Are you still struggling to breathe long after your COVID-19 infection has ended? You are not alone. The journey to reclaiming your breath and vitality begins with a powerful, proven solution: pulmonary rehab. This comprehensive guide is your roadmap to recovery, detailing essential pulmonary rehab exercises you can master. Discover how to effectively perform pulmonary rehab exercises at home, from foundational breathing exercises for lungs to using a targeted breathing exercise device for lungs. We will show you how to transform your recovery, turning every breathing exercise for lungs into a deliberate step toward healing, strength, and a life unburdened by breathlessness.
Table of Contents
Toggle- Understanding Lung Damage and the Path to Recovery
- Your Blueprint for Healing: Pulmonary Rehabilitation Programs Explained
- Master Your Breath: Essential Techniques for Lung Recovery
- Train Your Lungs to Win: Introducing “The Breather” Device
- Beyond the Lungs
- The Tech-Enabled Recovery
- Your At-Home Biofeedback Toolkit
- Breathing Exercise Device for the Lungs
- FAQ: Pulmonary Rehab After COVID-19
Understanding Lung Damage and the Path to Recovery
The battle against COVID-19 doesn’t always end when the fever breaks. For many, the virus leaves a challenging legacy in its most vital organ: the lungs. Understanding this impact is the first step toward reclaiming your breath and your life.
SARS-CoV-2, the virus behind COVID-19, primarily attacks the respiratory system. Imagine your lungs as an upside-down tree. The trunk is your windpipe, branching out into smaller airways. At the very end are tiny, delicate air sacs called alveoli. This is where the vital magic happens—oxygen enters your blood, and carbon dioxide is removed.
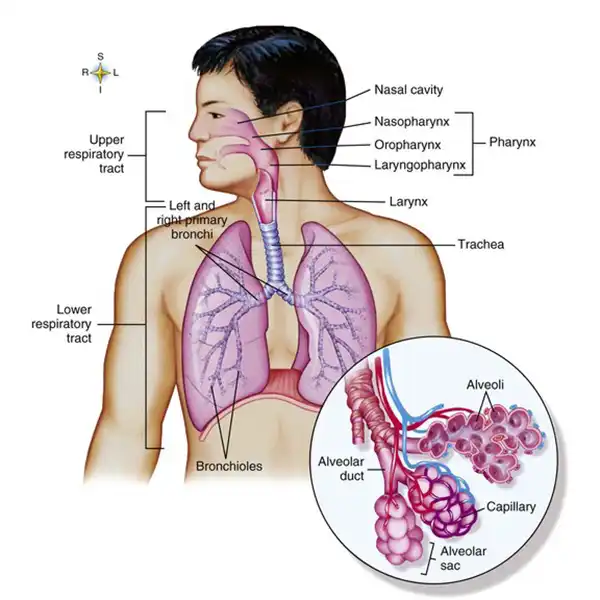
During a COVID-19 infection, the virus invades these sacs. Your immune system fights back, causing inflammation and swelling. In severe cases, the alveoli fill with fluid, leading to COVID-19-associated pneumonia. This condition limits your lungs’ ability to absorb oxygen, causing shortness of breath, cough, and crushing fatigue that many patients experience.
