Living with multiple sclerosis (MS) is challenging enough, but when depression in MS adds another layer of struggle, it can feel overwhelming. Studies show that nearly 50% of people with MS experience depression at some point—a rate much higher than the general population. The connection between MS and depression isn’t just emotional; it’s neurological, with inflammation and brain changes playing key roles. But there’s hope. From neurofeedback for MS to tailored therapy and medication, effective treatments exist. Understanding the link between multiple sclerosis and depression is the first step toward better mental health—because managing MS means caring for both body and mind.
Table of Contents
Toggle- What Is the Link Between Multiple Sclerosis and Depression?
- Why Does Depression in MS Happen?
- Common Symptoms of Depression in MS
- How MS-Related Depression Differs from General Depression
- Impact of Depression on MS Progression & Quality of Life
- Effective Treatments for Depression in MS
- Treatments for Encouraging Myelin Repair in MS Depression
- Neurofeedback for MS: Can It Help with Depression?
- Neurofeedback Protocols Used in MS
- Neuromodulation Variants: fNIRS & Light-Based Therapies
- Neurofeedback & Light-Based Brain Training for MS: Can It Help with Depression?
- Complementary Therapies & Lifestyle for MS and Depression Treatment
- Frequently Asked Questions (FAQ) about MS and Depression
- Conclusion: Moving Forward with Hope in MS and Depression
- Neurofeedback Home-Use Device for MS Depression Management
- References
What Is the Link Between Multiple Sclerosis and Depression?
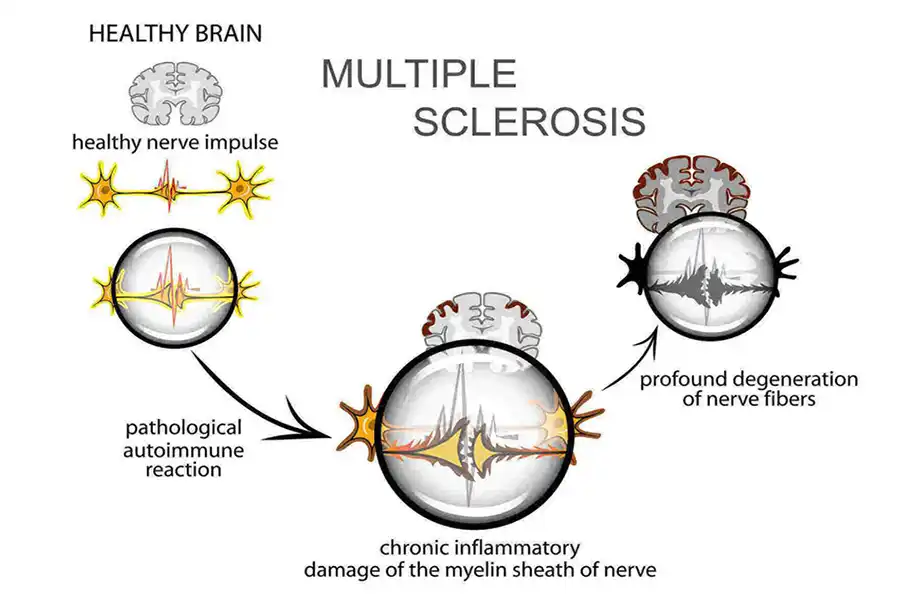
Multiple Sclerosis (MS) is a chronic neurological condition that affects the central nervous system, often causing a wide range of physical and cognitive symptoms. One of the lesser-discussed — yet highly significant — challenges of living with MS is depression.
In fact, people with MS are two to three times more likely to experience depression compared to the general population. This is not simply a psychological reaction to the diagnosis or physical limitations. Instead, depression in MS is often a direct result of the disease’s impact on the brain and nervous system.
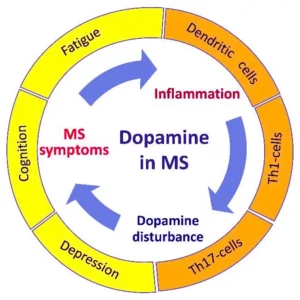
Research has shown that MS can cause lesions in areas of the brain that regulate mood, such as the prefrontal cortex and limbic system. These structural changes may interfere with the brain’s ability to manage emotions, leading to increased vulnerability to depression. Furthermore, the immune system’s activity and chronic inflammation associated with MS may also contribute to the alteration of mood-regulating neurotransmitters, such as serotonin and dopamine.
Depression in MS is more than just feeling sad. It’s a serious medical condition that can worsen fatigue, reduce motivation, and affect treatment adherence — ultimately impacting the course of the disease and the person’s overall quality of life.
Recognizing the strong link between MS and depression is the first step toward effective management. In the sections that follow, we will explore why depression happens in MS, how to recognize the symptoms, and what you can do to improve mental well-being alongside managing MS.
Key Insights
People living with Multiple Sclerosis (MS) frequently face emotional challenges—one of the most significant is depression. This chapter helps you understand the direct links so you can recognize and address them early.
