In the realm of mental health care, Post-Traumatic Stress Disorder (PTSD) stands as a formidable challenge, affecting millions worldwide with its enduring symptoms and complex neurobiological underpinnings. In recent years, a promising avenue for addressing this condition has emerged in the form of Neurofeedback for PTSD treatment. By harnessing the brain’s electrical activity, EEG Biofeedback offers a novel and non-invasive approach to navigating trauma care.
This article explores the intersection of neuroscience and therapy. It explains EEG Biofeedback’s principles, protocols, and potential for PTSD management. By examining neurobiology, clinical applications, and future directions, we aim to illuminate the role of Neurofeedback therapy for PTSD as a beacon of hope in the journey toward PTSD recovery.
Table of Contents
Toggle- Defining PTSD and its Impact
- Overview of EEG Biofeedback as a Treatment Approach
- Explanation of EEG and Brainwave Patterns
- Principles of Neurofeedback Therapy
- Brain Mechanisms Involved in PTSD
- How Neurofeedback Therapy for PTSD Targets Neural Dysregulation
- Neurofeedback Therapy for Complex PTSD: Protocols
- Assessment and Diagnosis
- Clinical Applications of Neurofeedback for PTSD
- Clinical Outcomes and Benefits of Neurofeedback for PTSD Treatment
- Integration of Neurofeedback for PTSD with Traditional Therapies
- FAQ – Neurofeedback for PTSD Treatment
- Home-Use Devices for Neurofeedback for PTSD
Post-Traumatic Stress Disorder (PTSD) is a debilitating mental health condition. It can profoundly affect individuals who have experienced or witnessed traumatic events. Characterized by symptoms such as intrusive memories, hypervigilance, and emotional numbness, PTSD can significantly impair daily functioning and quality of life. The frequency of PTSD underscores the urgent need for effective interventions to alleviate its burdens. In recent years, Neurofeedback therapy for PTSD has emerged as a promising therapeutic approach.
Defining PTSD and its Impact
Post-traumatic stress disorder (PTSD) is a neuropsychiatric disorder that may develop following exposure to a traumatic event or series of events. Such events can include, but are not limited to, combat experiences, natural disasters, physical or sexual assault, or serious accidents. Individuals with PTSD often re-experience the traumatic event through distressing memories, nightmares, or flashbacks. They may also exhibit avoidance behaviors, distancing themselves from reminders of the trauma, and experience negative changes in mood and cognition.
Furthermore, hyperarousal symptoms, such as exaggerated startle responses and difficulty concentrating, can impair functioning in various domains of life. The impact of PTSD extends beyond the individual, affecting families, communities, and societies at large, underscoring the importance of effective interventions to address its consequences.
Exposure-based therapy is currently one of the most effective treatments for PTSD. However, exposure to traumatic stimuli is so aversive that a significant number of patients drop out of therapy during treatment. Among various attempts to develop novel therapies that bypass such aversiveness, neurofeedback for PTSD treatment appears promising. With neurofeedback, patients can unconsciously self-regulate their brain activity through real-time monitoring and feedback of their EEG.
Overview of EEG Biofeedback as a Treatment Approach
EEG Biofeedback, also known as neurofeedback or neurotherapy. It aims to regulate brain activity through real-time electroencephalography (EEG) signal monitoring. By providing individuals with feedback about their brainwave patterns, EEG Biofeedback enables them to learn self-regulation techniques. Neurofeedback regulates neural activity associated with specific symptoms or conditions.
In the context of PTSD, EEG Biofeedback for PTSD holds promise as a therapeutic approach. Neurofeedback targets dysregulated brain networks involved in the disorder’s pathophysiology. Individuals can learn to adjust their brain activity through personalized training protocols, potentially reducing symptoms and improving overall well-being.
Explanation of EEG and Brainwave Patterns
Electroencephalography (EEG) is a non-invasive technique used to record electrical activity in the brain by placing electrodes on the scalp. Brainwave patterns, categorized into different frequency bands such as delta, theta, alpha, beta, and gamma, represent this activity. Each frequency band is associated with specific mental states and cognitive processes. For example, delta waves (0.5-4 Hz) are prominent during deep sleep, while beta waves (13-30 Hz) are associated with alertness and active concentration. By analyzing EEG recordings, clinicians and researchers can gain insights into brain function and identify abnormalities or dysregulations in neural activity.