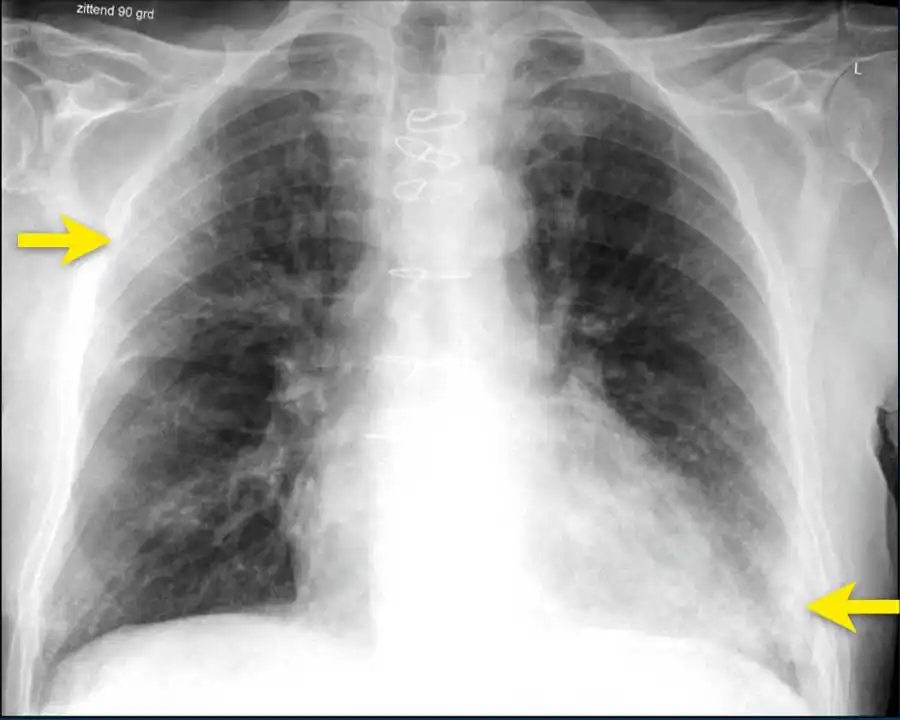
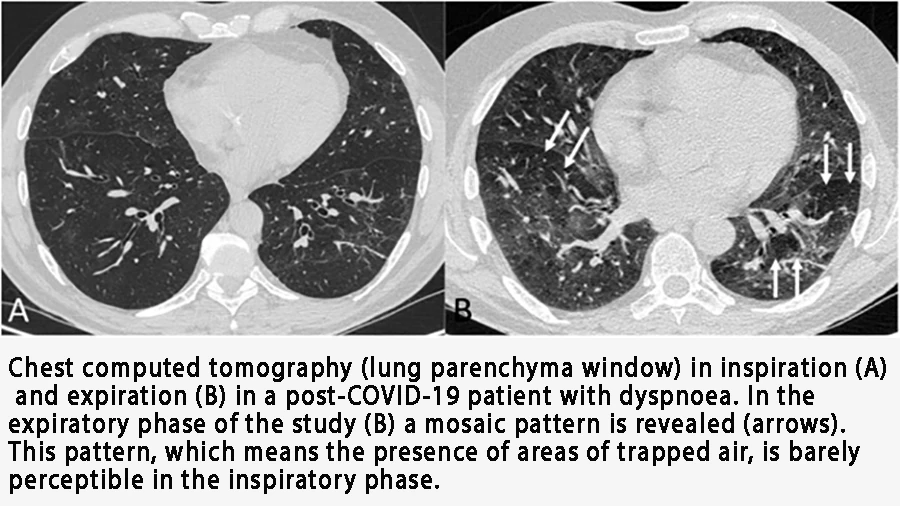
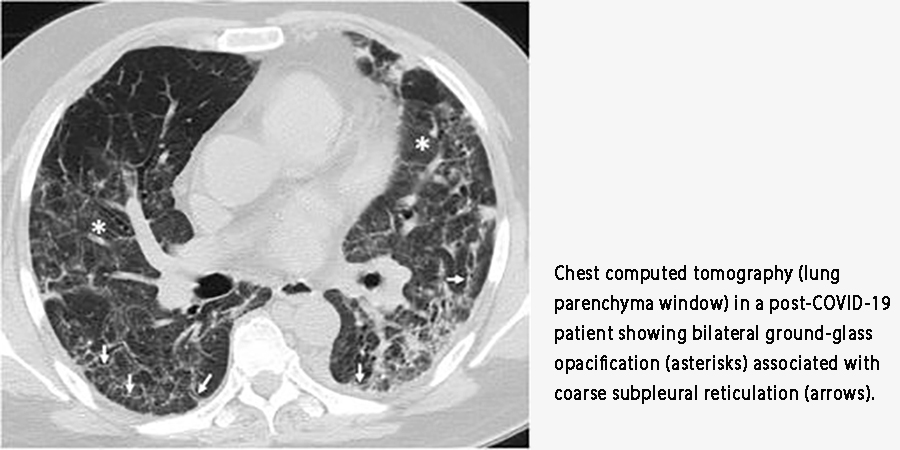
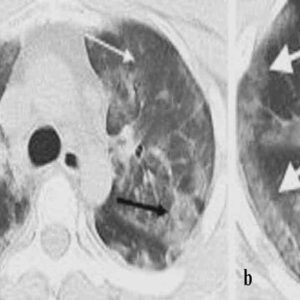
Doctors often see the aftermath on CT scans as “ground-glass opacities”—hazy areas that signal inflammation and damage.