- High prevalence: Up to 50% of individuals with MS experience clinical depression at some point—almost twice the rate in the general population
- Brain structure effects:
- MRI studies show lesions and atrophy in mood-regulating regions (prefrontal cortex, temporal lobe, hippocampus) in MS patients with depression
- Disrupted connectivity between the amygdala and prefrontal cortex reduces emotional resilience
- Neuroinflammation plays a significant role:
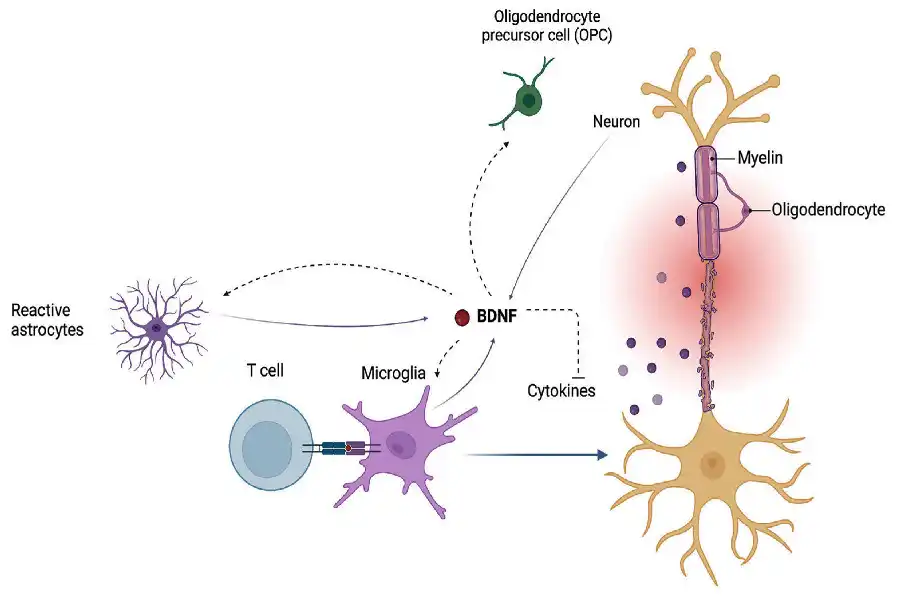
- MS-induced inflammation activates microglia and pro-inflammatory cytokines (IL 1β, IL 6, TNF α), leading to synaptic dysfunction in mood centers
- This triggers glutamatergic imbalance and neuronal hyperexcitability, particularly in the limbic system.
- Neuro-immune cross-talk:
- Shared mechanisms involve Th17 cell activation seen in both MS and depression
- Altered serotonin and dopamine regulation affects immune responses and mood
Why Does Depression in MS Happen?
Understanding the root causes is the first step to finding effective relief. When living with MS, feeling low isn’t just about stress—fundamental changes in your brain, body, and life can cause it. Here’s a deeper look:
1. Biological Factors
- Genetic vulnerability: Some people inherit traits that make them more likely to get depressed. If you have a family history of depression, your chance increases. A model called “diathesis–stress” explains this: a built-in sensitivity interacts with life stress to trigger depression
- Brain changes from MS: MS causes damage in regions that regulate mood, like the prefrontal cortex and limbic system. This can make it harder to feel happy or manage stress.
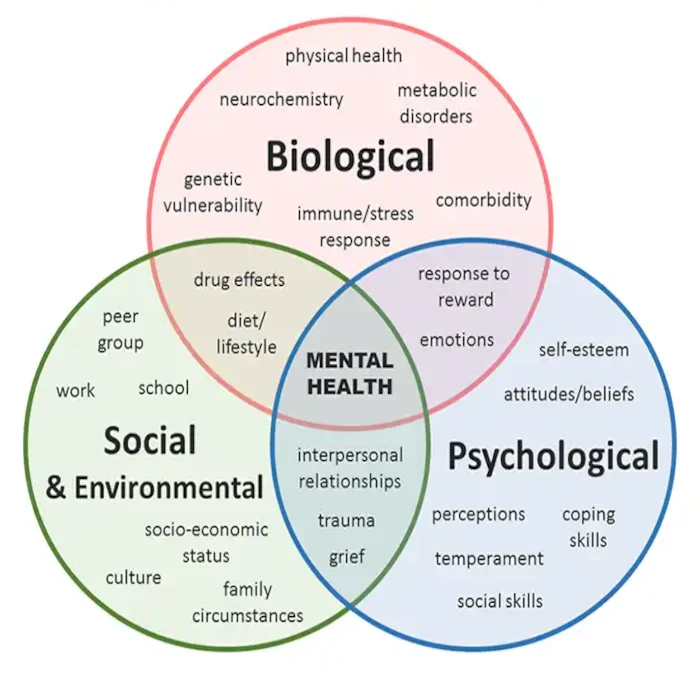
- Chronic inflammation: MS causes immune cells to release chemicals (cytokines) that can reach the brain and dampen mood-boosting neurotransmitters like serotonin and dopamine.
2. Psychological Triggers
- Stress overload: Getting diagnosed with MS or facing a relapse can be intensely stressful. For someone already vulnerable, this stress can “flip the switch” and cause depression.
- Emotional toll: Adjusting to reduced physical ability, losing independence, or coping with uncertainty can lead to grief, anxiety, and hopelessness—fueling depression.
3. Social & Lifestyle Pressures
- Isolation: MS can limit your ability to go out, stay active, or connect socially. Feeling disconnected often leads to loneliness and low mood.
- Economic strain: Medical bills, lost income, and career worries add stress—making it harder to stay positive.
Common Symptoms of Depression in MS
Emotional & Cognitive Signs
Understanding and identifying depression in MS isn’t easy—many symptoms mimic the condition itself. But recognizing these patterns can help you get the proper support sooner.
Persistent Sadness or Hopelessness
- Feeling sad, “empty,” or desperate most days for at least two weeks.
- Often described as a deep emotional pain that stays even on good days.