Principles of Neurofeedback Therapy
Neurofeedback therapy operates on the principle of operant conditioning, where individuals learn to modify their brainwave patterns using real-time feedback. During a neurofeedback session, an EEG monitoring system measures brainwave activity. It presents this information to the individual through visual or auditory feedback, such as a video game or sound, reflecting their current brain state. Through repeated exposure to this feedback, individuals learn to self-regulate their brainwave patterns.
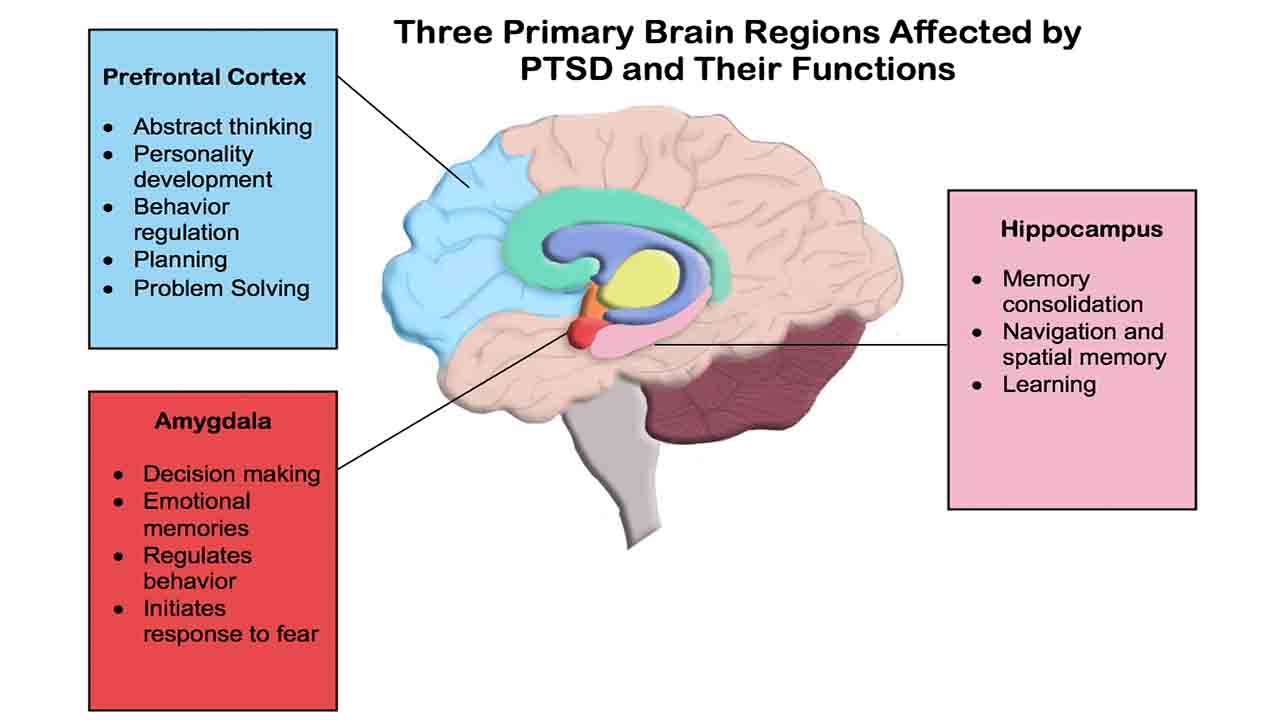
The efficacy of neurofeedback therapy relies on principles of neuroplasticity, the brain’s ability to reorganize and adapt in response to experience. Individuals can repeatedly practice self-regulation techniques to strengthen neural connections associated with desired brain states. This regular practice leads to enduring changes in brain function and behavior. In the context of PTSD, neurofeedback therapy aims to target specific brain regions or networks involved in the disorder’s pathophysiology, such as the amygdala, prefrontal cortex, and hippocampus. By regulating neural activity in these regions, individuals may experience reductions in PTSD symptoms and improvements in overall well-being.
