Urinary incontinence (UI), a prevalent condition affecting individuals across various age groups, can profoundly impact one’s quality of life. The involuntary loss of bladder control can lead to not only physical discomfort but also emotional and social challenges. In pursuing innovative and effective solutions, medical research and treatment has turned its attention to the promising biofeedback technique. Biofeedback therapy pelvic floor for urinary incontinence offers a transformative path to regain control and confidence. Urinary incontinence, affecting countless lives, stems from multifaceted factors like muscle weakness and bladder overactivity. Pelvic floor biofeedback bridges this gap by facilitating real-time communication with the body. Individuals learn to interpret and influence physiological responses through sensors and personalized cues, targeting the root causes.
Table of Contents
Toggle- What urinary incontinence is?
- What are the four types of urinary incontinence?
- What are the causes of urinary incontinence?
- The mechanism of urinary incontinence
- Treatment of urinary incontinence
- Pelvic Floor Muscle Exercises (Kegel Exercises)
- Auxiliary muscles exercise in urinary incontinence
- EMG Pelvic floor biofeedback for urinary incontinence
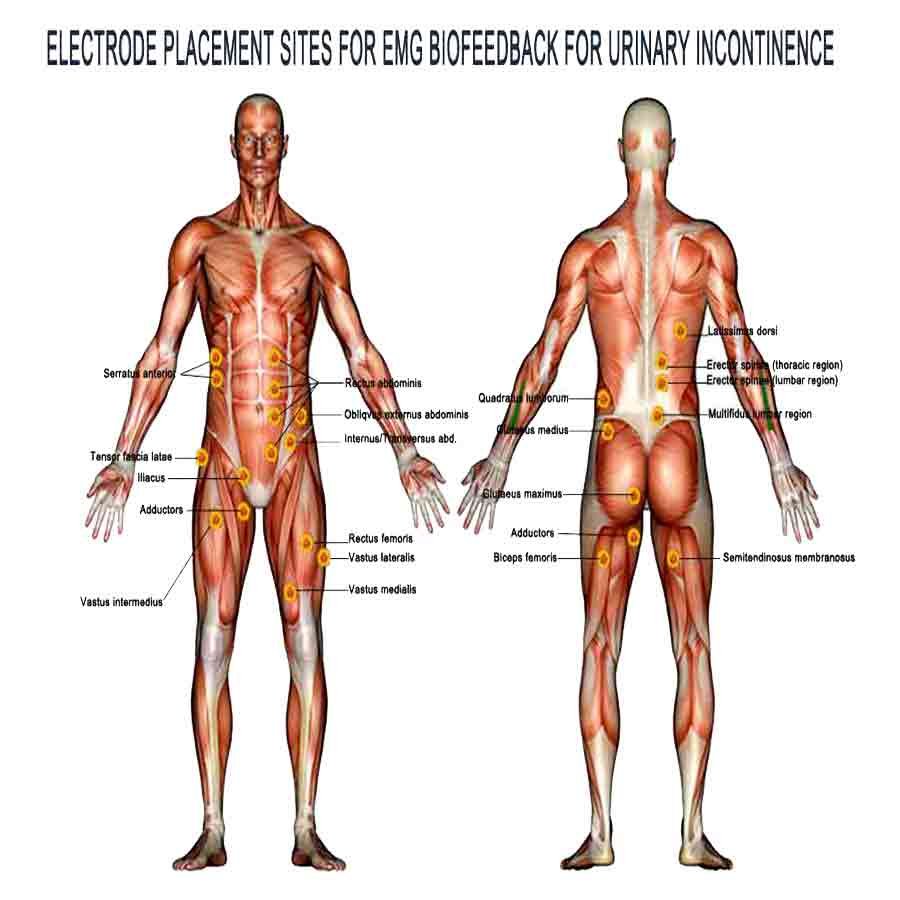
- Electromyographic (EMG) biofeedback for auxiliary muscles in UI
- Sacral Area Biofeedback
- Auxiliary Muscles and Pelvic Floor Biofeedback Device for Personal Use
What urinary incontinence is?
Urinary incontinence (UI) refers to the involuntary loss of bladder control, leading to the unintentional leakage of urine. It’s a common condition that can range in severity from occasional minor leaks to complete loss of bladder control. This loss of power can occur during activities such as coughing, sneezing, laughing, lifting, or even during sudden urgency to urinate.