- This is a key symptom of clinical depression—even when MS is the underlying condition
Loss of Interest
- Activities that once brought joy—hobbies, work, social events—feel meaningless or exhausting.
- This “blanking out” effect of depression robs you of motivation and pleasure.
Difficulty Concentrating or Learning
- Struggling to pay attention, remember things, or make decisions, even minor ones.
- Depression worsens MS-related “brain fog,” making simple tasks feel overwhelming.
Feelings of Guilt or Worthlessness
- Feeling like a burden, blaming yourself for “not doing enough”—even when it’s untrue.
- Such negative thoughts may spiral and fuel more profound sadness.
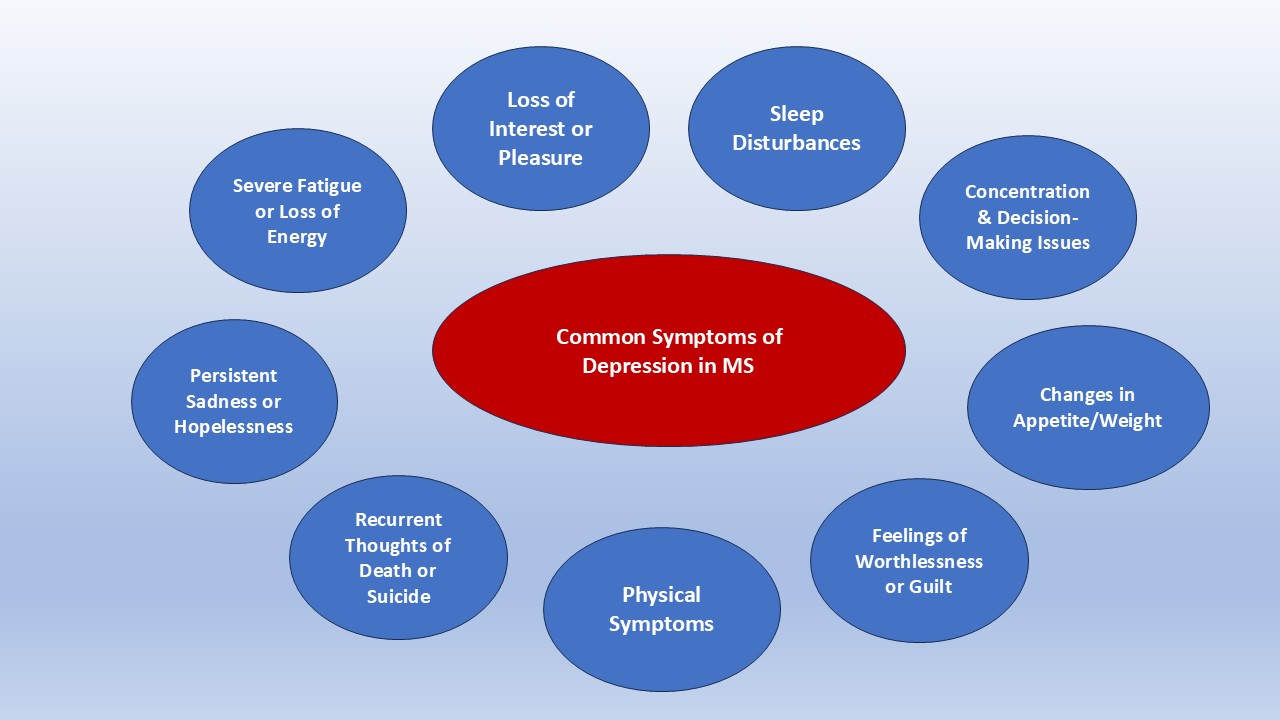
Physical & High-Risk Indicators
Changes in Eating or Weight
- Either losing your appetite or eating more than usual for no apparent reason.
- These changes can lead to noticeable weight fluctuations.
Physical Aches or Restlessness
- Unexplained pain, body aches, tension, or moving more slowly than usual.
- These physical symptoms may mask depression because they overlap with MS
Overwhelming Fatigue
- Feeling exhausted even after a whole night’s sleep or rest.
- Happens in up to 90% of people with MS, and worsens when depression is present.
- Unlike regular tiredness, it’s persistent and can make everyday tasks feel monumental.
Sleep Problems
- Trouble falling asleep or staying asleep (insomnia), or sleeping too much (hypersomnia).
- Over half of people with MS experience sleep disturbances, which often co-occur with fatigue and depression.
Suicidal Thoughts or Self-Harm
- Recurring thoughts about death, wishing you weren’t around, or planning self-harm.
- MS patients have up to 7 times higher risk of suicide than the general population—this is a medical emergency.