Brain Mechanisms Involved in PTSD
PTSD is associated with alterations in brain structure and function, particularly in regions involved in the processing of fear, stress, and emotional memory. One fundamental structure involved in PTSD is the amygdala, which plays a central role in the encoding and storage of emotional memories. In individuals with PTSD, the amygdala may exhibit heightened activation in response to trauma-related stimuli, leading to exaggerated fear responses and hyperarousal.
Additionally, the prefrontal cortex, responsible for executive functions such as emotion regulation and decision-making, may show reduced activity in PTSD, impairing the individual’s ability to regulate emotional responses and controle fear.
Furthermore, abnormalities in the hippocampus, a brain region involved in memory consolidation and contextual processing, have been observed in individuals with PTSD. Reduced hippocampal volume and impaired functioning may contribute to deficits in memory recall and contextualization of traumatic experiences. Dysregulation of the hypothalamic-pituitary-adrenal (HPA) axis, the body’s stress response system, is also commonly observed in PTSD, leading to alterations in cortisol levels and prolonged activation of stress-related pathways.
How Neurofeedback Therapy for PTSD Targets Neural Dysregulation
EEG Biofeedback for PTSD offers a promising approach to targeting neural dysregulation associated with PTSD by regulating brainwave patterns and promoting self-regulation of neural activity. Through personalized training protocols, individuals can learn to regulate specific brain regions or networks involved in the pathophysiology of PTSD, such as the amygdala, prefrontal cortex, and hippocampus.
For example, neurofeedback protocols may enhance activity in the prefrontal cortex, promoting emotion regulation and cognitive control while reducing hyperactivity in the amygdala, thereby attenuating fear responses and hyperarousal. By providing real-time feedback on brainwave activity, individuals can learn to recognize and control their physiological reactions to trauma-related stimuli, gradually restoring balance to dysregulated neural circuits.
Moreover, EEG Biofeedback for PTSD may facilitate neuroplastic changes in the brain, promoting adaptive rewiring and strengthening of neural connections associated with resilience and coping. By promoting self-regulation of neural activity, EEG Biofeedback for PTSD holds promise as a complementary therapeutic approach for individuals with PTSD, offering the potential for enduring symptom relief and improved quality of life.
Neurofeedback Therapy for Complex PTSD: Protocols
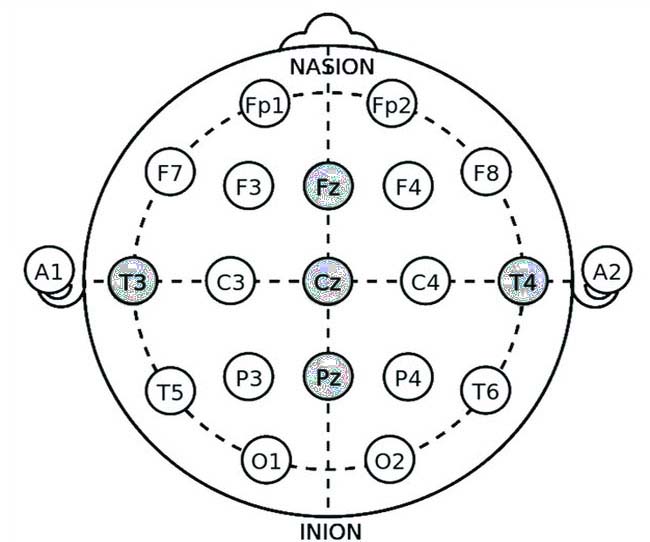
Neurofeedback protocols for PTSD aim to target specific brain regions and networks associated with the disorder. These protocols utilize the International 10-20 system for electrode placement (see video guide for electrode application), ensuring accurate and standardized recording of EEG signals. Below are some commonly used neurofeedback protocols for PTSD, with detailed explanations of electrode application sites and their therapeutic mechanisms.
Alpha-Theta Training Protocol
Electrode Application Sites:
- Fz (Frontal Midline)
- Pz (Parietal Midline)
- Oz (Occipital Midline)
Explanation: Alpha-theta training aims to increase the amplitude of theta waves (4-8 Hz) while decreasing the amplitude of alpha waves (8-12 Hz). This protocol often facilitates deep relaxation, emotional processing, and trauma resolution. During sessions, individuals enter a hypnagogic state, a transitional phase between wakefulness and sleep that features increased theta activity. This state allows for the integration of traumatic memories and emotional healing.