According to the World Health Organization, the prevalence of urinary incontinence reported in population-based studies ranges from 9.9% to 36.1%. It is twice as high in older women as in older men. UI can occur at any age, but it is more common among women over 50. Urinary incontinence may be a temporary condition that results from an underlying medical condition. It can range from the discomfort of slight urine losses to severe, frequent wetting.
Urinary incontinence can result from various factors. These factors include weakened pelvic floor muscles, overactive bladder muscles, nerve damage, hormonal changes, and certain medical conditions. Additionally, urinary incontinence can affect people of all ages and genders. However, it is more prevalent among older adults and women, particularly after childbirth or during menopause.
What are the four types of urinary incontinence?
There are four types of urinary incontinence: urgency, stress, overflow, and neurogenic incontinence.
Stress Urinary Incontinence
The most common type of stress urinary incontinence concerns urine leakage associated with physical exertion, coughing, and sneezing. Weakness or damage to the pelvic floor muscles and tissues that support the bladder and urethra can result in stress incontinence.
During activities that increase intra-abdominal pressure, such as sneezing, coughing, laughing, or lifting, the bladder’s pressure exceeds the weakened muscles’ ability to keep the urethra closed. Women commonly experience stress incontinence, especially after childbirth, often due to weakened pelvic floor muscles or damaged urethral sphincters, which leads to urine leakage. Stress incontinence usually results from weakened or stretched pelvic floor muscles and tissues supporting the bladder and urethra. Factors such as pregnancy, childbirth, obesity, hormonal changes, or aging can contribute to this weakening.
Urgency urinary incontinence
Overactive bladder (OAB) causes a sudden and intense urge to urinate, often leading to involuntary urine leakage before reaching a restroom. Individuals with urgency incontinence frequently experience an uncontrollable need to urinate throughout the day and night. This condition primarily arises from involuntary contractions of the bladder’s detrusor muscle, which triggers a strong sense of urgency. Various factors contribute to this type of incontinence. For example, neurological conditions, bladder irritation, certain medications, and infections can all play a role. Additionally, sometimes the cause remains unknown.
Overflow and Neurogenic Urinary Incontinence
Overflow urinary incontinence is characterized by frequent or constant dribbling of urine from the bladder, often with the sensation of incomplete bladder emptying. Individuals may also experience difficulty initiating urination and a weak urinary stream. This type of incontinence is typically caused by an obstruction or blockage in the urinary tract, which prevents the bladder from emptying fully. Common causes include an enlarged prostate in men, urinary stones, constipation, or nerve damage that affects bladder contraction.
Neurogenic urinary incontinence occurs when there is a disruption in the regular communication between the nervous system and the bladder. Depending on which nerves are affected, It can manifest as overactive or underactive bladder function. Neurogenic incontinence can result from various neurological conditions or injuries, such as multiple sclerosis, Parkinson’s disease, spinal cord injuries, or stroke. These conditions can disrupt the coordination between the brain, spinal cord, and bladder, leading to frequent and urgent voiding (overactive bladder) or an inability to empty the bladder (underactive bladder).
What are the causes of urinary incontinence?
Urinary incontinence can be caused by various factors that affect the normal function of the urinary system. Some common causes include:
Common Causes of Urinary Incontinence
1. Weak Pelvic Floor Muscles
Weakened pelvic floor muscles, often due to childbirth, aging, or obesity, can lead to stress incontinence, where pressure on the bladder from activities like sneezing, laughing, or lifting causes urine leakage.
2. Overactive Bladder Muscles
When the muscles of the bladder contract involuntarily, creating a strong urge to urinate, it can result in urge incontinence or “overactive bladder.” Various factors, including neurological conditions, infections, and certain medications, can cause this.
3. Neurological Disorders
Conditions that affect the nervous system, such as multiple sclerosis, Parkinson’s disease, and stroke, can disrupt the signals between the brain and the bladder, leading to various types of incontinence.
4. Hormonal Changes
Hormonal fluctuations, especially in women during menopause, can lead to changes in the lining of the urethra and the bladder’s ability to store urine, contributing to incontinence.
5. Prostate Issues
In men, an enlarged prostate gland (benign prostatic hyperplasia) or prostate surgery can impact bladder control and lead to incontinence.
6. Urinary Tract Infections
Infections in the urinary tract can cause irritation and overactivity of the bladder, resulting in temporary incontinence.
