Attention Deficit Hyperactivity Disorder (ADHD) has become one of the most common neurodevelopmental and psychiatric disorders of childhood (3% to 7% of school-age children) that persists into adolescence and adulthood in 40-60% of cases. ADHD treatment’s main strategies are the use of pharmacological therapy, omega-3, multivitamins, and multi-minerals. Neurofeedback for ADHD management is a non-pharmacological intervention based on neuroplasticity characteristics of the brain and utilizes cognitive behavioral therapeutic elements to gain access to and practice brain activity. In fact, several organizations worldwide are investigating claims that neurofeedback therapy for ADHD is as effective as pharmacological therapy, but significantly longer-lasting and free of side effects. This becomes more true if we consider the current friendly use of neurofeedback devices for ADHD management at home, school, university, and workplace.
Table of Contents
Toggle- Understanding ADHD in Children
- ADHD Symptoms in Children and Teenagers
- ADHD Symptoms in Adults
- ADHD SYMPTOM CHECKLISTS
- WHAT PARTS OF THE BRAIN ARE AFFECTED BY ADHD?
- NEUROPATHOPYSIOLOGY OF ADHD
- BRAIN WAVES IN ADHD
- NEUROFEEDBACK FOR ADHD MANAGEMENT
- Neurofeedback as an Alternative to Medications for ADHD
- How Neurofeedback Therapy for ADHD Works and Its Proven Efficacy
- The Role of Home Neurofeedback Devices and Dopamine Reinforcement
- Key Electrode Sites for ADHD Neurofeedback
- Neurofeedback Protocols for ADHD Management
- Effectiveness of Neurofeedback Therapy for ADHD management
- HOME USE DEVICE FOR NEUROFEEDBACK FOR ADHD MANAGEMENT
- ADHD OTHER MANAGEMENT MEANS
- Frequently Asked Questions about Neurofeedback Therapy for ADHD
Understanding ADHD in Children
Attention-deficit hyperactivity disorder (ADHD) is the most commonly diagnosed behavioral disorder in children, but it is also often misunderstood and the subject of controversy. As a result, confusion surrounding the disorder has led to both under- and over-treatment of children. Currently, doctors primarily diagnose ADHD by referring to the criteria outlined in the Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition, Text Revision (DSM-IV, 1994) or the International Statistical Classification of Diseases and Related Health Problems, 10th Revision (ICD-10, World Health Organization, 1992).
ADHD is a childhood-onset disorder characterized by inattention, hyperactivity, and impulsivity. Notably, the impact of ADHD on society is enormous. It imposes significant financial costs, causes stress for families, and leads to adverse academic and vocational outcomes. Moreover, it harms children’s self-esteem. Children with ADHD are easily recognized in clinics, schools, and at home due to their noticeable behaviors.
Challenges and Controversies in ADHD Across the Lifespan
Children with ADHD often struggle with daydreaming and distraction, finding it hard to stay focused for long periods. Additionally, their impulsive actions can result in accidents, difficulties with peers, and classroom disruptions. Hyperactivity, demonstrated through fidgeting and excessive talking, frustrates both teachers and parents. Consequently, schools typically have a low tolerance for such behavior, and parents struggle to manage their children in crowds or enforce reasonable sleep schedules. As these children enter their teenage years, hyperactivity and impulsivity may decrease, but ADHD symptoms persist. Unfortunately, teens with ADHD often experience low self-esteem, strained relationships, and an increased risk of delinquency, smoking, and substance abuse.
The diagnosis of ADHD in adults has generated much debate. Some researchers argue that most cases of ADHD are resolved by adulthood, questioning the validity of adult ADHD diagnoses. However, others believe that diagnosing ADHD in adults is both reliable and valid. Longitudinal studies have shown that as many as two-thirds of children with ADHD continue to have impaired symptoms into adulthood. In adults, restlessness often replaces hyperactivity. Throughout the life cycle, individuals with ADHD frequently experience comorbid conditions such as conduct, depression, bipolar, and anxiety disorders.
ADHD Symptoms in Children and Teenagers
ADHD is divided into three subtypes:
- predominantly inattentive (ADHD-PI or ADHD-I),
- predominantly hyperactive-impulsive (ADHD-PH or ADHD-HI), and
- combined type (ADHD-C).
The symptoms of ADHD in children and teenagers are well-defined, and they’re usually noticeable before the age of 6. They occur in multiple situations, such as at home and school.
Inattentiveness
The main signs of inattentiveness are:
- having a short attention span and being easily distracted
- making careless mistakes – for example, in schoolwork
- appearing forgetful or losing things
- being unable to stick to tasks that are tedious or time-consuming
- appearing to be unable to listen to or carry out instructions
- constantly changing activity or task
- having difficulty organizing tasks.
Hyperactivity and impulsiveness
The main signs of hyperactivity and impulsiveness are:
- being unable to sit still, especially in calm or quiet surroundings
- constantly fidgeting
- being unable to concentrate on tasks
- excessive physical movement
- excessive talking
- being unable to wait their turn
- acting without thinking
- interrupting conversations
- little or no sense of danger
These symptoms can cause significant problems in a child’s life, such as underachievement at school, poor social interaction with other children and adults, and problems with discipline.
Challenges Faced by Children with ADHD
Children with ADHD often face significant challenges in their daily lives. These challenges can include underachievement at school, poor social interactions with peers and adults, and issues with discipline. One common symptom of ADHD, both in children and adults, is the inability to focus for extended periods on tasks. People with ADHD tend to get easily distracted, which makes it difficult for them to maintain focus on an activity, assignment, or chore. However, there is a lesser-known and more controversial symptom called hyperfocus. While other conditions can include hyperfocus as a symptom, here we will focus on how it relates to ADHD.