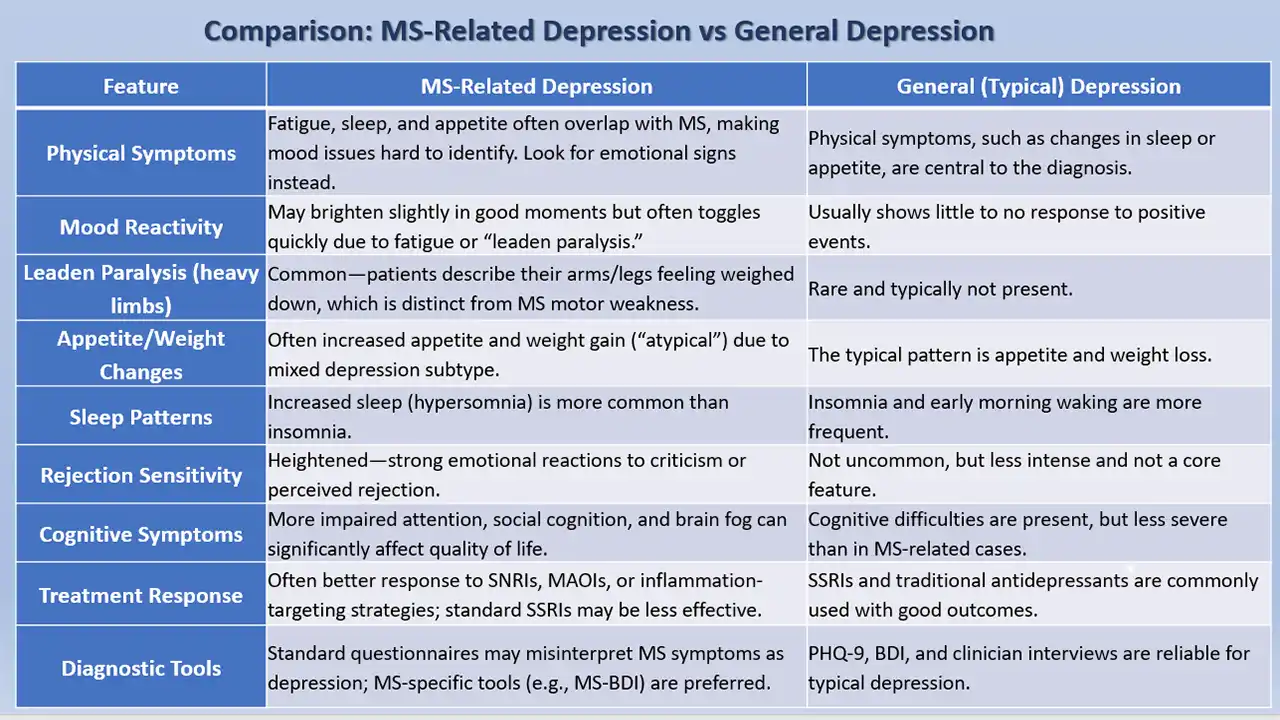
How MS-Related Depression Differs from General Depression
Depression in Multiple Sclerosis often looks like general depression—but with key differences that affect diagnosis and treatment. Understanding these helps you and your doctors find the proper support faster.
Overlapping Physical Symptoms
- Shared signs with MS—such as fatigue, poor sleep, and appetite changes—can mask or mimic depression. This makes it difficult to tell whether symptoms are due to MS progression or true major depression
- Clinicians often focus on emotional symptoms—like persistent sadness, hopelessness, or negative beliefs—rather than general physical complaints, to avoid misdiagnosis.
Mixed or Atypical Symptom Patterns
- People with MS are more likely to have a mixed atypical melancholic subtype, showing weight gain, heavy limbs (“leaden paralysis”), and irritability—symptoms less common in general depression
- This mixed presentation can confuse diagnosis, as it’s not the classic picture of sadness, sleep change, or interest loss typically seen in major depression
Neuropathology & Inflammation Roots
- Unlike general depression, MS-related depression is often tied to inflammation, demyelination, and specific brain lesions—in areas like the frontal or temporal lobes—that disrupt mood circuits
- Neuroendocrine changes—such as abnormal cortisol levels and HPA axis dysfunction—are also more common in MS-related depression
Diagnostic Challenge & Screening Tools
- Standard depression questionnaires may give false positives in MS, because they can’t separate physical symptoms due to MS from mood issues
- To improve accuracy, doctors use MS-specific tools like the MS BDI (Beck Depression Inventory for MS) or focus questions on core emotional symptoms like mood and loss of interest
Treatment Implications
- With mixed or atypical symptoms, antidepressants like MAOIs or SNRIs may work better than SSRIs for some MS patients.
- Inflammation-reducing treatments and disease-modifying therapies may directly improve mood — something not seen in typical depression.
Impact of Depression on MS Progression & Quality of Life
Untreated depression in MS can make the disease itself harder to manage and seriously affect daily living. Here’s how:
Lower Treatment Adherence
- Depression drains motivation: When you’re depressed, it’s harder to keep up with injections, pills, and doctor visits.
- Studies show that people with both MS and depression are around half as likely to stay on prescribed disease-modifying therapies (DMTs) compared to those without depression
- Those who follow antidepressant treatment for at least six months tend to have better adherence to MS meds, showing the power of treating both conditions
Faster MS Progression & Higher Relapse Risk
- Skipping DMTs or half-heartedly following the regimen = more relapses and brain lesions. Regular treatment helps control relapses and delay disability .
- Depression also worsens pain and fatigue, both of which are associated with more disability and quicker progression
Decline in Quality of Life
- Depression amplifies MS challenges—like brain fog, pain, and social withdrawal.
- Individuals facing both report lower quality of life, more days missed from work, and more negative social impact
- It also interrupts healthy habits: exercise, balanced diet, sleep routine, and meaningful connection—all essential to maintain well-being .
Social & Economic Consequences
- Depression contributes to unemployment, loss of financial stability, and reduced access to care .
- Less social support and more profound isolation make coping even harder and can further spiral mood and health .
Effective Treatments for Depression in MS
Treating depression in MS patients requires a well-rounded approach—combining medications, therapy, lifestyle adjustments, and sometimes advanced techniques like neurofeedback. Here’s a detailed guide:
Medications (Pharmacotherapy)
- SSRIs (Selective Serotonin Reuptake Inhibitors)
- First-line treatment (e.g., sertraline, paroxetine, fluvoxamine).