Additional Causes of Urinary Incontinence
7. Obstruction
An obstruction in the urinary tract, such as kidney stones or tumors, can disrupt urine flow and cause overflow incontinence.
8. Medications
Certain medications, like diuretics, sedatives, and alpha-blockers, can affect bladder function and contribute to incontinence.
9. Chronic Coughing
Conditions such as chronic bronchitis or smoking-related lung diseases can lead to chronic coughing, which can put stress on the pelvic muscles and lead to stress incontinence.
10. Physical Impairments
Mobility issues or physical disabilities that hinder a person’s ability to reach a restroom in time can contribute to functional incontinence.
11. Genetics
Some individuals may be genetically predisposed to developing weak pelvic floor muscles or other anatomical factors that increase the risk of incontinence.
12. Lifestyle Factors
Obesity, excessive caffeine or alcohol consumption, and inadequate fluid intake can exacerbate urinary incontinence symptoms.
Understanding the underlying cause of urinary incontinence is crucial for proper diagnosis and effective treatment.
The mechanism of urinary incontinence
The mechanism of urinary incontinence is closely tied to the role of pelvic floor muscles. Pelvic floor muscles are a group of skeletal muscles that form a sling-like structure at the base of the pelvis. These muscles are crucial for maintaining urinary continence. Here’s how they function:
1. Support: Pelvic floor muscles provide essential support to the bladder and other pelvic organs, keeping them in their proper position.
2. Sphincteric Function: The pelvic floor muscles encircle the urethra and the anal canal. They play a significant role in maintaining the closure of the urethra and preventing involuntary urine leakage. When these muscles contract, they compress the urethra, keeping it closed.
3. Voluntary Control: The external urethral sphincter, a part of the pelvic floor muscles, allows voluntary control over urination. When you choose to urinate, this muscle relaxes, releasing urine. When you want to delay or stop urination, the external urethral sphincter contracts to close off the urethra.
Pelvic Floor Muscles and Contributing Factors
The pelvic floor consists of layers of muscles and connective tissues connecting those muscles (ligaments) and wraps around the entirety of the pelvis. Two main muscles intertwine to form pelvic floor muscles:
• Levator ani composes the bulk of the pelvic floor muscles and consists of three separate muscle components:
– pubococcygeus,
– puborectalis and
– iliococcygeus.
• The coccygeus is the more minor muscle component in the pelvic floor muscles. It’s located toward the back of the pelvis.
Factors Affecting Pelvic Floor Muscles
Pelvic floor muscles can weaken due to injury or trauma, including childbirth and surgery. They can become stressed during pregnancy or from overuse (repeated heavy lifting, chronic coughing, constipation). They may grow weaker due to hormone changes during menopause and lose strength as a natural part of aging. Conditions like diabetes may also play a role in weakening pelvic floor muscles.
Understanding the role of pelvic floor muscles in maintaining continence and recognizing the factors that disrupt this balance is essential for diagnosing and effectively treating urinary incontinence. Strengthening these muscles through Kegel exercises can be a valuable part of managing certain types of incontinence, particularly stress incontinence. However, treatment approaches vary depending on the specific type and underlying causes of incontinence.
Common signs and symptoms of urinary incontinence include:
- Leaking urine when coughing, sneezing, laughing, or exercising.
- Feeling sudden, uncontrollable urges to urinate.
- Frequent urination.
Waking up many times at night to urinate. - Urinating during sleep.
Although pelvic floor muscles are hidden, they can be consciously controlled and trained, such as the arm, leg, or abdominal (tummy) muscles. Strengthening pelvic floor muscles will help actively support and maintain the bladder, reducing the likelihood of accidentally leaking from the bladder. Like other muscles in the body, pelvic floor muscles will become more robust with a regular exercise program. This is important for both men and women.
Treatment of urinary incontinence
The treatment of urinary incontinence varies based on the type and underlying causes of the condition. Here are some treatment approaches for different types of urinary incontinence:
1. Behavioral Interventions:
Behavioral interventions involve modifying habits and patterns that contribute to urinary incontinence. These include bladder training, scheduled voiding, and fluid and diet management to reduce irritants and excessive urine production.
- Bladder Training: This technique involves gradually increasing the time between trips to the restroom to improve bladder capacity and reduce the frequency of urge incontinence.
- Scheduled Voiding: Establishing a regular bladder emptying schedule can help manage urge and overflow incontinence by preventing overfilling or constant dribbling.