Understanding Hyperfocus in ADHD
Hyperfocus refers to the intense concentration that some individuals with ADHD experience. ADHD isn’t just a deficit of attention but rather a difficulty in regulating attention on desired tasks. Mundane tasks may feel impossible to focus on, while more engaging activities can be entirely absorbing. For instance, a person with ADHD may struggle with homework or work projects but can spend hours fully engrossed in video games, sports, or reading. During hyperfocus, they become so immersed in what they enjoy that they lose track of time, neglect other responsibilities, and ignore their surroundings. Although this intense concentration sometimes leads to productive work, it can also cause people to have less constructive activities.
Harnessing and Managing Hyperfocus in ADHD
Managing hyperfocus, especially in children, is crucial for their growth and development. It’s important to find interests that steer them away from isolated activities and promote social interaction, such as music or sports. For adults with ADHD, hyperfocus can also be a challenge at work and home. Rather than forbidding certain activities, the key is to harness their focus by making work or school more stimulating. Although difficult for children, this strategy can become advantageous for adults, particularly in the workplace. Finding a job aligned with their interests allows individuals with ADHD to thrive, using hyperfocus to their benefit.
Video – More screen tine leads to ADHD
Correlation Between ADHD and High Levels of Cell Phone Use
The Struggle with Mobile Phone Use in Children with ADHD
As a parent of a child with ADHD, you might notice how intensely your child’s attention can be focused on technology. Games, texting, the internet, and social media often capture their full attention. These aspects of mobile phone use provide a constant flow of feedback and stimulation, keeping the brain’s pleasure centers highly engaged. This makes it especially difficult to pull your child away from their phone. While researchers have not yet proven that excessive phone use increases the risk of ADHD, it’s essential to encourage thoughtful and limited phone use. There is a known correlation between high levels of cell phone use and ADHD, which raises questions about the impact of mobile technology on attention levels in children and teens.
Some studies suggest that children who frequently use their phones for calls and games are at higher risk for developing ADHD symptoms. However, it’s also possible that kids already experiencing ADHD symptoms, like inattention or hyperfocus, are drawn to these activities. For children with ADHD, the combination of hyperfocus and mobile technology can turn into a risky behavioral pattern.
Behavioral and Cognitive Dependence on Mobile Devices
Unlike other children who may lose interest in a smartphone game or app after a short time, kids with ADHD are more likely to become dependent on their devices. This dependency can be both behavioral and cognitive in nature. Behaviorally, kids may get caught in a loop of endlessly checking social media apps or trying to reach the next level in a game. Cognitively, they may become hyper-focused on their phone, constantly thinking about it or experiencing distress when they are unable to access it. This reliance on mobile devices can lead to other mental health issues, including anxiety, depression, sleep disturbances, and low self-esteem.
The cognitive aspect of this dependence may manifest when a child becomes distressed if their phone dies or if they can’t sleep without it nearby. Hyperfocus on technology not only distracts from important tasks but can also interfere with emotional regulation and day-to-day functioning. It’s essential to recognize how deeply these devices can draw a child with ADHD in, making them feel disconnected from their surroundings and responsibilities.
Managing Hyperfocus and Reducing Phone Dependence
While hyperfocus can create challenges, it can also be managed in ways that benefit a child with ADHD. Parents play a critical role in managing the time and content their children spend on phones. By keeping mobile devices out of bedrooms, parents can support healthy sleep habits. Providing alternative activities that are just as stimulating, but non-digital, is key to reducing phone dependency without it feeling like a punishment. Encourage activities that engage your child’s interests outside of screens, such as spending time at the park, visiting a museum, or going swimming.
Helping your child develop interests that foster social interaction, such as sports or music, can effectively reduce their reliance on mobile devices. Neurofeedback therapy for ADHD has also shown great promise in managing ADHD symptoms, improving memory, attention, concentration, and focus. These improvements can ultimately help curb a child’s addiction to phones and computers, offering a healthy, balanced approach to managing both ADHD and screen time.
Related conditions in children and teenagers with ADHD
Although not always the case, some children may also have signs of other problems or conditions alongside ADHD, such as:
- Anxiety disorder – which causes your child to worry and be nervous much of the time; it may also cause physical symptoms, such as a rapid heartbeat, sweating, and dizziness
- Oppositional defiant disorder (ODD) – this is harmful and disruptive behavior, particularly towards authority figures, such as parents and teachers.
- Conduct disorder – this often involves a tendency towards highly antisocial behavior, such as stealing, fighting, vandalism, and harming people or animals.
- Depression
- Sleep problems – finding it difficult to get to sleep at night and having irregular sleeping patterns
- Autistic spectrum disorder (ASD) – this affects social interaction, communication, interests, and behavior.
- Epilepsy – a condition that affects the brain and causes repeated fits or seizures
- Tourette’s syndrome – a condition of the nervous system characterized by a combination of involuntary noises and movements (tics)
- Learning difficulties – such as dyslexia or dyscalculia.
ADHD Symptoms in Adults
In adults, the symptoms of ADHD are more difficult to define. This is mainly due to a lack of research into adults with ADHD.
As ADHD is a developmental disorder, it cannot develop in adults without first appearing during childhood. However, the symptoms of ADHD often persist from childhood into a person’s teenage years and then adulthood.
Any additional problems or conditions experienced by children with ADHD, such as depression or dyslexia, may also continue into adulthood. By the age of 25, an estimated 15% of people diagnosed with ADHD as children still have a full range of symptoms, and 65% still have some symptoms that affect their daily lives. Hyperactivity tends to decrease in adults, while inattentiveness tends to worsen as adult life pressures increase. Adult symptoms of ADHD also tend to be far more subtle than childhood symptoms.