But there is hope. Research shows that with time and targeted effort, your lungs can heal. For instance, studies found that while over half of patients had lung damage 6 weeks after discharge, that number dropped significantly by the 12-week mark. Recovery is a journey, and it starts with a dedicated pulmonary rehab program. This specialized approach is designed to help you rebuild lung function, increase stamina, and reduce breathlessness. Engaging in structured pulmonary rehab exercises is crucial for stimulating healing and guiding your lungs back to health.
Your Blueprint for Healing: Pulmonary Rehabilitation Programs Explained
Feeling short of breath after COVID-19 can be frightening. It creates a cycle of anxiety that makes you avoid activity, which in turn makes your muscles weaker. This is where a structured pulmonary rehab program becomes your essential blueprint for recovery. Think of it as professional training for your lungs and your entire body.
The goal of pulmonary rehabilitation is multi-layered. Firstly, it reverses reversible damage. Secondly, it helps your body adapt to and compensate for any lasting changes. The benefits are profound:
- Boosts Your Metabolism and Mood: It stimulates your body’s systems, increases energy, and improves your mental state.
- Enhances Exercise Tolerance: It systematically helps you build back the strength to perform daily tasks without exhaustion.
- Corrects Breathing Mechanics: It retrains your body to breathe more efficiently, reducing the massive energy cost of labored breathing.
A comprehensive program doesn’t just focus on the lungs. It combines general tonic exercises to improve overall health with special breathing exercises for lungs. These targeted breathing techniques are crucial. They strengthen your respiratory muscles, increase mobility in your chest and diaphragm, and help break the cycle of air hunger. For many, continuing these pulmonary rehab exercises at home is the key to sustaining long-term progress and regaining functional independence.

Master Your Breath: Essential Techniques for Lung Recovery
Knowing how to breathe correctly is the cornerstone of your recovery. After COVID-19, many people develop inefficient breathing patterns that worsen shortness of breath. Retraining your breath is a powerful step toward healing. Here are foundational techniques used in professional pulmonary rehab programs.
Master diaphragmatic breathing.
Often called “belly breathing,” this technique ensures you use your primary breathing muscle—the diaphragm—effectively. To practice, place one hand on your chest and the other on your belly. Breathe in slowly through your nose, feeling your belly push your hand out. Your chest should remain relatively still. Then, exhale slowly through pursed lips, feeling your belly fall. This simple breathing exercise for lungs maximizes oxygen exchange and is the foundation for all advanced techniques.
Unlock the power of resonance frequency breathing.