- Well tolerated and effective in MS; sertraline is often the preferred starting option
- SNRIs & Other Antidepressants
- SNRIs (like duloxetine) or tricyclics/MAOIs are usually second-line—used when SSRIs don’t work.
- However, some SNRIs may worsen fatigue or interact with MS medications
- Tailored choices
- Sedating medications can worsen fatigue. Anticholinergic drugs may impact thinking, so doctors often choose medicines based on your MS symptoms .
Psychological Therapies
- Cognitive Behavioral Therapy (CBT)
- Proven effective for reducing depression. Targets negative thought cycles and develops new coping skills
- Mindfulness-Based Therapies (Mindfulness-Based Stress Reduction, Mindfulness-Integrated CBT)
- Several small trials show improvements in mood, stress, fatigue, and emotional regulation .
- Other psychological programs
- Education groups, dialectical behavior therapy, or social-cognitive training have potential benefits
Lifestyle & Self-Care Strategies
A meta-review emphasizes lifestyle changes as powerful allies in depression care for MS patients:
- Regular physical exercise
- Activities like walking, swimming, resistance, or aquatic therapy reduce depressive symptoms, fatigue, and enhance mood
- Diet and nutrition
- Emerging evidence suggests that a balanced diet (e.g., ketogenic), sufficient vitamin D, probiotics, and anti-inflammatory foods may help .
- Mind-body practices
- Yoga, meditation, breathing exercises, positive affirmations, and support groups enhance psychological resilience
- Stress reduction and boundaries
- Principles like “learning to say no”, pacing activities, and stress management are frequently recommended by MS communities .
Integrated Treatment Approach
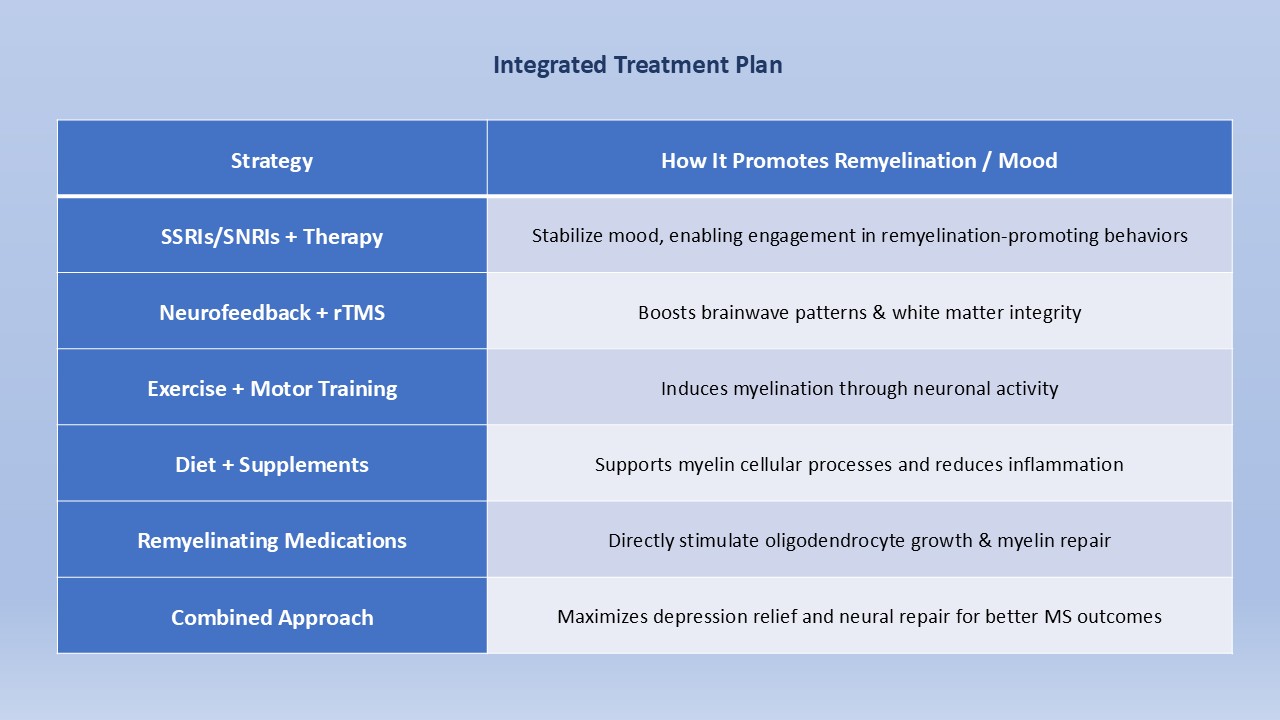
Guidelines recommend a combined strategy—personalizing treatment according to individual MS and depression profiles.
- Begin with SSRIs or SNRI if needed.
- Add CBT and/or mindfulness therapy.
- Implement lifestyle changes (exercise, diet, stress reduction).
- Consider neurofeedback if symptoms persist.
- In severe, treatment-resistant cases, newer options like neurostimulation (e.g., rTMS, tDCS) may be evaluated—not yet standard for MS-related depression.
Treatments for Encouraging Myelin Repair in MS Depression
Treating depression in MS can be supercharged by focusing not only on symptom relief but also on promoting remyelination and brain neuroplasticity. Here’s how combining traditional treatments with remyelination strategies can improve mood and resilience:
Why Remyelination Helps Depression
- Myelin repairs neural communication: By restoring the myelin sheath around axons, brain circuits function more smoothly—improving cognition, fatigue, and emotional regulation.