Some specialists have suggested the following as a list of symptoms associated with ADHD in adults:
- Impulsiveness
- Excessive activity or restlessness and edginess
- Carelessness and lack of attention to detail
- Continually starting new tasks before finishing old ones
- Poor organizational skills and problems prioritizing
- Poor time management skills
- Problems focusing on a task
- Poor planning
- Trouble multitasking
- Continually losing or misplacing things
- Forgetfulness
- Difficulty keeping quiet and speaking out of turn
- Blurting out responses and often interrupting others
- Frequent mood swings, irritability, and a quick temper
- Low frustration tolerance
- Trouble coping with stress
- Extreme impatience
- Taking risks in activities, often with little or no regard for personal safety or the safety of others – for example, driving dangerously.
Related conditions in adults with ADHD
Although ADHD doesn’t cause other psychological or developmental problems, as with ADHD in children and teenagers, ADHD in adults can occur alongside several related problems or conditions and make treatment more challenging.
- Mood disorders. Many adults with ADHD also have depression, bipolar disorder, or another mood disorder. While mood problems aren’t necessarily due directly to ADHD, a repeated pattern of failures and frustrations due to ADHD can worsen depression.
- Anxiety disorders. Anxiety disorders occur pretty often in adults with ADHD. Anxiety disorders may cause overwhelming worry, nervousness, and other symptoms. Anxiety is getting worse because of the challenges and setbacks caused by ADHD.
- Learning disabilities. Adults with ADHD may score lower on academic testing than adults of their age, intelligence, and education without ADHD. Learning disabilities can include problems with understanding and communicating.
- Other psychiatric disorders. Adults with ADHD are at increased risk of other psychiatric disorders, such as personality disorders, intermittent explosive disorder, and substance abuse.
– personality disorders – conditions in which an individual differs significantly from the average person in terms of how they think, perceive, feel, or relate to others
– bipolar disorder – a condition affecting your mood, which can swing from one extreme to another
– obsessive-compulsive disorder (OCD) – a condition that causes obsessive thoughts and compulsive behavior.
The behavioral problems associated with ADHD can also cause problems such as difficulties with relationships and social interaction.
Genetic Factors in ADHD Development
The exact cause of ADHD remains unclear, though researchers believe a combination of factors may contribute to it. One key area of focus involves genetics, particularly a gene linked to dopamine production. Dopamine is a chemical that helps the brain regulate consistent attention. Researchers suspect that ADHD may be connected to this gene, as dopamine plays a crucial role in attention control. ADHD often runs in families, and in many cases, the genes inherited from parents are considered a significant factor in developing the condition. Studies have shown that parents and siblings of a child with ADHD are more likely to have the condition as well. However, the inheritance of ADHD is complex and does not appear to be caused by a single genetic issue.
Additional Contributing Factors to ADHD
While genetics play a significant role, other factors may also contribute to the development of ADHD. Some researchers suggest that brain injuries or infections may be potential contributors. Additionally, exposure to certain conditions before birth, such as a lack of oxygen or exposure to substances like alcohol or nicotine, could increase the risk of ADHD. Premature birth is another factor linked to the condition. Moreover, difficult experiences during early childhood may influence the likelihood of developing ADHD. These factors, in combination with genetics, create a multifaceted picture of what may lead to ADHD.
ADHD SYMPTOM CHECKLISTS
Does My Child Have Attention Deficit Hyperactivity Disorder (ADHD or ADD)?
Only a mental health professional can tell for sure whether symptoms of distractibility, impulsivity, and hyperactivity are severe enough to suggest a positive ADHD diagnosis. The ADHD Checklist for Boys and Girls tests may provide behavioral clues and suggestions about next steps. This questionnaire is designed to determine whether your child demonstrates symptoms similar to those of attention-deficit/hyperactivity disorder (ADHD). Download and print out the NICHQ Vanderbilt Assessment Scale. If you answer yes to a significant number of these questions, consult a licensed mental health practitioner. An accurate diagnosis can only be made through clinical evaluation.
Scoring Instructions for the NICHQ Vanderbilt Assessment Scales
These scales should NOT be used alone to make any diagnosis. You must consider information from multiple sources. Scores of 2 or 3 on a single Symptom question often reflect frequently occurring behaviors. Scores of 4 or 5 on Performance questions reflect problems in performance.
The initial assessment scales, for parents and teachers, have two components: symptom assessment and impairment in performance. On both the parent and teacher initial scales, the symptom assessment screens for symptoms that meet the criteria for both inattentive (items 1–9) and hyperactive-impulsive (items 10–18) ADHD.
To meet DSM-IV criteria for the diagnosis, one must have at least six positive responses to either the inattentive nine or hyperactive nine core symptoms or both. A positive response is a 2 or 3 (often, very often) (you could draw a line straight down the page and count the positive answers in each subsegment). There is a place to record the number of positives in each subsegment and a place for a total score for the first 18 symptoms (add them up).
Screening for Comorbidities and Performance Impairment
The initial scales also have symptom screens for three other comorbidities: oppositional-defiant, conduct, and anxiety/ depression. These are screened by the number of positive responses in each of the segments separated by the “squares.” The specific item sets and number of positives required for each co-morbid symptom screen set are detailed in the PDF file.
The second section of the scale includes a set of performance measures, scored 1 to 5, with scores of 4 and 5 indicating a problem.
To meet the criteria for ADHD, there must be at least one item of the Performance set in which the child scores a 4 or 5; i.e., there must be impairment, not just symptoms, to meet diagnostic criteria. The sheet has a place to record the number of positives (4s, 5s) and an Average Performance Score—add them up and divide by the number of Performance criteria answered.
Adult ADHD Self-Report Scale (ASRS) Symptom Checklist
Many adults have been living with Adult Attention-Deficit/Hyperactivity Disorder (Adult ADHD) and don’t recognize it. Why? Because its symptoms are often mistaken for a stressful life. If you’ve felt this type of frustration most of your life, you may have Adult ADHD.