- Fluid and Diet Management: Adjusting fluid intake, particularly reducing caffeine and alcohol consumption, can help decrease bladder irritability and excessive urine production.
2. Pelvic Floor Muscle Exercises (Kegel Exercises):
Kegel exercises strengthen the pelvic floor muscles that support the bladder and urethra. Improving muscle tone and control is effective in reducing stress and urge incontinence.
- Stress Incontinence: Strengthening the pelvic floor muscles through Kegel exercises can provide better bladder support and reduce stress incontinence episodes.
- Urge Incontinence: Kegel exercises can also help individuals gain better control over their bladder and reduce urgency.
3. Medications:
Medications can help manage urinary incontinence by reducing overactive bladder contractions or relaxing bladder muscles. Anticholinergics and beta-3 adrenergic agonists are commonly prescribed for urge incontinence.
- Anticholinergics: These medications relax the bladder muscles and reduce spasms, making them helpful in treating urge incontinence. Examples include oxybutynin, tolterodine, and solifenacin.
- Beta-3 Adrenergic Agonists: Some medications like mirabegron can increase bladder capacity and decrease the frequency of contractions, helping with both urgency and frequency.
4. Medical Devices:
Medical devices, such as pessaries, support the bladder and urethra, temporarily relieving stress incontinence. Additionally, urethral inserts can prevent leakage during specific activities. These devices help manage symptoms effectively for individuals dealing with stress incontinence.
- Pessaries: A pessary is a device inserted into the vagina to provide support to the urethra and bladder, helping manage stress incontinence.
- Urethral Inserts: These are tampon-like disposable devices that can be inserted into the urethra to prevent leakage during specific activities.
5. Incontinence Pads and Products:
- Absorbent pads and adult diapers can provide temporary relief and increased confidence, especially for individuals with more severe incontinence.
6. Surgery:
Surgical options are considered for more severe cases of urinary incontinence. Procedures like sling placement or bladder neck suspension can support the urethra for stress incontinence.
- Sling Procedures: Surgical sling placement under the urethra or bladder neck can provide additional support to prevent stress incontinence.
- Bladder Neck Suspension: A surgical procedure that supports the bladder, neck, and urethra to treat stress incontinence.
- Artificial Urinary Sphincter: For severe cases of stress incontinence, an artificial urinary sphincter can be implanted to provide manual control over the urethral opening.
Advanced and Complementary Treatments
7. Pelvic floor biofeedback:
Pelvic floor biofeedback is a non-invasive technique that uses sensors to provide real-time feedback about muscle activity and bladder function. For urinary incontinence, biofeedback therapy pelvic floor assists in training individuals to strengthen pelvic floor muscles for stress incontinence and gain control over bladder contractions for urge incontinence.
- Pelvic floor biofeedback for urinary incontinence and pelvic floor muscle retraining are treatments that help patients learn to strengthen or relax their pelvic floor muscles to improve bowel or bladder function and decrease some types of pelvic floor pain.
- Auxiliary muscles biofeedback: In addition to pelvic floor muscles, several other muscle groups, such as abdominal, gluteal, quadriceps, etc., can play a role in managing urinary incontinence, depending on the type and underlying causes of the condition. EMG pelvic floor biofeedback is a valuable therapeutic technique used to target and train various muscle groups beyond the pelvic floor muscles in managing urinary incontinence, depending on the specific type and causes of the condition.
8. Neuromodulation:
- Sacral Nerve Stimulation: Electrical stimulation of the sacral nerves can help regulate bladder function and treat urge incontinence.
9. Botox Injections:
- Botox injections into the bladder muscle can help control overactive bladder symptoms by temporarily relaxing the muscle and reducing spasms.
10. Lifestyle Modifications:
- Maintaining a healthy weight, avoiding constipation, practicing good hygiene, and managing chronic cough can help alleviate urinary incontinence symptoms.
It’s important to note that appropriate treatment depends on a thorough evaluation by a healthcare professional. The professional will consider factors such as the type and severity of incontinence, underlying causes, the individual’s overall health, and preferences. A comprehensive treatment plan may involve a combination of approaches, with pelvic floor biofeedback playing a pivotal role in empowering individuals to gain control over their bodily functions and improve their quality of life.