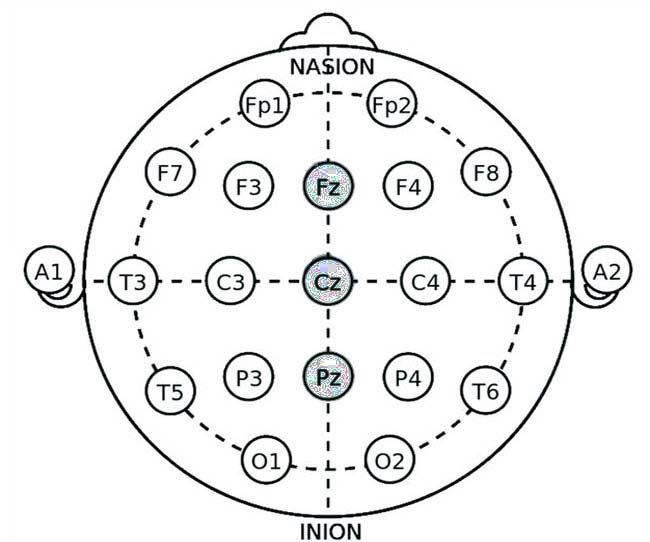
- Fz: Placing an electrode at Fz targets the prefrontal cortex, which is involved in emotion regulation and cognitive control. Enhancing theta activity in this region can promote relaxation and reduce hypervigilance.
- Pz and Oz: Electrodes at Pz and Oz help monitor the overall balance of alpha and theta waves, providing comprehensive feedback on brain activity.
Amygdala Down-Training Protocol
Electrode Application Sites:
- T3 (Left Temporal)
- T4 (Right Temporal)
- Fp1 (Left Frontal Pole)
- Fp2 (Right Frontal Pole)
Explanation: The amygdala down-training protocol reduces excessive beta wave activity (13-30 Hz) in the temporal lobes – amygdala anatomical projection. Elevated beta activity in these areas is associated with hyperarousal and heightened fear responses. By down-training beta waves, this protocol aims to decrease amygdala hyperactivity and promote emotional regulation.
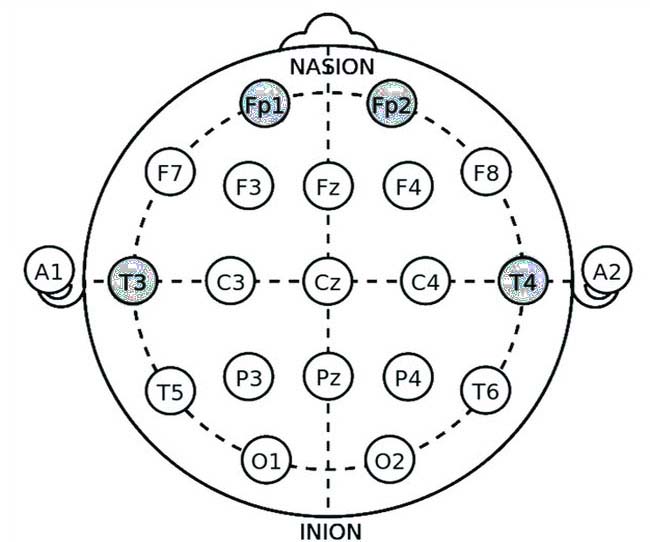
- T3 and T4: Electrodes at T3 and T4 target the temporal lobes, directly influencing the amygdala. Reducing beta activity here can help diminish the exaggerated fear responses characteristic of PTSD.
- Fp1 and Fp2: Electrodes at Fp1 and Fp2 provide additional monitoring of frontal lobe activity, supporting overall emotional regulation and cognitive control.