The following 6-question Adult Self-Report Scale-Version 1.1 (ASRS-V1.1) Screener questionnaire can be used as a starting point to help you recognize the signs/symptoms of Adult ADHD, but is not meant to replace consultation with a trained healthcare professional. An accurate diagnosis can only be made through a clinical evaluation. Regardless of the questionnaire results, if you have concerns about the diagnosis and treatment of Adult ADHD, please discuss your concerns with your physician.
The Adult Self-Report Scale Symptom Checklist is intended for people 18 or older. Download below.
WHAT PARTS OF THE BRAIN ARE AFFECTED BY ADHD?
In children with ADHD, several brain regions and structures (pre-frontal cortex, striatum, basal ganglia, and cerebellum) tend to be smaller by roughly 5%.
ADHD brains have low levels of a neurotransmitter called norepinephrine, which is linked arm-in-arm with dopamine. The ADHD brain has impaired neurotransmitter activity in four functional regions.
1. Frontal Cortex
This region controls high-level functions:
- Attention
- Executive Function
- Organization
This region orchestrates our high-level functioning: maintaining attention, organization, and executive function. A dopamine deficiency within this brain region might cause inattention, problems with organization, and impaired executive functioning.
2. Limbic System
This region is located deeper in the brain and regulates emotions and attention. A dopamine deficiency in this region might result in restlessness, inattention, or emotional volatility.
3. Basal Ganglia
These neural circuits regulate communication within the brain. Information from all brain regions enters the basal ganglia and is relayed to the correct sites in the brain. A dopamine deficiency in the basal ganglia can cause inter-brain communication and information to “short-circuit,” resulting in inattention or impulsivity.
4. Reticular Activating System
This is the major relay system among the many pathways that enter and leave the brain. A dopamine deficiency here can cause inattention, impulsivity, or hyperactivity.
These four regions interact, so a deficiency in one area may cause a problem in one or more of the others. ADHD results from problems in one or more of these regions.
NEUROPATHOPYSIOLOGY OF ADHD
The Role of Dopamine in Brain Function
The human brain contains millions of neurons that secrete dopamine. These cells are distributed across different regions, each responsible for various functions. These include movement, cognitive functions, memory, and essential management skills like decision-making and planning, which enable attention and learning. Dopamine is also released when we experience pleasure or success as part of the brain’s positive feedback regulation system. This system allows us to strengthen desired behaviors and progress toward our goals. It operates through neural pathways that generate feelings of pleasure, motivation, and concentration. Dopamine secretion increases when we feel motivated or interested in completing a task. This, in turn, boosts motivation, attention, and the sensation of success.
ADHD and Brain Dysfunction
ADHD is linked to multiple neurophysiological deficits. Recent theories combine clinical symptoms and neuropsychological challenges within the framework of specific brain dysfunctions. Cognitive deficits in ADHD may arise from dysfunctions in the frontostriatal or mesocortical brain networks, both of which involve the dopaminergic system. Additionally, difficulties with reward processing are likely connected to problems in the mesolimbic dopaminergic system (Sagvolden et al., 2005; Sonuga-Barke, 2005).
Research suggests that these deficits can be present even in the resting brain. A more fundamental neuronal network approach points to Default Mode-Network (DMN) activity as a significant issue. DMN activity, typically prominent during rest, may interfere with the brain’s task-related networks, leading to challenges in state regulation and periodic attention lapses (Sonuga-Barke and Castellanos, 2007; Castellanos and Proal, 2012). This interference explains why neurofeedback is particularly effective in managing ADHD, offering long-lasting results.
Pharmacological and Non-Pharmacological ADHD Treatments
Pharmacological treatments, especially stimulants like methylphenidate and amphetamine sulfate and non-stimulants like Atomoxetine, have proven to be highly effective in alleviating ADHD symptoms (Banaschewski et al., 2006; King et al., 2006). These medications work by increasing norepinephrine levels in the brain. Stimulants achieve this by promoting norepinephrine synthesis, while non-stimulants slow the breakdown of norepinephrine. Once the brain’s norepinephrine levels are balanced, the individual’s hyperactivity, inattentiveness, and impulsivity diminish.
However, these effects only last as long as the medication is active. The problem with stimulant drugs like Adderall and Ritalin is the potential for addiction, as individuals need more of the drug to continue feeling in control and focused. Researchers have questioned the long-term effectiveness of these medications (Molina et al., 2009; van de Loo-Neus et al., 2011). Side effects, non-responsiveness, and social stigma have increased interest in non-pharmacological treatments (Sonuga-Barke et al., 2013; Daley et al., 2014).