Pelvic Floor Muscle Exercises (Kegel Exercises)
In urinary incontinence, particularly stress and some urge incontinence, targeting and strengthening the pelvic floor muscles is essential. These muscles support the bladder, urethra, and other pelvic organs and are directly involved in urinary control. Strengthening these muscles can improve their ability to contract and relax appropriately, helping to prevent leakage and improve bladder control.
1. Support: Pelvic floor muscles support the bladder, helping keep it in its proper position.
2. Sphincteric Function: These muscles help maintain closure of the urethra, preventing urine leakage when there is increased abdominal pressure (as in stress incontinence).
3. Urge Control: Strong pelvic floor muscles can also help suppress sudden urination urges (as in some forms of urge incontinence) by providing better voluntary control.
Pelvic floor muscle exercises, often called Kegel exercises, are designed to target and strengthen these muscles. Kegel exercises can effectively reduce urinary incontinence episodes and improve overall bladder control when done correctly and regularly.
To perform Kegel exercises:
1. Locate the Muscles: Identify the pelvic floor muscles by trying to stop urine flow during urination. The muscles you engage to do this are the ones you’ll be working on during Kegel exercises.
2. Isolate the Muscles: Once you’ve identified the muscles, practice contracting and relaxing them without using other muscles, such as the abdomen or buttocks.
3. Start Slowly with short contractions, hold for a few seconds, and then relax. Gradually increase the duration and intensity of the contractions as you become more comfortable.
4. Be Consistent: Perform these exercises regularly. Aiming for several sets of 10 repetitions is often recommended throughout the day.
Remember that it’s crucial to perform Kegel exercises correctly to avoid straining other muscles and effectively target the pelvic floor muscles. If you’re uncertain how to do Kegel exercises correctly, consider consulting a healthcare professional or a pelvic floor physical therapist who can provide guidance and personalized instructions. Additionally, pelvic floor biofeedback techniques can assist in ensuring that you’re engaging the right muscles during pelvic floor exercises, enhancing their effectiveness in managing urinary incontinence.
Auxiliary muscles exercise in urinary incontinence
In addition to pelvic floor muscles, several other muscle groups can play a role in managing urinary incontinence, depending on the type and underlying causes of the condition. Here are some of the muscles and muscle groups that may be involved in the treatment of urinary incontinence:
Muscle Groups Contributing to Urinary Incontinence Management
1. Abdominal Muscles (Transverse Abdominis): Strengthening the transverse abdominis, the deepest layer of abdominal muscles, can help support the pelvic organs and reduce pressure on the bladder. This is particularly relevant for stress incontinence.
2. Oblique Abdominal Muscles: The internal and external oblique muscles can help stabilize the trunk and support the pelvic area. Exercises that engage these muscles can assist in managing stress incontinence.
3. Gluteal Muscles: The gluteal muscles (buttocks) play a role in pelvic stability and posture. Strengthening these muscles can help maintain proper pelvic alignment and contribute to better overall pelvic health.
4. Thigh Muscles (Quadriceps and Hamstrings): Strong thigh muscles can assist in activities like rising from a seated position and maintaining balance, which can reduce the risk of falls and related stress incontinence.
5. Lower Back Muscles (Erector Spinae): Strengthening the lower back muscles can help support the spine and maintain proper posture, indirectly contributing to pelvic health.
Additional Muscle Groups Impacting Urinary Health
6. Diaphragm: The primary breathing muscle is connected to the pelvic floor through the core muscles. Learning to engage and coordinate the diaphragm with the pelvic floor can assist in overall core stability and urinary control.
7. Hip Adductors and Abductors: The muscles responsible for moving the thighs toward or away from the body’s midline can impact pelvic stability and balance.
It’s important to note that while these muscle groups can indirectly influence urinary continence, the primary focus for addressing urinary incontinence remains the pelvic floor muscles. Strengthening the pelvic floor muscles through exercises like Kegel exercises is usually the first-line approach for treating stress incontinence and some forms of urge incontinence.
However, a comprehensive approach to managing urinary incontinence may include exercises that engage these other muscle groups as part of a broader physical therapy or rehabilitation program. Additionally, maintaining overall physical fitness, which involves working on various muscle groups, can contribute to improved pelvic health and better urinary control. Consultation with a healthcare professional or a pelvic floor physical therapist can help design a personalized exercise regimen tailored to your specific needs and condition.
EMG Pelvic floor biofeedback for urinary incontinence
What pelvic floor biofeedback muscle retraining is?