Prefrontal Cortex Up-Training Protocol
Electrode Application Sites:
- Fp1 (Left Frontal Pole)
- Fp2 (Right Frontal Pole)
- F3 (Left Frontal)
- F4 (Right Frontal)
Explanation: This protocol aims to enhance alpha wave activity (8-12 Hz) in the prefrontal cortex, promoting relaxation, cognitive flexibility, and emotional regulation. Increased alpha activity in the prefrontal cortex can counteract the hypoactivity observed in PTSD, improving the individual’s ability to manage stress and regulate emotions.

- Fp1 and Fp2: Electrodes at Fp1 and Fp2 target the frontal poles, areas involved in executive functions and emotional control.
- F3 and F4: Electrodes at F3 and F4 focus on the dorsolateral prefrontal cortex, enhancing cognitive control and reducing symptoms of anxiety and depression.
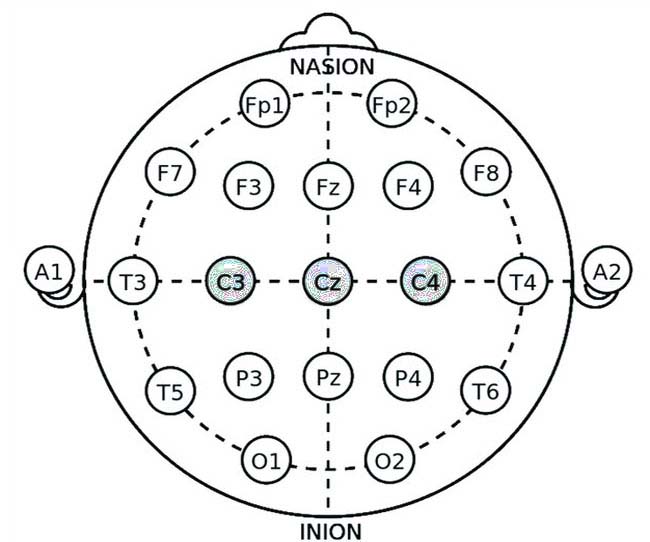
Sensory Motor Rhythm (SMR) Training Protocol
Electrode Application Sites:
- Cz (Central Midline)
- C3 (Left Central)
- C4 (Right Central)
Explanation: The SMR training protocol aims to increase the amplitude of sensory-motor rhythm (12-15 Hz) over the sensorimotor cortex. SMR training is associated with improved relaxation, reduced hyperarousal, and better sleep quality, which are crucial for individuals with PTSD.
• Cz: Placing an electrode at Cz targets the sensorimotor cortex, enhancing SMR activity and promoting relaxation.
• C3 and C4: Electrodes at C3 and C4 provide additional monitoring and training of the sensorimotor areas, supporting overall relaxation and sleep regulation.
Combined Alpha-Theta and Beta Down-Training Protocol
Electrode Application Sites:
- Fz (Frontal Midline)
- Cz (Central Midline)
- Pz (Parietal Midline)
- T3 (Left Temporal)
- T4 (Right Temporal)
Explanation: This combined protocol addresses both the need for deep relaxation and the reduction of hyperarousal by simultaneously training alpha-theta and down-training beta activity. It provides a comprehensive approach to managing PTSD symptoms by promoting relaxation and reducing excessive fear responses.
- Fz and Cz: Electrodes at Fz and Cz help monitor and train frontal and central regions, enhancing relaxation and emotional regulation.
- Pz: The electrode at Pz supports the overall balance of brainwave activity.
- T3 and T4: Electrodes at T3 and T4 target the temporal lobes, reducing hyperarousal and fear responses.
Assessment and Diagnosis
Effective treatment using EEG Biofeedback for PTSD begins with accurate assessment and diagnosis. Here, we will discuss the diagnostic tools and criteria for PTSD and the role of EEG-based assessments in identifying neural dysregulation associated with the disorder.
Screening for PTSD: Diagnostic Tools and Criteria
Diagnostic Criteria:
PTSD is diagnosed based on criteria outlined in the Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition (DSM-5). The criteria include:
- Exposure to Trauma. Direct exposure, witnessing, or learning about a traumatic event experienced by a close associate.
- Intrusive Symptoms. Recurrent, involuntary, and intrusive distressing memories, nightmares, flashbacks, or intense psychological distress upon exposure to cues.
- Avoidance. Persistent avoidance of stimuli associated with the trauma, such as avoiding thoughts, feelings, or external reminders.
