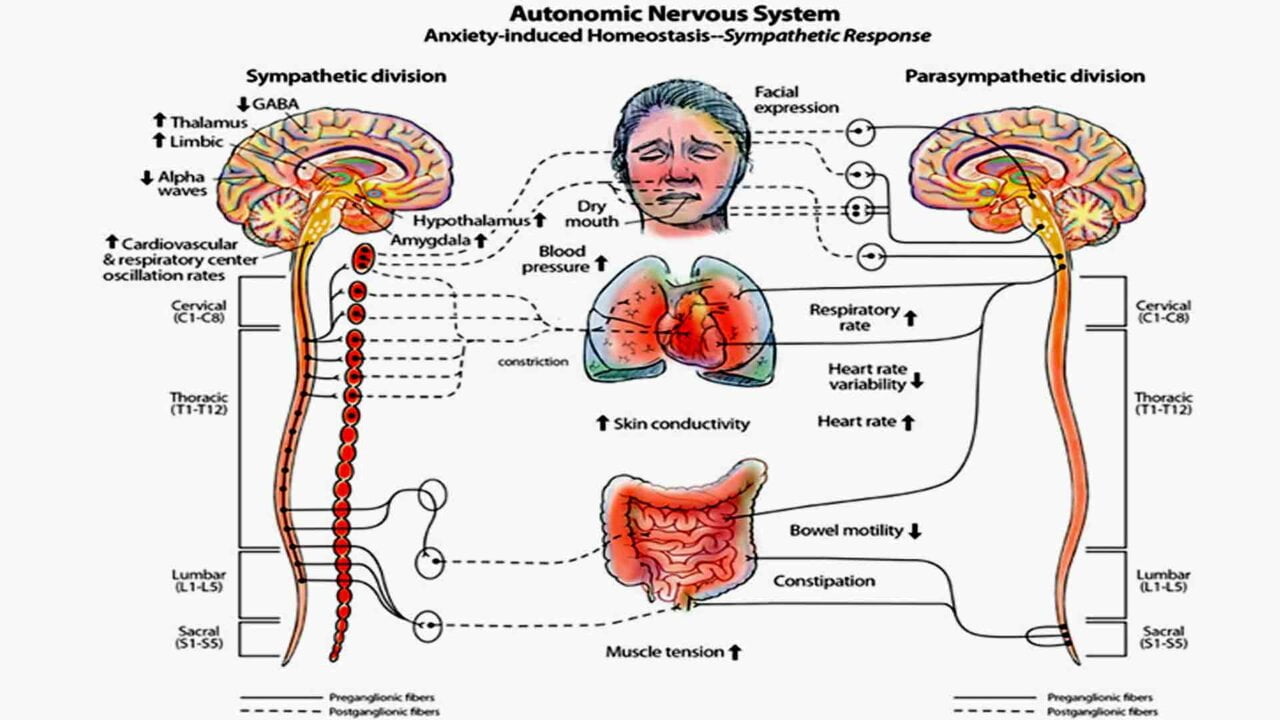
The Central Autonomic Network’s Role in Cardiac Regulation
During physical or psychological stress, the activity of the SNS dominates, producing physiological arousal to help adapt to challenges, which results in an increased pulse or heart rate. Conversely, during relative safety and stability periods, the PNS maintains lower physiological arousal and a decreased heart rate. The ease with which an individual transitions between high and low arousal states largely depends on the ANS’s ability to vary heart rate rapidly. Specifically, a flexible ANS enables quick modulation of physiological and emotional states in response to situational demands. Furthermore, the Central Autonomic Network (CAN) remotely regulates the autonomic influences on heart rate. It integrates physiological responses into emotional expression while responding to environmental demands, facilitating goal-directed behavior, and supporting homeostatic regulation.