BRAIN WAVES IN ADHD
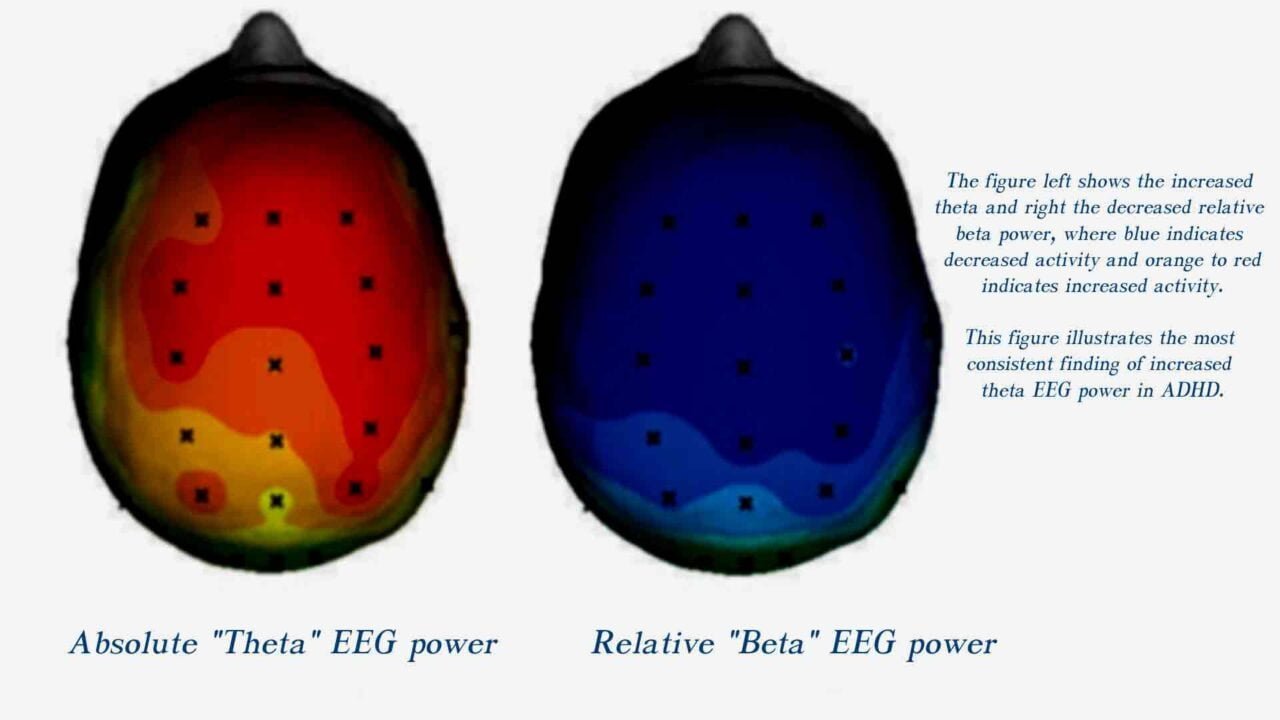
ADHD has been associated with specific clinical behavioral symptoms for many years. Recently, interest has been focused on ADHD to determine whether specific abnormal EEG patterns correlate with clinical manifestations of ADHD.
Multiple studies have determined that children with ADHD have more significant theta activity compared to gender and age-matched controls. Other studies showed increased delta activity coupled with decreased alpha and beta activities.
Additionally, abnormalities in the theta/beta ratio are one of the most significant measures of EEG alterations in ADHD.
Some researchers describe significantly increased theta/low beta and theta/alpha ratios in patients with ADHD.
Brain scans show that ADHD brains produce more low-frequency delta or theta brain waves than do neurotypical brains and often show a shortage of high-frequency beta brain waves linked to focus and impulse control.
NEUROFEEDBACK FOR ADHD MANAGEMENT
Neurofeedback as an Alternative to Medications for ADHD
EEG Biofeedback, also known as Neurofeedback (NFB), is a non-pharmacological intervention for ADHD management that incorporates cognitive behavioral therapy elements to train and regulate brain activity. Many organizations worldwide are exploring the claims that neurofeedback therapy for ADHD can be as effective as pharmaceutical treatments in helping children with ADHD. For example, a course of neurofeedback sessions may have the same effect as regularly taking psychostimulant medications like Ritalin. However, unlike medication, neurofeedback therapy for ADHD often eliminates the need for ongoing treatment after the course completion, reducing reliance on drugs altogether.
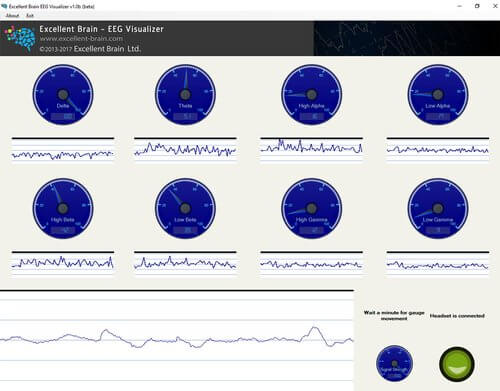
The brain’s functioning and a person’s behavior are interconnected. Changes in behavior can alter the brain and vice versa. Neurofeedback therapy for ADHD focuses on changing behavior by training the brain in a positive, natural manner. The primary goal is to increase the brain’s capacity for beta waves while reducing the occurrence of delta and theta waves, thereby improving attention and focus.
How Neurofeedback Therapy for ADHD Works and Its Proven Efficacy
Recent clinical trials have produced intriguing findings, showing that ADHD brains exhibit distinct EEG patterns. The results also confirm the effectiveness of neurofeedback protocols focusing on theta suppression/beta enhancement, as well as theta suppression/alpha enhancement, in reducing ADHD symptoms.
Theta/beta training aims to reduce theta band activity (4–8 Hz) and increase beta band activity (13–20 Hz) in the electroencephalogram (EEG). This corresponds to an alert, focused, yet relaxed state, addressing the cortical arousal aspects of ADHD. The alpha enhancement protocol, in particular, is more effective in reducing omission errors, enhancing attention, and improving cognitive performance in individuals with ADHD.
The Role of Home Neurofeedback Devices and Dopamine Reinforcement
Neurofeedback training allows individuals to self-regulate their brainwave frequency. Numerous home-use neurofeedback headset devices are now available, enabling users to practice brain training from the comfort of their own homes. These devices measure brain frequencies in real-time while the user plays a video game that responds to their brainwaves. The trainee can score points in the game only when their brainwave frequency aligns with the desired state for attention or relaxation.
When the trainee reaches the correct brainwave frequency, they experience success, activating the brain’s reinforcement system and naturally increasing dopamine secretion. This dopamine release enhances attention and motivates the trainee to maintain the correct brainwave state. Over time, the brain learns to remember how to reach the desired frequency, enabling the individual to support improved focus and behavior in daily life, even without the use of the neurofeedback device. This process leads to long-lasting reductions in ADHD symptoms, making neurofeedback a powerful tool for ADHD management.
