Stuttering is an action-induced speech disorder with involuntary, audible, or silent repetitions or prolongations in the utterance of short speech elements (sounds, syllables) and words. Stuttering typically begins in childhood and may persist into adulthood. It can vary in severity, with some individuals experiencing only mild stuttering while others may have more pronounced difficulties speaking fluently. Treatment for stuttering often involves a combination of therapeutic approaches tailored to the individual’s needs and goals. Biofeedback speech therapy for stuttering is a therapeutic technique that can help individuals gain better control over physiological processes, such as muscle tension and stress, that may effectively contribute to stuttering. Several modalities of biofeedback speech therapy for stuttering can be used for treatment to help individuals gain better control over physiological processes that may contribute to disfluency.
Table of Contents
ToggleWhat stuttering is?
Stuttering, or stammering, is a speech disorder characterized by disruptions in the normal flow of speech. People who stutter may experience difficulty producing sounds, syllables, words, or phrases, manifesting as repetitions of sounds or words, prolongations of sounds, or blocking, where the person cannot produce any sound for a brief period. These disruptions in speech can be accompanied by physical tension, such as facial grimaces or rapid eye blinking, as well as feelings of frustration and anxiety.
Stuttering typically begins in childhood and may persist into adulthood. It can vary in severity, with some individuals experiencing only mild stuttering while others may have more pronounced difficulties speaking fluently. The exact cause of stuttering is not fully understood, but it is believed to result from genetic, neurological, and environmental factors.
Treatment for stuttering often involves speech therapy. In this approach, a trained speech-language pathologist works with individuals to enhance their fluency and reduce both the frequency and severity of stuttering episodes. Specifically, therapists may use techniques such as speech modification, fluency shaping, and stuttering modification. These methods aim to help individuals manage their speech more effectively. Furthermore, early intervention is crucial for children who stutter. By addressing the issue early, it is possible to prevent the disorder from becoming more ingrained and severe.
It’s important to note that stuttering does not reflect a person’s intelligence or competence, and many individuals who stutter lead successful lives and careers with appropriate support and therapy. Supportive environments and understanding from family, friends, and peers can also play a significant role in helping individuals with stuttering feel more confident and comfortable in their communication.
Pathophysiology of stuttering
The pathophysiology of stuttering, or the underlying biological and neurological processes contributing to the disorder, is not fully understood. Stuttering is believed to be a complex condition influenced by a combination of genetic, neurological, and environmental factors. While researchers continue to study the condition, no single, universally accepted theory explains all aspects of stuttering. However, several hypotheses have been proposed to shed light on the potential mechanisms involved:
Overview
1. Genetic Contributions: Evidence suggests that stuttering may have a genetic component. Studies have shown that stuttering tends to run in families, and certain genetic variations may increase susceptibility to the disorder. However, no specific “stuttering gene” has been identified, and genetics alone cannot account for all cases of stuttering.
2. Neurological Differences: Stuttering involves abnormalities in the brain’s speech-processing areas and neural pathways. Some studies have identified differences in brain structure and function in individuals who stutter. For example, there may be variations in the size or activity of regions like the left inferior frontal gyrus, which is involved in speech production and language processing.
Neural and Developmental Influences on Stuttering
3. Neural Processing Challenges: Stuttering may be associated with differences in how the brain processes speech and language. It is hypothesized that individuals who stutter may have difficulties with the timing and coordination of the neural circuits responsible for speech production, leading to disruptions in fluency.
4. Developmental Factors: Stuttering often begins in childhood during rapid language and speech development. Some researchers suggest that developmental factors, such as the rate at which a child’s speech and language skills develop, may contribute to stuttering. Children who experience a rapid increase in speech demands without a corresponding increase in their abilities for motor control of speech may be more susceptible to stuttering.
Environmental and Psychological Factors
5. Environmental and Emotional Influences: While genetic and neurological factors play a role, environmental and psychological factors can also influence the severity and persistence of stuttering. Stress, anxiety, and social pressure can exacerbate stuttering, while supportive and communicative environments can help individuals manage their stuttering more effectively.
It’s important to note that stuttering is a highly variable condition, and the pathophysiology may differ from one individual to another. Additionally, ongoing research continues to refine our understanding of the disorder, and new insights are regularly emerging. Speech-language pathologists and researchers work together to develop and refine therapies that address the specific needs of individuals who stutter, considering the complex interplay of genetic, neurological, and environmental factors.