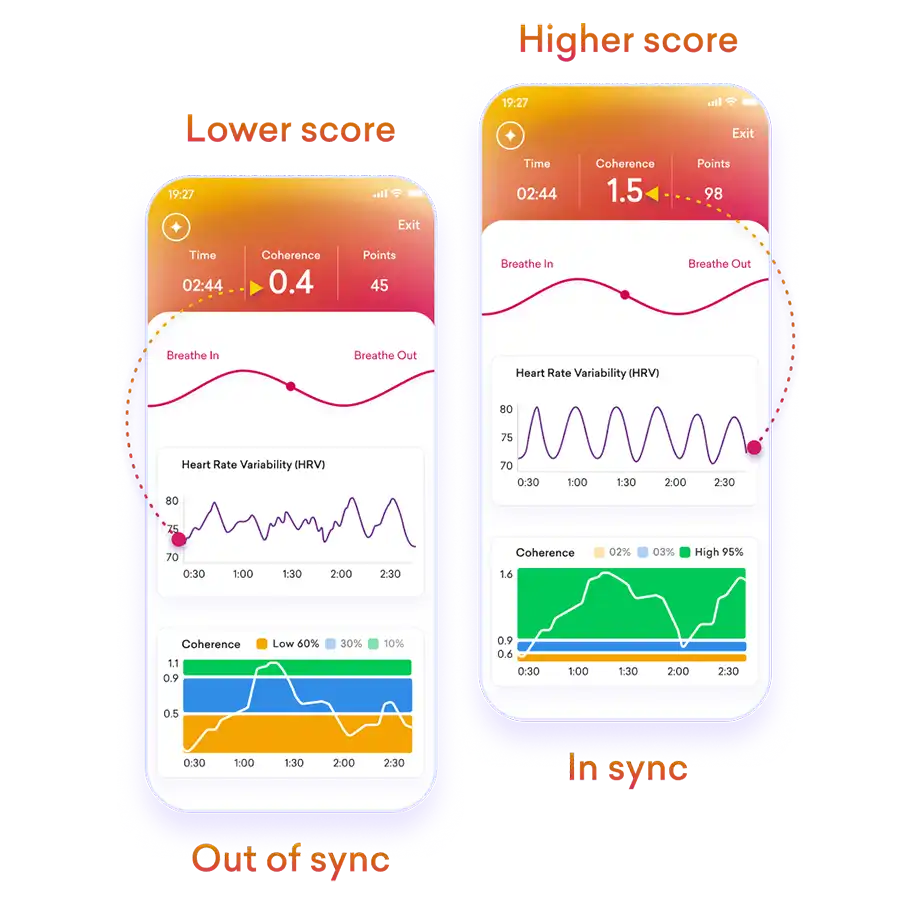
This is a game-changer for the recovery of the cardiovascular and pulmonary systems. Scientific research has identified an optimal breathing rate of approximately 4.5 to 6.5 breaths per minute (around 5.5 seconds inhale, 5.5 seconds exhale). Why is this so effective? This specific pace, combined with diaphragmatic breathing, creates a “resonance” in your cardiovascular system. It synchronizes your heart rate and blood pressure, maximizing Heart Rate Variability (HRV)—a key marker of your body’s resilience and adaptability. This powerful rhythm calms the nervous system, improves gas exchange in the lungs, and is a core component of advanced biofeedback training.
Incorporate breathing control into movement.
Always exhale during the exertion phase. For example, exhale when you stand up, and inhale as you sit back down. This coordinates your effort, making movement feel easier and protecting your airways.
These breathing exercises for your lungs form a powerful toolkit. To begin with, they help relax your airways and strengthen your diaphragm. In addition, they give you more active control over breathlessness. When you practice these techniques consistently as part of your pulmonary rehab exercises at home, you build a strong foundation for recovery.
Train Your Lungs to Win: Introducing “The Breather” Device
What if you could use a simple, handheld device to accelerate your lung recovery? Now you can. While foundational breathing techniques are vital, using a targeted breathing exercise device for lungs can dramatically enhance your results and speed up your healing journey. Enter The Breather, a revolutionary tool designed specifically for respiratory muscle training.
The Breather is not just another gadget; it’s a comprehensive drug-free respiratory therapy system. It functions as both an inspiratory (inhale) and expiratory (exhale) muscle trainer. This dual action is critical because COVID-19 weakens all the muscles involved in breathing.

Here’s why it’s a must-have for your pulmonary rehab exercises at home:
- Targeted Strength Training: Think of it as weightlifting for your respiratory muscles. With independent dials for inhalation and exhalation resistance, you can gradually strengthen your diaphragm and intercostal muscles. Stronger muscles mean breathing requires less effort, directly combating breathlessness.