- Neuroplastic rewiring: When the brain remyelinates, it builds new pathways, helping reshape circuits involved in mood, stress resilience, and thought patterns.
- Emotion regulation boost: Stronger, more efficient neural connections mean better control over emotions—reducing depressive symptoms.
Neurofeedback, Biofeedback & Brain Stimulation
- EEG neurofeedback trains individuals to self-modulate brainwave patterns—often increasing beta (focus) and decreasing theta. Trials show it not only reduces depression/fatigue in MS patients but also enhances white matter integrity, suggesting remyelination and neuroplasticity.
- fMRI neurofeedback supports structural changes: adults trained to regulate motor cortex activity showed measurable increases in white matter tracts like the corpus callosum
- Non-invasive brain stimulation (rTMS/tDCS) promotes growth of oligodendrocytes and myelin formation—animal studies show remyelination, human MS studies show improved cognition and fatigue.
Physical Activity & Motor Training
- Exercise-induced remyelination: Aerobic and motor learning regimens stimulate oligodendrocyte precursor cells, increasing myelin protein, axon density, and white matter integrity.
- Motor rehabilitation improves brain structure and mood—helps with neuroplastic changes, fatigue reduction, and emotional well-being.
Diet & Supplementation
- Vitamin D, omega-3s, ketogenic diets, and intermittent fasting can aid myelin repair and brain metabolism.
- These dietary strategies support brain plasticity and may both soothe mood and promote remyelination.

Remyelinating Medications & Agents
- Clemastine fumarate (an antihistamine) has shown remyelination in clinical trials for optic neuropathy and mouse models
- Clemastine’s benefits are linked to improved nerve conduction and fatigue reduction—though some trials showed mixed outcomes.
- GSK239512 (an H3 antagonist) promotes oligodendrocyte development and improves myelin integrity in relapsing MS
- RXR agonists (e.g., bexarotene, acitretin) stimulate myelin-producing cells and show remyelination in preclinical models
- Emerging drugs like sobetirome, thyroid hormone analogs, ellagic acid, and GD1a promote OPC differentiation and remyelination
- Deep brain stimulation (DBS) and non-invasive methods may modulate neural activity to encourage remyelination—still under study.
Neurofeedback for MS: Can It Help with Depression?
Neurofeedback is a promising brain-training method that could boost emotional health and brain structure in people with MS. Here’s how and why it works:
What Is Neurofeedback?
- How it works: You wear a non-invasive EEG cap that monitors your brainwaves. Visual or audio signals provide real-time feedback, encouraging you to shift brainwave patterns toward healthier states (e.g., boosting beta, reducing theta).
- Goal: Train your brain to self-regulate mood, stress, attention, and calmness—without relying solely on medication
How Neurofeedback Relieves Depression
- Enhances emotional control by strengthening brain networks involved in mood regulation (e.g., prefrontal cortex, amygdala).
- Improves cognitive function like memory and processing speed—benefiting daily life
- Reduces negative thinking loops and increases psychological resilience—helping break out of depressed states.
Neurofeedback in MS Patients
- A randomized trial with 24 MS patients (16 neurofeedback sessions) showed significant improvements in both depression and fatigue, with effects lasting at least two months.
- A pilot MRI study found that neurofeedback led to improved white matter integrity (higher fractional anisotropy) and functional brain connectivity in MS patients—suggesting it may promote remyelination or stronger neural connections
- Additional studies report better balance, fatigue, and quality of life after neurofeedback training in MS.
- Reviews from 2021 suggest neurofeedback may alleviate depression, anxiety, pain, and cognitive deficits in MS—even though protocols vary.
Promoting Neuroplasticity and Remyelination
- Neurofeedback triggers Hebbian learning: “neurons that fire together wire together,” strengthening brain circuits and boosting white matter integrity (myelin).
- Improved connections in the corticospinal tract and anterior thalamic radiation align with better cognitive control and mood—clear markers of brain repair.
- As your neural wiring improves, signal transmission becomes smoother—enhancing fatigue management, emotional stability, and reducing depressive symptoms.
Neurofeedback Protocols Used in MS
Theta/Beta Ratio Reduction
Study: Keune et al. (2019) randomized MS patients for a two-week neurofeedback intervention over five sessions.
Protocol: Measured frontal EEG (Fz vs. mastoid references), trained participants to reduce the theta/beta ratio (theta: 4–7 Hz; beta: higher frequency) with real-time visual feedback.
Outcome: State-wise reductions in theta were observed during training, indicating a potential for improved processing speed.
SMR (Sensorimotor Rhythm) Uptraining
Study: Kober et al. (2019) delivered home-based neurofeedback (10 sessions over 3–4 weeks) to MS patients.
Protocol: Focused on increasing SMR amplitude (12–15 Hz) from the Cz electrode, with visual feedback.
Outcome: Participants demonstrated improvement in long-term memory and executive function tasks, indicating cognitive enhancement through neuroplasticity.
EEG Neurofeedback Enhancing Hypnotic Analgesia
Study: Jensen et al. (2015) pilot study involving individuals with MS and chronic pain.
Protocol: Five sessions of left-anterior theta (NF-HYP) neurofeedback preceding hypnosis versus relaxation control.
Outcome: Those receiving NF-HYP saw a greater reduction in pain, highlighting the unity between neurofeedback and hypnosis.
Cognitive Rehabilitation via Neurofeedback (Review Analysis)
Review: Vilou et al. (2023) surveyed EEG neurofeedback protocols employed across neurological conditions, including MS.