Stuttering signs and symptoms
Stuttering signs and symptoms may include:
- Difficulty starting a word, phrase, or sentence,
- Prolonging a word or sounds within a word,
- Repetition of a sound, syllable, or word,
- Brief silence for certain syllables or words or pauses within a word (broken word),
- Addition of extra words such as “um” if difficulty moving to the next word is anticipated,
- Excess tension, tightness, or movement of the face or upper body to produce a word,
- Anxiety about talking,
- Limited ability to effectively communicate.
Classification of stuttering
Stuttering can be classified into several categories or types based on various factors, including its characteristics and presentation. The classification of stuttering helps clinicians and researchers understand the nature of the disorder and tailor treatment approaches accordingly. Here are some standard classifications of stuttering:
Types of Stuttering
1. Developmental Stuttering:
- Developmental stuttering is the most common type and typically begins in childhood as a child learns to speak.
- It often starts between 2 and 4 when language and speech skills develop.
- Developmental stuttering can vary in severity, and many children naturally outgrow it with age or through speech therapy.
2. Neurogenic Stuttering:
- Neurogenic stuttering is associated with neurological conditions or injuries that affect the brain’s speech centers or motor control.
- It can result from conditions such as strokes, traumatic brain injuries, or other neurological disorders.
• Neurogenic stuttering may have a sudden onset and typically occurs in adulthood.
3. Psychogenic Stuttering:
- Psychogenic stuttering is thought to be related to psychological factors and is often a response to stress, anxiety, or psychological trauma.
- It can occur suddenly and may resolve with appropriate psychological therapy or intervention.
4. Cluttering:
- Cluttering is a speech disorder characterized by rapid and disorganized speech, which may include frequent interruptions, irregular pacing, and unclear articulation.
- Unlike stuttering, which involves disruptions in speech flow, cluttering often involves overly rapid and hasty speech.
- Treatment for cluttering focuses on slowing down speech and improving articulation.
Additional Classifications
5. Acquired Stuttering:
- Acquired stuttering refers to stuttering that develops later in life due to specific events, such as head injuries, illnesses, or psychological trauma.
- It can be associated with sudden and noticeable changes in speech fluency.
6. Persistency:
- This classification considers whether stuttering persists into adulthood or if it is outgrown during childhood.
- Some individuals continue to stutter into adulthood, while others naturally recover or see significant improvements.
7. Secondary Behaviors:
- Stuttering may also be classified based on the presence of secondary behaviors. These are physical or verbal reactions to stuttering, such as facial grimaces, eye blinking, or word substitutions, used to avoid stuttering.
- Stuttering with secondary behaviors can be more complex and challenging to treat.
8. Severity Levels:
- Stuttering can be classified by severity, ranging from mild to severe. Severity is often determined by the frequency and duration of disfluencies and their impact on communication.
It’s important to note that these classifications are not always mutually exclusive, and some individuals may exhibit characteristics of more than one type of stuttering. Additionally, the presentation and classification of stuttering can vary from person to person. Stuttering is a complex communication disorder, and assessment by a qualified speech-language pathologist is essential to determine the most appropriate treatment and management strategies for each individual.
Stuttering therapy
- Treatment for stuttering often involves a combination of therapeutic approaches tailored to the individual’s needs and goals. Here is a list of some of the standard therapeutic approaches used for the treatment of stuttering:
Speech Modification Techniques
- Fluency Shaping: This approach teaches individuals who stutter to speak more fluently by modifying their speech patterns. Techniques may include slowing speech rate, prolonging vowel sounds, and using gentle onsets (soft starts to words).
- Easy Onset: Encourages individuals to start words or sentences with gentle, easy starts instead of sudden or forceful starts, reducing tension and improving fluency.
Stuttering Modification Strategies:
- Cancellation: After a stuttering event, individuals pause, acknowledge the stutter, and repeat the word or phrase with reduced tension. Addressing and correcting the stutter improves fluency.
- Pull-Out: When stuttering occurs, individuals pause and smoothly transition out of the stutter. Corrects the stutter mid-speech for improved fluency.
- Preparation: Involves anticipating challenging words or situations and using techniques like stretching sounds or lightly tapping. Reduce stuttering by preparing for difficult speech moments.
Cognitive-Behavioral Therapy (CBT):
CBT aims to address the emotional and psychological aspects of stuttering, such as anxiety, fear, and negative self-perceptions. It helps individuals develop coping strategies and improve their self-esteem.