HRV Biofeedback Training
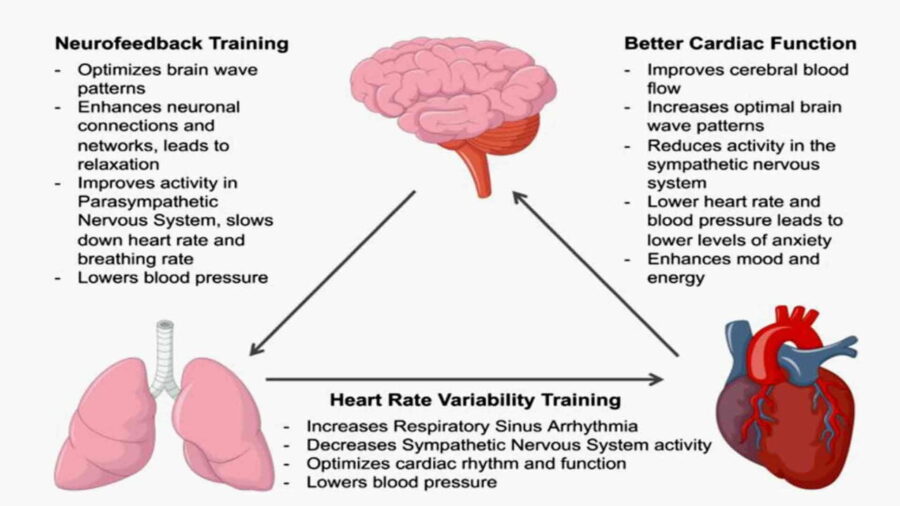
Mechanisms of Heart Rate Variability During Biofeedback Training
During HRV biofeedback training, the amplitude of heart rate oscillations grows to the amplitude at rest many times, while the pattern becomes sinusoidal and straightforward. This pattern occurs in almost everyone and is often achievable within a fraction of a minute, even in persons previously exposed to the technique. The mechanism for this effect lies in a confluence of processes:
(1) phase relationships between heart rate oscillations and breathing at specific frequencies,
(2) phase relationships between heart rate and blood pressure oscillations at specific frequencies,
(3) the activity of the baroreflex and
(4) resonance characteristics of the cardiovascular system.
Optimizing Heart Rate Variability Through Breathing Techniques
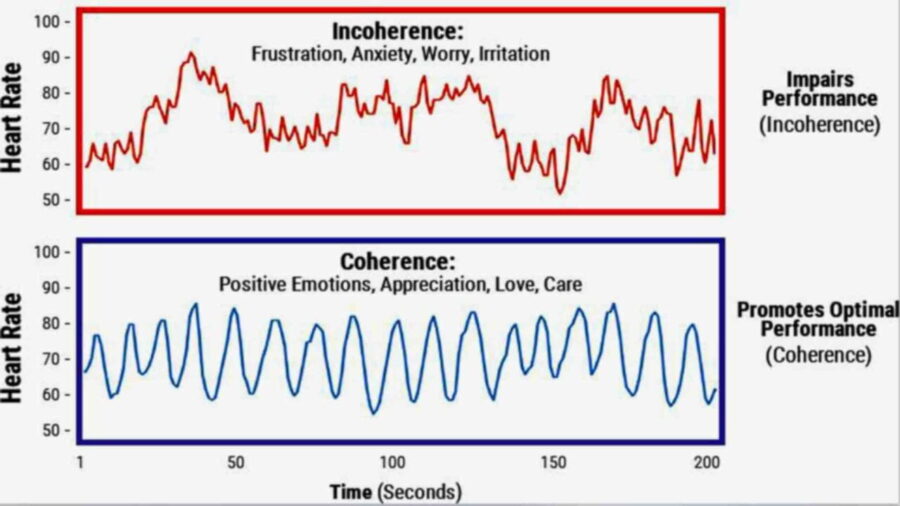
HRV Biofeedback training can focus on increasing the total HRV in a specific frequency range. Increasing the heart rate change in the Low-Frequency Range (LF) appears optimal. For most persons, resonant frequency involves dominance of heart rate change in the Low-Frequency range, around 0.1 Hz. This 0.1 Hz frequency is most frequently produced by persons in a relaxed mental state, with a positive emotional tone, breathing diaphragmatically at a rate of about 5-7 breaths per minute. Relaxed breathing at six breaths per minute produces a spike in heart rate variability at 0.1 Hz. The amplitude of variation increases because the baroreceptors’ effects on heart rate combine with the effects of slow breathing. Researchers have long recognized a systematic relationship between HRV amplitude and breathing frequency, showing that slower respiration leads to higher amplitudes.