Key Electrode Sites for ADHD Neurofeedback
1. Fz (Frontal Midline):
- Location: Frontal lobe, on the midline, 20% of the distance from the nasion (bridge of the nose).
- Relevance: Associated with attention, impulse control, and executive function. Targeting Fz can help improve these areas.
2. Cz (Central Midline):
- Location: The scalp vertex, halfway between the nasion and inion and equally spaced between the left and right preauricular points (just above the ears).
- Relevance: Central region involved in motor control and general arousal regulation. Often used as a reference site.
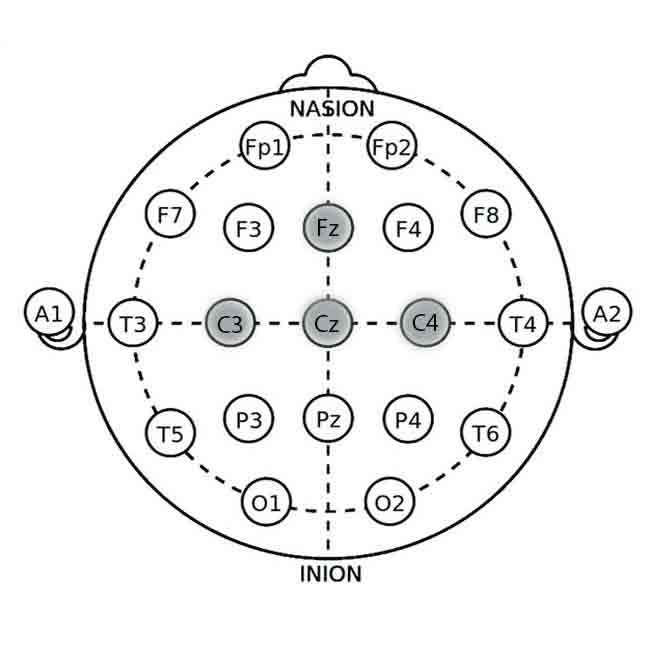
3. C3 (Left Sensorimotor Cortex):
- Location: Left hemisphere, 20% of the distance from the midline along the central line.
- Relevance: Involved in motor control and coordination, relevant for reducing hyperactivity.
4. C4 (Right Sensorimotor Cortex):
- Location: Right hemisphere, analogous to C3 on the right side.
- Relevance: Also involved in motor control, balancing neural activity related to motor functions.
Neurofeedback Protocols for ADHD Management
The protocol involves training individuals to increase or decrease specific brainwave activity at the targeted locations to improve attention, impulse control, and executive function.
Theta/Beta Ratio Training
This protocol aims to balance theta (4-8 Hz) and beta (15-20 Hz) wave activity to improve attention and reduce impulsivity.
- Target Brainwaves: Theta (4-8 Hz) and Beta (15-20 Hz)
- Goal: Decrease theta activity and increase beta activity to improve cognitive control and reduce symptoms of ADHD.
Procedure:
1. Electrode Placement: Place electrodes at Fz and Cz (reference).
2. Baseline Recording: Record baseline theta and beta activity for 5-10 minutes.
3. Feedback Mechanism: Provide real-time feedback using visual (e.g., a game or moving bar) or auditory (e.g., tone) cues. Positive feedback occurs when theta decreases and beta increases.
4. Training Sessions: Conduct 20-30 minutes of training sessions, 2-3 times per week, for 20-40 sessions.
5. Progress Monitoring: Utilize attention and impulse control scales and follow-up qEEG to track progress.
SMR Training Protocol
This protocol focuses on increasing sensorimotor rhythm (SMR, 12-15 Hz) activity to enhance motor inhibition and reduce hyperactivity.
- Target Brainwaves: SMR (12-15 Hz)
- Goal: Increase SMR activity to enhance motor inhibition and promote calmness.
Procedure:
1. Electrode Placement: Place electrodes at C3 (left sensorimotor cortex) and Cz (reference).
2. Baseline Recording: Record baseline SMR activity for 5-10 minutes.
3. Feedback Mechanism: Provide real-time feedback using visual or auditory cues. Positive feedback is given when SMR activity increases.
4. Training Sessions: Conduct 20-30 minutes of training sessions, 2-3 times per week, for 20-40 sessions.
5. Progress Monitoring: Use attention and hyperactivity rating scales and follow-up qEEG to monitor changes.
Alpha/Theta Training
This protocol balances alpha (8-12 Hz) and theta (4-8 Hz) waves to promote relaxation and improve cognitive control.
- Target Brainwaves: Alpha waves (8-12 Hz) and Theta waves (4-8 Hz)
- Goal: Increase alpha activity and decrease theta activity to enhance relaxation and attention.
Procedure:
1. Electrode Placement: Place electrodes at Fz and Cz (reference).
2. Baseline Recording: Record baseline alpha and theta activity for 5-10 minutes.
3. Feedback Mechanism: Use calming visual or auditory feedback. Positive feedback is provided when alpha increases, and theta decreases.
4. Training Sessions: Conduct 20-30 minutes of training sessions, 2-3 times per week, for 20-40 sessions.
5. Progress Monitoring: Use attention and relaxation scales and follow-up qEEG to monitor changes.
Effectiveness of Neurofeedback Therapy for ADHD management
Moreover, long-term follow-up studies with children who have been successfully treated with neurofeedback have shown that the improved attention and memory abilities of these children remain stable long after treatment has ended. These children also learn to manage their emotional status in different stressful situations. In other words, abnormal brainwave patterns are permanently normalized without the use of toxic drugs. It is also important to note that drugs do not improve the child’s ability to learn, but neurofeedback therapy for ADHD does.
Research indicates that neurofeedback is most effective for children over six years old with average or high intelligence. Usually, 30-50 treatment sessions (30-45 minutes each) are required for successful treatment at a rate of 2-3 sessions per week.