Pelvic floor biofeedback muscle retraining is a treatment to help patients learn to strengthen or relax their pelvic floor muscles to improve bowel or bladder function. It is a painless process that uses special sensors and a computer or mobile phone monitor to display information about muscle activity. This information or “feedback” is used to gain sensitivity and, with practice, control over pelvic floor muscle function. An essential part of biofeedback therapy pelvic floor is the consistent practice of pelvic floor muscle exercises at home. With pelvic floor biofeedback, an individual can learn to stop using the incorrect muscles and start using the correct ones.
Biofeedback for pelvic floor has shown promising effectiveness in managing urinary incontinence, particularly for conditions like stress and urge incontinence. This non-invasive technique utilizes real-time physiological data to help individuals gain awareness and control over their pelvic floor muscles and bladder function. Here’s how pelvic floor biofeedback proves effective:
Stress Incontinence: Pelvic floor biofeedback helps individuals strengthen their pelvic floor muscles, which are crucial for supporting the bladder and preventing leakage during activities that increase intra-abdominal pressure. Individuals can learn proper muscle engagement techniques by providing visual or auditory cues that indicate when the correct muscles are being contracted. Over time, consistent practice guided by pelvic floor biofeedback can improve muscle strength and endurance, reducing or eliminating stress incontinence episodes.
Urge Incontinence (Overactive Bladder): Pelvic floor biofeedback assists in training individuals to recognize the early signs of an impending urge to urinate. By monitoring bladder contractions and providing feedback when the bladder muscles start to contract involuntarily, individuals can learn to control these and suppress the urge. This technique empowers individuals to retrain their bladder and enhance their ability to delay urination until an appropriate time and place.
Efficacy and Benefits of pelvic floor biofeedback
Numerous clinical studies have demonstrated the effectiveness of pelvic floor biofeedback in reducing urinary incontinence episodes and improving overall bladder control. It offers several benefits, including:
1. Personalized Training: Pelvic floor biofeedback tailors training to an individual’s specific needs, adapting to their progress and challenges.
2. Non-Invasive: Unlike surgical interventions, pelvic floor biofeedback is non-invasive and carries minimal risks or side effects.
3. Empowerment: By providing real-time feedback, individuals feel empowered and engaged in their treatment process.
4. Holistic Approach: Pelvic floor biofeedback complements other treatment options, such as pelvic floor exercises and lifestyle modifications.
5. Psychological Well-being: Gaining control over bladder function often improves self-esteem, confidence, and emotional well-being.
6. Long-Term Benefits: Consistent pelvic floor biofeedback training can lead to sustainable improvements, reducing the need for medication or more invasive procedures.
While pelvic floor biofeedback offers promising outcomes, its effectiveness can vary based on individual commitment, incontinence severity, and skilled healthcare professionals’ guidance. Combining pelvic floor biofeedback with other strategies, such as exercises and behavioral modifications, can enhance its overall impact. As technology advances and research continues, biofeedback holds the potential to play an increasingly significant
Electromyographic (EMG) biofeedback for auxiliary muscles in UI
Electromyographic (EMG) biofeedback is a valuable therapeutic technique used to target and train various muscle groups beyond the pelvic floor muscles in managing urinary incontinence, depending on the specific type and causes of the condition.
Here’s how EMG auxiliary muscle biofeedback can be employed for these purposes:
1. Abdominal Muscles (Transverse Abdominis and Obliques):
• Purpose: Strengthening the transverse abdominis and oblique abdominal muscles can provide additional support to the pelvic area, reducing pressure on the bladder and assisting in managing stress incontinence.
• EMG sensors can be placed on the abdominal muscles to monitor their activity during specific exercises. Patients can visualize this activity on a screen or receive auditory cues, helping them learn to engage and strengthen these muscles effectively.
2. Lower Back Muscles (Erector Spinae):
• Purpose: Strengthening the erector spinae muscles can contribute to better spinal stability and posture, indirectly influencing pelvic health and urinary control.
• EMG sensors can be positioned on the lower back muscles, allowing patients to monitor muscle engagement and ensure they target the correct muscles during exercises.
3. Hip Muscles (Adductors and Abductors):
• Purpose: The hip adductors and abductors play a role in pelvic stability and balance, which can affect urinary control.
• EMG biofeedback can be used to assess the activity of these hip muscles during specific movements or exercises, helping individuals focus on improving their strength and coordination in this area.