- Improved Oxygen Flow: By training your muscles to work more efficiently, The Breather helps increase oxygen uptake. This delivers more vital oxygen to your body’s organs and working muscles, boosting your energy and exercise capacity.
- Proven Clinical Benefits: This device is clinically shown to help individuals with respiratory challenges. Regular use can lead to reduced breathlessness, improved peak cough flow, and better oxygen saturation—all crucial goals for post-COVID pulmonary rehab.
Make The Breather the centerpiece of your daily routine. To begin with, it acts as an effective breathing exercise device for your lungs. As a result, it transforms your pulmonary rehab exercises into powerful, measurable, and highly effective training sessions. Furthermore, you can pair it with the diaphragmatic and resonance-frequency breathing techniques from the previous chapter. Together, these methods create a truly transformative recovery experience.
Beyond the Lungs
The Critical Role of Muscle Relaxation and Neuromuscular Training
Recovery from COVID-19 goes far beyond your lungs. The virus often causes significant muscle wasting throughout the body, including in the core and limbs. This weakness contributes to ongoing fatigue, poor balance, and that persistent feeling of breathlessness. Why? Because your body has to work much harder to perform any movement, placing extra strain on your already compromised respiratory system.
This is where targeted muscle relaxation and retraining become non-negotiable. You must break the cycle of tension and weakness. While techniques like guided meditation are helpful, technology now offers a more precise and powerful solution: the NeuroTrac EMG Biofeedback Equipment.
Imagine having a personal coach that gives you a real-time window into your muscle tension. The NeuroTrac Simplex device does precisely that. It uses sensors to detect the electrical activity produced by your muscles (EMG) and displays it back to you as easy-to-understand visual or audio signals. This biofeedback is revolutionary for your pulmonary rehab because it allows you to:
- See Your Tension: Objectively identify which muscles are chronically tight—like your neck, shoulders, and chest—and contributing to inefficient breathing patterns.
- Master Relaxation On-Demand: Learn to release tension in those overworked muscles consciously. By watching the feedback, you can discover what true relaxation feels like and how to achieve it at will.
- Retrain Your Neuromuscular System: Re-establish the brain-body connection for proper muscle function, reducing the extra energy cost of movement and breathing.
Integrating the NeuroTrac Simplex into your routine helps your entire body work in harmony. By consistently using the device, you relax tense muscles and improve neuromuscular control. As a result, you directly reduce the workload on your respiratory system. This means every breathing exercise for your lungs becomes more effective. Ultimately, the device becomes a vital component of a strong and comprehensive recovery plan.
The Tech-Enabled Recovery
How Biofeedback Supercharges Your Pulmonary Rehab
You’ve learned the techniques and the tools. Now, let’s talk about the technology that ties it all together to create a truly optimized recovery plan. Biofeedback is the missing link that transforms guesswork into measurable progress. For post-COVID pulmonary rehab, breathing and Heart Rate Variability (HRV) biofeedback are revolutionary.
So, what is it? Biofeedback is a training technique that uses electronic sensors to give you real-time information about your body’s functions. Essentially, it “feeds back” data you’re normally unaware of, allowing you to gain conscious control. In the context of your recovery, it directly targets the two most critical systems: your breathing and your autonomic nervous system.
The mechanism is powerful. HRV biofeedback involves training yourself to breathe at your body’s “resonant frequency”—typically around 4.5 to 6 breaths per minute. When you breathe at this precise rhythm, a remarkable thing happens: your heart rate, blood pressure, and respiratory cycle synchronize. This synchronization:
- Maximizes Gas Exchange: It creates the ideal conditions for your lungs to absorb oxygen and release carbon dioxide.
- Calms the Nervous System: It powerfully stimulates the vagus nerve, shifting your body out of a stressed “fight-or-flight” state and into a restorative “rest-and-digest” state.
- Increases Autonomic Flexibility: High HRV indicates a healthy, resilient system that can adapt smoothly to physical and emotional challenges.