After 1-5 sessions
6 -10 sessions
11 – 20 sessions
20+ sessions
HOME USE DEVICE FOR NEUROFEEDBACK FOR ADHD MANAGEMENT
Neurofeedback Devices for Personal and Medical Use
Neurofeedback devices serve medical and non-medical purposes, with a fine line between the two. The non-medical use of neurofeedback often focuses on personal improvement, helping users enhance relaxation, attention, focus, concentration, and self-awareness. It can also support activities like meditation, counseling, or hypnosis, and even aid in achieving altered states of consciousness. These applications can be done without professional intervention. However, when neurofeedback is used to address a medical condition, such as relieving symptoms of a disorder, professional help becomes necessary.
Although neurofeedback systems are designed to let users control a computer for recreational, educational, or entertainment purposes, they are not considered medical instruments. Detailed information about various neurofeedback devices for home use, including methods and indications, is available online. A device claiming to aid in relaxation or alleviate symptoms related to a disorder is considered a medical device. The primary difference lies in how the device is marketed and utilized—whether for personal improvement or medical treatment.
Distinctions Between Medical and Non-Medical Neurofeedback
While both medical and non-medical neurofeedback systems share similar functions, their use depends on user intent and labeling. The benefits of neurofeedback may differ in either context, but the expectations and applications set them apart. For example, using neurofeedback to improve attention and concentration could be considered a personal improvement tool. However, if it’s employed to address conditions like Attention Deficit Hyperactivity Disorder (ADHD), it may fall under medical treatment.
Neurofeedback intended to reduce ADHD symptoms, especially if it is used to avoid stimulant medications like Ritalin, is generally considered medical. On the other hand, when parents, teachers, or counselors use neurofeedback in an educational setting to help a child achieve focused relaxation and academic improvement, the procedure is viewed as educational rather than medical treatment. The distinction relies on the purpose of the neurofeedback intervention.
Neurofeedback and the Brain’s Neuroplasticity
Neurofeedback capitalizes on neuroplasticity, the brain’s ability to change and adapt by forming new connections between nerve cells. This process occurs naturally whenever we learn a new skill, as the brain strengthens pathways that link different areas. The more these pathways are activated, the better the brain performs the associated tasks.
Neurofeedback therapy for ADHD is a type of learning where responses are shaped by their consequences. It provides ideal conditions for learning because it helps the brain recognize when it’s producing healthier brainwave patterns. This positive change is reinforced, and the user is given multiple opportunities to practice during a session. As the brain strengthens these healthier pathways, neurofeedback therapy for ADHD supports long-term focus, attention, and self-regulation improvement.
Excellent Brain ADHD Neurofeedback Home Training Kit




Neurosky Puzzlebox Orbit Bundle EEG Headset
Biofeedback Home Use Device
Various modalities of biofeedback, including Electromyography (EMG), Heart Rate Variability (HRV), Temperature, and Galvanic Skin Response (GSR), can also be utilized in the management of Attention-Deficit/Hyperactivity Disorder (ADHD). EMG biofeedback helps individuals gain awareness and control over muscle tension, which can reduce physical restlessness and hyperactivity often associated with ADHD. HRV biofeedback trains individuals to regulate their heart rate variability, promoting autonomic balance and improving emotional regulation and stress resilience. Temperature biofeedback involves monitoring peripheral skin temperature to enhance relaxation and decrease physiological arousal, thereby aiding concentration and impulse control. GSR biofeedback measures the skin’s electrical conductance, which varies in response to sweat gland activity and can provide insights into stress and arousal levels. By learning to modulate these physiological responses, individuals with ADHD can improve their focus, reduce impulsivity, and manage stress more effectively, complementing traditional neurofeedback approaches.
ADHD OTHER MANAGEMENT MEANS
DIET AND NATURAL SUPPLEMENT IN ADHD
- Proteins
- Balanced Meals
- B Vitamins
- Zinc, Iron, and Magnesium
- Multivitamins/ Multimineral
- Picamilon
- Proteins
Foods rich in protein, such as lean beef, pork, poultry, fish, eggs, beans, nuts, soy, and low-fat dairy products, can help alleviate symptoms of ADHD. The body uses Protein-rich foods to make neurotransmitters, the chemicals released by brain cells to communicate with each other. Protein can also prevent surges in blood sugar, which increases hyperactivity.
- Balanced Meals
A well-balanced diet, including vegetables, complex carbohydrates, fruits, and a sufficient amount of protein, tends to lead to behavior that is more consistently under control.
- B Vitamins
Studies suggest that B vitamin supplements may improve IQ scores and reduce aggression and antisocial behavior in children who are deficient in B vitamins. Vitamin B-6 may also increase the brain’s
levels of dopamine, a neurotransmitter that improves alertness.
- Zinc, Iron, and Magnesium
Zinc synthesizes dopamine and boosts the effects of some ADHD stimulant medications, such as Ritalin and Concerta; low levels of zinc correlate with inattention. Iron is also necessary for making dopamine; low levels of iron may cause cognitive deficits and severe ADHD. Adequate magnesium levels keep the brain calm.
- Multivitamins/Multiminerals
Daily recommended values of vitamins and minerals are essential for any child, especially one with ADHD. A daily multivitamin/multimineral will ensure that he gets what he needs.
- Picamilon
Combining the B-vitamin niacin and gamma-aminobutyric acid, picamilon improves blood flow to the brain. It has been shown to improve alertness and attention, as well as reduce aggressive behavior.
OMEGA 3 IN ADHD MANAGEMENT
Omega-3 Fatty Acids and Brain Health Throughout Life
It is now widely recognized that omega-3 fatty acids play a crucial role in brain health. Our needs for EPA (Eicosapentaenoic Acid) and DHA (Docosahexaenoic Acid) shift throughout life, meaning the optimal balance of these fatty acids in our diet also changes. For children, DHA is essential for growth and development. The brain, central nervous system (CNS), and retina rely heavily on DHA during fetal development, and this need continues into early childhood.