- Negative Alterations in Cognitions and Mood: Inability to recall important aspects of the trauma, negative beliefs about oneself or the world, distorted blame, persistent negative emotional states, and diminished interest in activities.
- Hyperarousal and Reactivity. Irritable behavior, hypervigilance, exaggerated startle response, problems with concentration, and sleep disturbances.
- Duration: Symptoms persist for more than one month.
- Functional Significance: Symptoms cause significant distress or impairment in social, occupational, or other important areas of functioning.
Assessment Tools:
- Clinical Interviews: Structured or semi-structured interviews, such as the Clinician-Administered PTSD Scale (CAPS), are used to assess PTSD symptoms and their severity.
- Self-Report Questionnaires: Instruments like the PTSD Checklist for DSM-5 (PCL-5) allow individuals to report their symptoms and their impact on daily life.
- Behavioral Assessments: Observations of behavior and physiological responses to trauma-related stimuli can provide additional insights into the severity of PTSD.
EEG-Based Assessments in PTSD Diagnosis
EEG-based assessments provide a non-invasive way to examine brainwave patterns and identify neural dysregulation associated with PTSD. These assessments can complement traditional diagnostic tools by offering objective data on brain function.
Quantitative EEG (qEEG):
Quantitative EEG (qEEG) involves the statistical analysis of EEG data to identify deviations from normative brainwave patterns. In individuals with PTSD, qEEG may reveal:
- Increased Beta Activity: Excessive beta wave activity, particularly in the temporal lobes, is associated with hyperarousal and heightened anxiety.
- Decreased Alpha Activity: Reduced alpha wave activity in the prefrontal cortex can indicate impaired relaxation and emotion regulation.
- Altered Theta Activity: Abnormal Theta wave patterns may reflect difficulties in processing and integrating traumatic memories.
Event-Related Potentials (ERPs):
Event-related potentials (ERPs) are time-locked brain responses to specific sensory, cognitive, or motor events. ERPs can provide insights into the processing of trauma-related stimuli and cognitive functions affected by PTSD.
Common ERP findings in PTSD include:
- Elevated P3 Amplitude: Increased P3 amplitude in response to trauma-related stimuli indicates heightened attentional processing.
- Reduced N2 Amplitude: Decreased N2 amplitude reflects deficits in cognitive control and emotion regulation.
Clinical Utility of EEG Assessments:
EEG-based assessments can guide the development of personalized neurofeedback protocols by identifying specific areas of neural dysregulation. For example:
- Hyperarousal: Individuals with elevated beta activity may benefit from beta down-training protocols.
- Emotional Dysregulation: Those with reduced alpha activity in the prefrontal cortex may be candidates for alpha up-training protocols.
- Memory Processing: Alpha-theta training can address decreased theta activity to facilitate trauma integration and improve memory processing.
Clinical Applications of Neurofeedback for PTSD
Personalized Treatment Plans: Effective application of Neurofeedback for complex PTSD treatment involves creating customized treatment plans based on individual assessments. This personalized approach targets specific brainwave dysregulations, optimizing the therapeutic benefits.
The process includes:
1. Initial Assessment: Conduction a comprehensive evaluation using diagnostic tools and qEEG assessments to identify specific patterns of neural dysregulation.
2. Protocol Selection: Based on the assessment results, choose appropriate neurofeedback protocols. For instance, individuals with decreased theta activity might undergo alpha-theta training, while those with elevated beta activity may receive beta down-training.
3. Session Structure: Each neurofeedback session lasts 30-60 minutes. During the session, individuals receive real-time feedback on their brainwave activity, allowing them to learn self-regulation techniques.
4. Progress Monitoring: Regular reassessment of brainwave patterns and symptoms ensures the treatment plan remains effective and allows for necessary adjustments.
Case Studies
Case Study 1: Alpha-Theta Training for PTSD
Background: A 35-year-old female veteran presented with severe PTSD symptoms, including frequent flashbacks, hypervigilance, and sleep disturbances. qEEG assessment revealed significantly decreased theta activity.
Protocol: Alpha-theta training aimed to increase theta activity, promoting deep relaxation and trauma integration.