4. Diaphragm:
• Purpose: Coordinating the diaphragm with pelvic floor muscles and other core muscles can enhance overall core stability and control, indirectly impacting urinary continence.
• EMG sensors placed on the diaphragm can assist individuals in learning to coordinate their activity with the pelvic floor and other muscle groups during exercises to improve core strength and stability.
How EMG biofeedback for auxiliary muscles works
• EMG biofeedback involves the placement of sensors or electrodes on the targeted muscle groups. These sensors detect and record the electrical activity generated by muscle contractions.
• The EMG signals are then transmitted to a monitoring device, a computer screen, or an auditory feedback system.
• Patients receive real-time visual or auditory cues based on their muscle activity. This feedback allows them to observe and adjust muscle engagement, ensuring they target the right muscles and use proper exercise techniques.
• Over time, patients can learn to control and strengthen these muscle groups effectively, which can contribute to improved bladder control and the management of urinary incontinence.
EMG biofeedback can be particularly beneficial when working on specific muscle groups to complement other treatment approaches, such as pelvic floor exercises. It helps individuals gain awareness of muscle activity and ensures that exercises are performed correctly, ultimately enhancing the effectiveness of the overall incontinence management plan.
Sacral Area Biofeedback
This area biofeedback and stimulation are therapeutic approaches used in the treatment of urinary incontinence, particularly for certain types of incontinence, such as overactive bladder (urge incontinence) and some cases of mixed incontinence.
Sacral area biofeedback involves using sensors or electrodes placed on or near the sacral area, which is the region at the base of the spine near the tailbone. These sensors detect electrical or muscular activity in the pelvic floor and bladder muscles. Here’s an overview of these techniques:
• Mechanism: During biofeedback sessions, the sensors provide real-time information on the pelvic floor muscles and bladder activity. Patients can see this feedback on a monitor, making them aware of muscle contractions and bladder function.
• Benefits: Sacral area biofeedback helps individuals learn to control pelvic floor muscles more effectively, improve coordination, and increase the ability to suppress unwanted contractions. It can also enhance the relaxation of the bladder muscles when needed.
• Training: Biofeedback sessions are often conducted by trained healthcare professionals, such as pelvic floor physical therapists. These sessions guide patients in practicing muscle control techniques while monitoring their progress on the biofeedback display.
• Effectiveness: Sacral area biofeedback is particularly useful for people with urge incontinence or overactive bladder. It assists in training individuals to gain better control over bladder contractions, reduce urgency, and improve bladder capacity.
Sacral Nerve Stimulation (SNS)
Sacral nerve stimulation, or neuromodulation, involves implanting a device that sends electrical impulses to the sacral nerves involved in bladder control.
• Mechanism: The implanted device delivers controlled electrical stimulation to the sacral nerves, modulating their activity. This neuromodulation affects the communication between the brain, spinal cord, and bladder, helping to regulate bladder function.
• Benefits: SNS is typically recommended for individuals with overactive bladder symptoms who have not responded to conservative treatments. It can reduce urgency, frequency, and incontinence episodes.
• Procedure: The SNS device is surgically implanted, and a healthcare professional can adjust its settings externally. It is a reversible procedure, and if the individual does not experience relief or encounters side effects, the device can be turned off or removed.
• Effectiveness: SNS has shown promising results in treating overactive bladder, improving urinary symptoms, and the quality of life for many patients.
Both sacral area biofeedback and sacral nerve stimulation are typically considered after conservative treatments like pelvic floor exercises and medications have been tried without success. They offer alternative options for individuals who are seeking additional interventions to manage urinary incontinence, mainly when it is related to overactive bladder or neurological factors. These treatments are usually recommended and managed by urologists or healthcare providers with expertise in incontinence management.
Clinical studies have generally reported success rates ranging from around 60% to 90% regarding symptom improvement and quality of life. However, these success rates can vary widely depending on the study population, methodology, and duration of treatment.
Auxiliary Muscles and Pelvic Floor Biofeedback Device for Personal Use











You are actually a good webmaster. The web site loading speed is incredible.
It kind of feels that you’re doing any unique trick.
In addition, the contents are masterwork. you’ve performed a great task on this subject!
It’s actually a great and useful piece of information. I am happy that you simply shared this helpful info with
us. Please keep us up to date like this. Thanks for sharing.
I have to thank you for the efforts you’ve put in writing this blog. I’m hoping to see the same high-grade blog posts from you in the future as well.