Protocols Described:
- Theta/Beta Ratio Training – As above, aiming to optimize attention and processing speed.
- SMR Training (12–15 Hz) – Enhances sensorimotor function and cognitive control.
- Slow Cortical Potential (SCP) and Coherence Training – Used less frequently but focus on long-term cortical state modulation and inter-regional connectivity improvements.
Broader Non-MS Protocols (Adaptable Strategies)
While not MS-specific, these are relevant as potential extensions:
- Alpha–Theta Training: Induces a relaxed, meditative state—applicable for stress and mood regulation.
- Low-Beta Training (15–18 Hz): Helps reduce muscle tension/spasticity and pain.
- Cognitive Enhancement: Training that targets attention, working memory, and processing speed (via tailored frequency bands).
Neuromodulation Variants: fNIRS & Light-Based Therapies
You inquired about two newer approaches: fNIRS-based neurofeedback (similar to Mendi) and flashing-light systems (such as NeuroVIZR). Here’s what the current evidence says:
fNIRS Neurofeedback (e.g., Mendi)
- What is it?
Functional near-infrared spectroscopy (fNIRS) measures blood oxygen levels in the cortex and can be used for real-time feedback. In neurofeedback, users learn to consciously regulate oxygenation in targeted brain regions. - Early evidence:
- A study using fNIRS neurofeedback showed healthy participants could up-regulate prefrontal oxygen signals, improving working memory task performance afterward.
- Another study using motor imagery showed reliable activation of motor cortex regions via fNIRS feedback.
- Limitations to note:
- No robust trials in MS or depression populations yet.
- No studies directly evaluating the Mendi headband’s effectiveness; clinical experts raise doubts about its claimed benefits.
Bottom line: fNIRS neurofeedback shows promise in guided brain activation and may aid neuroplasticity, but lacks direct evidence for MS-related depression at this time.
Light-Based Therapy (NeuroVIZR & Similar Devices)
- How it works:
Uses rhythmic LED light pulses (1–40 Hz) and synchronized sound to entrain the brain’s electrical activity toward desired states like relaxation, focus, or sleep.
Known as audiovisual entrainment (AVE), it gently “nudges” brainwaves via photic stimulation. - Reported benefits:
- Users and small observational studies report reduced stress, improved sleep quality, enhanced focus, and better mood after sessions.
- Reddit accounts describe improved relaxation, sleep regulation, and daily routine support—often combined with other modalities.
- Neuroplastic and myelin implications:
- Principles of entrainment suggest repeated light stimulation creates new neural pathways and strengthens connectivity—potentially aiding remyelination through activity-dependent mechanisms.
- While there’s no MS-specific study yet, AVE has shown increased cerebral blood flow and neurotransmitter changes, key processes in plastic repair.
Neurofeedback & Light-Based Brain Training for MS: Can It Help with Depression?
Exploring brain training methods—including EEG/fNIRS neurofeedback, flashing red/NIR light, and audiovisual entrainment (AVE)—reveals new ways to support mood and brain repair in MS.
Neurofeedback: EEG & fNIRS
- EEG-based neurofeedback uses brainwave feedback to help you consciously shift patterns like increasing beta (focus) and reducing theta (drowsiness)—a method shown to reduce depression and fatigue in MS with benefits lasting at least two months
- fNIRS neurofeedback (e.g., Mendi) monitors blood oxygen in the prefrontal cortex. A pilot study found that eight sessions strengthened connectivity and self-regulation networks, suggesting that this supports emotional control.
- Both EEG and fNIRS methods encourage neuroplasticity—reinforcing healthy mood circuits and potentially promoting remyelination through activity-dependent brain change.
Flashing Light & Audiovisual Entrainment (NeuroVIZR)
- Systems like NeuroVIZR combine flashing red/NIR light and sound, harnessing audiovisual entrainment (AVE) to “tune” brainwave frequencies toward calmness, focus, or sleep.
- These devices are grounded in neuroplasticity principles; AVE primes your brain for learning, emotional regulation, and neural pattern flexibility.
- Though no MS-specific clinical trials exist yet, AVE shows efficacy in stress reduction, better sleep, and enhanced mood in other groups.
Red/NIR Photobiomodulation & Brain Repair
- Red and near-infrared photobiomodulation (tPBM) targets mitochondria to increase ATP (cellular energy), enhance cerebral blood flow, reduce inflammation, and support synaptic growth—all essential for mood and brain repair.
- The therapy has shown significant reductions in depressive symptoms in clinical settings, including eight-week trials for depression and traumatic brain injury.
- Animal models suggest NIR light slows demyelination and may support remyelination, while human studies indicate improved mood, cognition, and sleep—especially valuable for MS patients.
Complementary Therapies & Lifestyle for MS and Depression Treatment
Complementary treatments aren’t just “nice extras” — they’re powerful, science-backed tools that help support mental health, neuroplasticity, and even myelin repair. Here are the most effective strategies:
Physical Activity & Movement
- Any activity works–from walking to Pilates: Even low-intensity exercise improves mood, reduces fatigue and anxiety, and supports myelin regeneration in animal models—plus there’s a human MS trial underway to confirm these benefits.
- Motor learning & targeted training: Exercises like dancing, cycling, or balance work promote remyelination by activating neuronal circuits—boosting cognitive control and emotional resilience.
- Group vs solo sessions: Exercising with others enhances social connection and motivation, giving extra emotional benefit.