Outcome: Over 20 sessions, the patient reported reduced flashbacks and hypervigilance, improved sleep quality, and an overall sense of calm. Follow-up qEEG showed normalized theta activity, corroborating the symptomatic improvements.
Case Study 2: Beta Down-Training for Hyperarousal
Background: A 28-year-old male who survived a severe car accident experienced heightened anxiety, irritability, and hyperarousal. qEEG assessment indicated elevated beta activity in the temporal lobes.
Protocol: The beta down-training protocol aimed to reduce excessive beta wave activity and alleviate hyperarousal symptoms.
Outcome: After 15 sessions, the patient showed marked reductions in anxiety and irritability. He reported feeling more relaxed and less reactive to stressors. Post-treatment qEEG confirmed reduced beta activity in the targeted areas.
Case Study 3: Prefrontal Cortex Up-Training for Emotional Regulation
Background: A 40-year-old female with a history of childhood trauma struggled with emotional dysregulation and depressive symptoms. qEEG assessment revealed reduced alpha activity in the prefrontal cortex.
Protocol: Prefrontal cortex up-training enhanced alpha activity and improved emotional regulation and cognitive control.
Outcome: Following 25 sessions, the patient improved mood stability and emotional regulation. She also reported increased cognitive clarity and reduced depressive symptoms. qEEG data showed increased alpha activity in the prefrontal cortex.
Clinical Outcomes and Benefits of Neurofeedback for PTSD Treatment
- Symptom Reduction: EEG Biofeedback for PTSD has demonstrated efficacy in reducing core PTSD symptoms such as intrusive thoughts, hypervigilance, and emotional numbness. Neurofeedback helps restore balance and improve overall brain function by targeting specific neural dysregulations.
- Emotional Regulation Improvement.Patients using EEG Biofeedback for PTSD report enhanced emotional regulation. As a result, they can manage stress and trauma-related triggers more effectively. Additionally, improved prefrontal cortex activity helps them gain better control over their emotional responses.
- Enhanced Relaxation and Sleep:Neurofeedback protocols like alpha-theta and SMR training promote deep relaxation and better sleep quality. For example, many individuals experience reduced anxiety and hyperarousal. Consequently, this leads to more restful and restorative sleep.
- Sustained Neuroplastic Changes: The self-regulation techniques learned through EEG Biofeedback for PTSD facilitate lasting neuroplastic changes in the brain. Therefore, patients can experience long-term improvements in their mental health and resilience. As a result, these benefits often continue even after the treatment has ended.
Integration of Neurofeedback for PTSD with Traditional Therapies
While EEG Biofeedback offers a promising standalone treatment for PTSD, its integration with traditional therapies such as Cognitive Behavioral Therapy (CBT), Eye Movement Desensitization and Reprocessing (EMDR), and pharmacotherapy can enhance therapeutic outcomes.
Combining EEG Biofeedback for PTSD with Cognitive Behavioral Therapy (CBT)
Cognitive Behavioral Therapy (CBT) is a widely used therapeutic approach for PTSD, focusing on identifying and modifying negative thought patterns and behaviors. Thus, CBT helps patients develop coping strategies and resilience to manage trauma-related symptoms.
Integration of CBT with EEG Biofeedback for PTSD:
- Enhanced Emotional Regulation: EEG Biofeedback for PTSD improves emotional regulation before or during CBT sessions, making patients more receptive to cognitive restructuring and behavioral interventions.
- Stress Reduction: Neurofeedback can reduce hyperarousal and anxiety, making it easier for patients to engage in CBT techniques and homework assignments.
- Complementary Techniques. EEG Biofeedback for PTSD and CBT application in tandem, with neurofeedback sessions focusing on physiological self-regulation and CBT addressing cognitive and behavioral aspects of PTSD.
Case Example: A patient undergoing CBT for PTSD due to a car accident experienced high levels of anxiety during exposure therapy. Incorporating EEG Biofeedback for PTSD sessions aimed at beta down-training helped reduce his stress, allowing him to engage more fully in exposure exercises and achieve better outcomes.