This scientific approach represents a giant leap beyond traditional methods. It gives you clear, objective data and guided practice at every step. As a result, you can master your resonance-frequency breathing and diaphragmatic breathing with confidence. When you integrate biofeedback into your routine, your pulmonary rehab exercises become precise and personalized. Ultimately, this makes your training far more effective and accelerates your journey back to full health.
Your At-Home Biofeedback Toolkit
HeartMath and BioSignals Devices
The science is clear: biofeedback works. But how can you access this powerful technology? Fortunately, you no longer need a clinical setting. Instead, you can use professional-grade, user-friendly devices at home. These tools help you take charge of your recovery with confidence.
However, you must choose the right device for your specific needs. For your pulmonary rehab exercises at home, we recommend two standout solutions. Each one supports a different stage of recovery and focuses on a specific goal.
HeartMath Inner Balance
For targeted breathing and nervous system regulation, the HeartMath Inner Balance for Focus & Calm is the ideal choice. This sleek, user-friendly device clips to your earlobe and pairs with a simple mobile app. It is perfect if your primary goals are to practice resonant frequency breathing (about six breaths per minute) and to increase Heart Rate Variability (HRV). The app provides real-time visual guides, making it easy to achieve a coherent state that calms your nervous system and optimizes lung function. It’s the ultimate tool for mastering a foundational breathing exercise for lungs and is especially beneficial for those dealing with anxiety and stress post-COVID.
BioSignals 5 Biofeedback Sensors Device
For a comprehensive recovery addressing both physical and emotional symptoms, the BioSignals 5 Biofeedback Sensors Device offers unparalleled depth. This advanced system is for you if you need more than just breathing pacing. It combines an HRV monitor with abdominal and chest breathing belts to provide precise feedback for developing diaphragmatic breathing. It provides a breathing exercise device for lungs.
Furthermore, it includes Galvanic Skin Response (GSR) and temperature sensors. These tools are crucial for managing the stress, anxiety, and emotional turbulence that often hinder physical recovery. If you find that your breathing difficulties are tightly linked to your emotional state, the BioSignals 5 gives you the complete toolkit to address both simultaneously.
Choosing between them depends on your personal recovery journey. If your focus is squarely on mastering your breath and heart rhythm, HeartMath provides a streamlined path. Suppose you require a holistic approach that integrates a breathing exercise device for lungs, HRV training with deep stress and emotion management. In that case, the BioSignals 5 system is the most powerful way to personalize and optimize your entire pulmonary rehab strategy.
Breathing Exercise Device for the Lungs
FAQ: Pulmonary Rehab After COVID-19
Pulmonary rehab is a supervised program designed to help people with chronic breathing problems. After COVID-19, it’s crucial because it directly addresses lung damage, muscle weakness, and debilitating shortness of breath. It uses pulmonary rehab exercises, education, and support to help you regain function and improve your quality of life.
Many effective pulmonary rehab exercises at home can significantly aid your recovery. Techniques like diaphragmatic breathing can be practiced anywhere. Furthermore, devices like The Breather provide structured resistance training, while biofeedback tools like the HeartMath Inner Balance offer real-time coaching to ensure you’re performing exercises correctly for maximum benefit.
The most foundational and effective breathing exercise for lungs is diaphragmatic (belly) breathing, as it retrains your primary respiratory muscle. Building on that, resonance frequency breathing (at about 4.5-6 breaths per minute) is highly powerful for calming the nervous system and improving gas exchange in the lungs.
This is where broader biofeedback tools like the BioSignals 5 device excel. By using its GSR and temperature sensors, you can get direct feedback on your stress levels. This allows you to learn, in real-time, how to consciously calm your body, which directly helps to ease your breathing and break the anxiety-breathlessness loop.
The Breather provides adjustable resistance to both your inhalation and exhalation. This strengthens your diaphragm and intercostal muscles, making every breath require less effort, reducing breathlessness, and improving overall lung capacity.












Add a Comment