Nutrition & Supplements
- Anti-inflammatory diets: Mediterranean, ketogenic, or MIND diets rich in whole foods, healthy fats, and omega-3s may support myelin production and reduce depression risk.
- Targeted nutrients:
- Vitamin D and omega-3 fatty acids show potential for mood enhancement and MS inflammation control.
- High-dose omega-3s (2 g+/day) may effectively reduce depressive symptoms.
Mind–Body Therapies
- Mindfulness & meditation: Techniques like MBSR or MBCT reduce rumination, anxiety, and depressive episodes. These are proven effective in reducing depression severity and improving emotional regulation in MS.
- Yoga: Builds physical strength, balance, and mental calm. Studies have shown improvements in fatigue, mood, and quality of life in patients with MS.
- Relaxation & stress reduction: Practices like progressive muscle relaxation and relaxation-based mindfulness reduce fatigue and depressive symptoms.
Biofeedback & Neuromodulation
- EMG biofeedback: Helps restore muscle control and reduce MS-associated pain or spasticity—indirectly easing stress and depression.
- Pulsed electromagnetic field (PEMF): While older studies were promising, recent results are mixed; more research is needed.
- Cold/cooling therapy: Helps manage heat sensitivity, making activity and exercise more accessible and comfortable.
Environment & Lifestyle Habits
- Nature exposure: Access to green spaces is linked to lower antidepressant use—being outdoors can boost mood and cognitive restoration.
- Sleep & stress management: Regulating your internal clock, limiting heat exposure, and quitting smoking support both MS and mental wellness.
- Social support & psychoeducation: Educational groups and peer- or guided therapies (like DBT) improve coping skills and reduce emotional isolation.
Why Lifestyle Matters for Mood & Myelin
- Activity-dependent myelination: Movement and motor learning trigger oligodendrocyte growth and myelin repair—reinforcing efficient brain circuits and lifting mood.
- Anti‐inflammatory nutrition: Reducing systemic inflammation improves neurotransmission and reduces mood disruption.
- Stress reduction: Mind–body practices buffer cortisol spikes and inflammation, indirectly protecting brain health.
Frequently Asked Questions (FAQ) about MS and Depression
Up to 50% of people with MS experience major depression at least once, far higher than the general population (about 17%).
Depression in MS is a mix of:
- Biological factors: Immune-driven inflammation and brain lesions in mood centers
- Psychological stress: Coping with physical limitations, uncertainty, and loss can trigger depressive symptoms.
- Social challenges: Isolation, stigma, and shared stress uniquely raise depression risk in MS.
Look for persistent sadness, loss of interest, changes in sleep or appetite, fatigue (beyond typical MS fatigue), difficulty concentrating, guilt, or thoughts of death.
Common placements include:
- Fz (theta/beta training)
- Cz (SMR uptraining)
- Left frontal region (e.g., F3/F7 for theta enhancement)
Seek professional help if depressive symptoms last two weeks or more, affect daily life, or include suicidal thoughts. Depression in MS affects treatment adherence and overall well-being.
Conclusion: Moving Forward with Hope in MS and Depression
Living with both multiple sclerosis and depression can feel overwhelming—but this journey is not without effective, life-changing strategies. Here’s what to take away:
Depression in MS Is Real—and Treatable
Depression affects up to half of individuals with MS and is tied to both biological changes and lifestyle stressors. Recognizing it early—and understanding that it’s not “just your MS”—is the first step toward relief.
A Multi-Faceted Treatment Path Works Best
- Evidence supports combining medications, therapy, lifestyle interventions, and neuro-based therapies for optimal results.
- Lifestyle changes such as exercise, mindfulness, diet, and support groups are backed by clinical studies and can significantly reduce depressive symptoms.
Your Brain—and Myelin—Can Heal
Emerging evidence shows these interventions may not just alleviate depression—they can help the brain rebuild. Strategies such as neurofeedback, red/NIR light therapies, and motor learning support neuroplasticity and may promote remyelination, thereby enhancing both mood and cognitive function.
You Are Not Alone
Even if up to 30% of MS patients with depression go untreated, help works. Nearly all proven treatments—whether pharmacologic or non-pharmacologic—outperform doing nothing. With the right tools, it’s possible to improve fatigue, cognition, mood, and even influence the disease course.
Neurofeedback Home-Use Device for MS Depression Management
 Sale!Get it now! 20% OFF With Code: EARLY20
Sale!Get it now! 20% OFF With Code: EARLY20€303.07Original price was: €303.07.€242.46Current price is: €242.46.
References
1. Choobforoushzadeh, A., Neshat-Doost, H. T., Molavi, H., & Abedi, M. R. (2015). Effect of neurofeedback training on depression and fatigue in patients with multiple sclerosis. Applied Psychophysiology and Biofeedback, 40(1), 1–8
2. Voggenberger L, Böck M, Moser D, Lorbeer G, Altmann P, Leutmezer F, Berger T, Seidel S. Bright light therapy as a non-pharmacological treatment option for multiple sclerosis-related fatigue: A randomized sham-controlled trial. Mult Scler J Exp Transl Clin. 2022 Nov 7;8(4)
3. Seidel, S. et al. (2022). Bright light therapy shows hope for MS fatigue in small study. MS UK.
4. 4. Pinter, D., Kober, S. E., Fruhwirth, V., et al. (2021). MRI correlates of cognitive improvement after home-based EEG neurofeedback training in patients with multiple sclerosis: a pilot study. Journal of Neurology, 268, 3808–3816.











Add a Comment