Integrating EEG Biofeedback for PTSD with Eye Movement Desensitization and Reprocessing (EMDR)
EMDR is a psychotherapy approach that involves processing traumatic memories through guided eye movements or other bilateral stimulation. EMDR aims to reduce the distress associated with traumatic memories and enhance adaptive information processing.
Integration of EMDR with Neurofeedback for complex PTSD:
- Preparation and Stabilization: EEG Biofeedback for PTSD can be used to prepare patients for EMDR by promoting relaxation and stabilization of physiological responses.
- Facilitating Trauma Processing: Neurofeedback can help patients maintain a calm and focused state during EMDR sessions, enhancing their ability to process traumatic memories.
- Post-Processing Support: Following EMDR sessions, EEG Biofeedback for PTSD can support ongoing emotional regulation and reinforce adaptive neural patterns.
Case Example: A patient with childhood trauma found EMDR sessions emotionally overwhelming. By integrating alpha-theta training with her EMDR therapy, she was able to achieve a deeper state of relaxation and process traumatic memories more effectively.
Neurofeedback for PTSD and Pharmacotherapy
Pharmacotherapy for PTSD often involves the use of medications such as selective serotonin reuptake inhibitors (SSRIs), benzodiazepines, and prazosin to manage symptoms like anxiety, depression, and sleep disturbances.
Integration of Pharmacotherapy with EEG Biofeedback:
- Reducing Medication Dependence: EEG Biofeedback can help reduce the need for high doses of medication by addressing both underlying neural dysregulations and improving self-regulation.
- Complementary Effects: Combining pharmacotherapy with EEG Biofeedback can provide a multi-faceted approach to symptom management, addressing both neurochemical and neurophysiological aspects of PTSD.
- Monitoring and Adjustment: EEG assessments can help monitor the effects of medication on brainwave patterns, providing valuable data for optimizing pharmacological treatment plans.
Case Example: A patient taking SSRIs for PTSD experienced persistent hyperarousal and sleep disturbances. Integrating EEG Biofeedback, specifically SMR training, helped improve her sleep quality and reduce hyperarousal, allowing for a gradual reduction in medication dosage.
Benefits of Integrated Treatment Approaches
Holistic Care: Combining EEG Biofeedback with traditional therapies offers a holistic approach to PTSD treatment, addressing cognitive, emotional, and physiological dimensions of the disorder.
Personalized Treatment Plans: Integrated approaches allow for highly customized treatment plans tailored to each patient’s specific needs and preferences, enhancing overall efficacy and satisfaction.
Improved Outcomes: Research indicates that integrated treatment approaches can lead to improved outcomes, with patients experiencing more significant reductions in PTSD symptoms and enhanced overall well-being.
FAQ - Neurofeedback for PTSD Treatment
Neurofeedback works on the principles of operant conditioning and neuroplasticity. During a session, sensors on your scalp measure your brainwave activity. You receive instant feedback through sounds or visual cues on a screen. This process unconsciously teaches your brain to adjust its own activity, strengthening calming neural pathways and reducing those linked to fear and hyperarousal, leading to lasting changes in brain function.
The effectiveness of a protocol depends on the individual’s specific brainwave patterns, but several are commonly used for PTSD:
- Alpha-Theta Training: Promotes deep relaxation and facilitates the processing of traumatic memories.
- Amygdala Down-Training: Reduces beta wave activity to calm an overactive fear response.
- Prefrontal Cortex Up-Training: Increases alpha waves to improve emotional regulation and cognitive control.
- SMR Training: Enhances the sensory-motor rhythm to reduce hyperarousal and improve sleep quality.
Absolutely. Neurofeedback is often integrated with traditional therapies for a more comprehensive approach. It can prepare the brain for treatment by lowering baseline anxiety and hyperarousal, making patients more receptive to the cognitive work of CBT or the memory processing involved in EMDR. This combination can lead to faster and more robust therapeutic outcomes.
Neurofeedback targets explicitly the brain networks disrupted by PTSD. This includes calming the amygdala (the brain’s fear center), strengthening the prefrontal cortex (responsible for emotional regulation and reasoning), and supporting the hippocampus (involved in memory processing). By regulating these areas, neurofeedback helps restore balance to the entire fear-processing system.










Add a Comment