HRV Biofeedback’s Impact on Respiratory and Gastrointestinal Disorders
HRV biofeedback is a powerful intervention for asthma. Research data show that the HRV BFB participants reported fewer symptoms and better lung function, with no medication boosts.
In recent years, much progress has been made in understanding the enteric nervous system and its autonomic regulation. Research has shown that six-per-minute breathing maneuvers dramatically affect esophageal pain thresholds. Improvement was mediated by the restoration of vagal tone, presumably influenced by the HRV BFB. A recent study from the U.K. compared hypnosis to HRV BFB for irritable bowel syndrome. Both groups showed nice improvements, with the HRV BFB group reporting slightly more symptom reduction.
Broader Applications of HRV Biofeedback in Cardiology and Mental Health
There is promising literature on using HRV biofeedback for various cardiologic disorders. Within cardiology, it is increasingly recognized that balancing SNS and PNS activity is a crucial component of cardiac health. Exciting data show that HRV biofeedback impacts the heart muscle itself. Biofeedback in treating essential hypertension is well-known within the field.
A recent study in Germany has shown that adding HRV biofeedback to traditional back exercises and trigger point release produced the most significant pain relief in back pain patients. The mechanism hypothesized to be in play for “trigger points” (TPs) is known as “accentuated antagonism.” Good autonomic balance allows the PNS to govern the SNS in non-emergency situations. Therefore, the use of HRV biofeedback may be effective by blocking some of the sympathetic overflows to TPs.
Few studies show promise for conditions such as pregnancy-induced hypertension and preterm labor: the HRV BFB group had almost two weeks added gestation period with significantly heavier babies.
There have been several studies showing decreased depression levels with HRV biofeedback, including cases where the depression was secondary to trauma or anxiety.
The relevant literature shows that heart rate variability is associated with emotions and thoughts; the literature also indicates that self-regulation training incorporating HRV biofeedback can improve behavior and, in turn, improve cognitive regulation of emotions.
FAQs: HRV Biofeedback Healing Mind & Body
HRV refers to the variation in time between heartbeats. A higher HRV indicates a more flexible and resilient nervous system, which is associated with improved stress management, emotional balance, physical health, sport performance, and longevity.
HRV (Heart Rate Variability) biofeedback is a technique that helps individuals train their autonomic nervous system by monitoring and improving their heart rate variability. It involves breathing at a specific pace to increase coherence between the heart, brain, and respiration, promoting relaxation and emotional regulation.
HRV biofeedback has been used to support the treatment of conditions like anxiety, depression, PTSD, chronic pain, hypertension, insomnia, and cardiovascular disorders. It is also used for performance enhancement in sports and professional settings.
Many users notice benefits after just a few sessions, such as feeling more relaxed or sleeping better. However, significant improvements in HRV and long-term health often require regular practice over 4–8 weeks or more.
Ideally, HRV biofeedback should be practiced 5–15 minutes a day, several times a week. Consistency is key for lasting improvements in autonomic regulation and emotional resilience.
HRV Biofeedback Home-Use Device
Heart rate variability biofeedback has enjoyed considerable popularity in recent years. Several commercial products have been introduced, ranging in price from $80 to over $200.
The HRV biofeedback equipment should have a sensor to measure heart rate (variability) with an electrocardiogram (ECG) or Blood Volume Pulse (BVP) and a respiration sensor by using a breathing belt.
- All
- Back
- EMG Biofeedback Device
- Temperature Biofeedback Device
- Electrodermal Activity Biofeedback Device
- HRV Biofeedback Device
- Breathing Biofeedback Device
- Posture Corrector Device