Children under five, in particular, require DHA to support their brain and CNS development. If they take omega-3 supplements, they must ensure they contain DHA to meet their developmental needs.
Changing Omega-3 Needs and the Role of EPA
As children grow older, particularly after age five, their brain and CNS development slows down. At this stage, their need for DHA decreases, and increasing the intake of EPA becomes essential. Studies have shown that EPA is beneficial for improving children’s behavior, academic performance, focus, and attention. Additionally, it can help reduce aggression.
For adolescents and adults, EPA remains in high demand. Research strongly correlates low EPA levels with a higher risk of mental health issues such as depression, dyslexia, and dyspraxia. Low levels of EPA are also linked to physical health problems, including heart disease, joint and bone conditions, and neurodegenerative diseases like multiple sclerosis (MS) and Parkinson’s disease. Fortunately, most of the body’s EPA needs can be met by consuming EPA-rich oils, fish, marine products, organic greens, and pastured animal products.
Omega-3 for ADHD and Recommended Supplementation
Recent studies suggest that children with ADHD may have omega-3 deficiencies, and taking a daily omega-3 supplement could help reduce symptoms while improving focus and cognitive function. Although researchers have not yet determined the optimal omega-3 dosage for ADHD, it is generally recommended that children between the ages of four and six start with a 500 mg daily supplement of omega-3; for children aged seven and older, a 1000 mg dosage is advised.
The most effective omega-3 supplements for managing ADHD symptoms contain an EPA-to-DHA ratio of 2:1 and Vitamin E. One highly effective supplement is eVitamins Ultra Omega 3, which provides 750 mg of omega-3, 500 mg of EPA, and 250 mg of DHA. This combination has shown an 85% effectiveness rate in reducing ADHD symptoms, with effects lasting up to six months.
SPORT IN ADHD MANAGEMENT
The Impact of Physical Activity on Children with ADHD
Regular physical activity, even just 30 minutes to an hour a day, can make a huge difference in a child’s mental and physical health, particularly for those with ADHD. Active children with ADHD often sleep better and experience fewer emotional outbursts at home and school. Being part of a team or learning the rules of a new activity provides structure, organization, and a sense of accomplishment. Involvement in sports also helps children develop communication and social skills, improve coordination, and build self-esteem. Additionally, exercise lowers the risk of depression, which is a common concern for people with ADHD.
Social and Emotional Benefits of Sports for Children with ADHD
Sports offer both physical fitness and social interaction, which can be particularly beneficial for children with ADHD. These activities help them bond with peers, come out of their shells, and build friendships. Finding an activity that helps them gain confidence and self-esteem is essential. Sports offer a healthy alternative to isolating behaviors, such as sitting alone or spending excessive time in front of the television. By engaging in physical activities, children with ADHD can benefit from improved self-confidence and social skills, which in turn positively impact their overall well-being.
Choosing the Right Sport for Your Child
When deciding which sport is best for your child with ADHD, involve them in the decision-making process. Ask what interests them, and support their choices. If they enjoy their work, they’re more likely to excel and have a great time. Many kids are exposed to different athletic activities at school, camp, or after-school programs, allowing them to discover what they like most.
The best after-school activities for kids with ADHD often include swimming, track and field, cross-country, horseback riding, tennis, baseball, basketball, gymnastics, martial arts, soccer, wrestling, and archery. Your child might take a few tries to find the right fit, so try different activities in various seasons. Be patient, and let them explore their interests at their own pace. Never underestimate your child’s potential just because they have ADHD.
Many successful individuals, including athletes like Michael Phelps, Simone Biles, Michael Jordan, and Terry Bradshaw, have thrived despite having ADHD. Artists like Jim Carrey, Adam Levine, and writer Jenny Lawson have shared their inspiring stories of living with and succeeding despite ADHD.
Frequently Asked Questions about Neurofeedback Therapy for ADHD
Neurofeedback can be as effective as psychostimulant medications like Ritalin in reducing ADHD symptoms. A key advantage is that its effects are often long-lasting after a full course of treatment, unlike medication, which only works while active in the system.
The primary patterns are:
- Excessive Theta Waves: Linked to daydreaming and inattention.
- Reduced Beta Waves: Linked to focus and impulse control.
- High Theta/Beta Ratio: This is a significant biomarker for ADHD. The main protocol involves suppressing theta waves and enhancing beta waves.
Improvements are gradual. The research shows symptom reduction of 37% after 2 sessions, 60% after 10 sessions, and 78% after 20 sessions. Significant improvements in attention and memory are typically seen after 11-20 sessions.
A successful treatment typically requires 30 to 50 sessions, each lasting 30 to 45 minutes. These sessions are typically conducted at a rate of 2-3 times per week to ensure consistency and optimal results.
Yes, there are personal-use best neurofeedback devices for ADHD (such as Mendi, NeuroSky, NeuroVizr, etc.) that allow for home training. These devices often use video games that respond to your brainwaves, providing real-time feedback. However, for medical treatment of ADHD symptoms, professional guidance is recommended.
Neurofeedback leverages the brain’s neuroplasticity—its ability to form new neural connections. By repeatedly rewarding the brain for producing healthier wave patterns, it “learns” and strengthens these pathways. This creates a new, stable baseline for focus and behavior, reducing the need for ongoing treatment.




















Thanks for the great article!
WOW just what I was looking for. Came here by searching for
ADHD holistic approaches
Thanks for the great article!
Thanks for the great article!
Valuable information. Lucky me, I found your website by accident! I bookmarked it.