Desensitization and Confidence-Building:
Therapy may involve desensitization techniques, such as voluntarily stuttering or speaking in challenging situations to reduce anxiety and build confidence.
Group Therapy:
Group therapy provides a supportive environment for individuals who stutter to practice fluency techniques, share experiences, and gain social confidence.
Parent/Caregiver Training:
Parents and caregivers can learn strategies to create a supportive communication environment for their child who stutters, helping them communicate more comfortably.
Stress and Anxiety Management:
Stress and anxiety can exacerbate stuttering. Techniques such as relaxation exercises, mindfulness, and stress reduction strategies can be integrated into therapy to manage emotional triggers.
Neurofeedback and Biofeedback:
Neurofeedback or biofeedback is used to gain better control over physiological responses associated with stuttering, such as muscle tension or stress.
Electronic Devices and Apps:
Speech therapy apps and devices may provide visual or auditory feedback to assist individuals in monitoring and improving their speech patterns.
Supportive Counseling:
Some individuals find it helpful to engage in counseling to discuss the emotional and psychological aspects of living with stuttering, such as self-acceptance and managing societal pressures.
It’s important to note that stuttering therapy should be personalized to meet the unique needs of each individual. A qualified and experienced speech-language pathologist (SLP) or therapist specializing in stuttering can assess the specific challenges faced by the person who stutters and develop a tailored treatment plan. Early intervention is crucial in helping children who stutter, but therapy can also benefit teenagers and adults. Therapy aims to improve speech fluency, communication confidence, and overall quality of life.
Biofeedback speech therapy for stuttering
Biofeedback speech therapy for stuttering is a therapeutic technique to help individuals gain better control over physiological processes, such as muscle tension and stress, that may contribute to stuttering. While biofeedback is not a standalone treatment for stuttering, it can be a valuable component of a comprehensive therapy program. Here’s how biofeedback can be used in the treatment of stuttering:
1. Muscle Tension Monitoring:
Electromyographic (EMG) biofeedback speech therapy for stuttering can monitor muscle tension, especially in the muscles associated with speech production (e.g., facial muscles and neck muscles).
Individuals who stutter can learn to recognize patterns of excessive muscle tension during speech, which can contribute to disfluencies. Biofeedback provides real-time information about muscle activity, helping them become more aware of tension and relaxation in these muscles.
2. Relaxation Training:
Biofeedback can assist in teaching individuals relaxation techniques to reduce muscle tension and stress.
By seeing or hearing their physiological responses on a biofeedback monitor (e.g., muscle activity or skin conductance), individuals can practice relaxation exercises and learn to control their bodily responses.
3. Stress Reduction:
Stress and anxiety can exacerbate stuttering. Biofeedback can help individuals learn to manage stress and anxiety levels by providing feedback on physiological stress indicators, such as heart rate variability or skin temperature.
Individuals can develop strategies to reduce stress and anxiety during speaking situations with biofeedback.
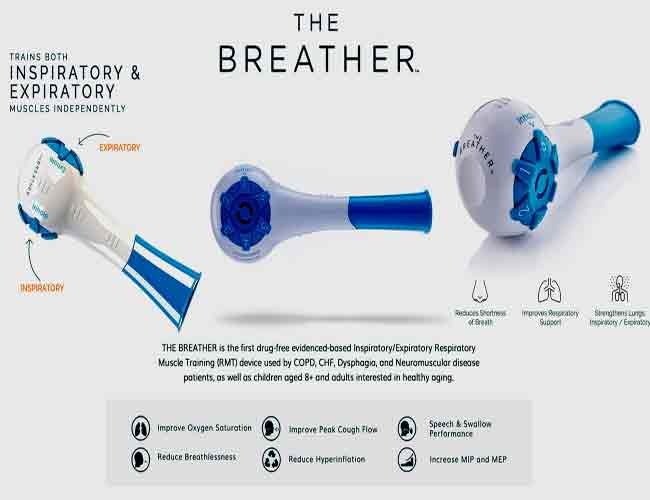
4. Control of Breathing:
Breathing patterns play a significant role in speech production and fluency. Respiratory biofeedback speech therapy for stuttering can monitor and adjust breathing patterns during speech.
Individuals can learn to control their breath and reduce breath-related disfluencies by providing feedback on respiratory rate and depth.
5. Generalization and Self-Regulation:
The skills learned through biofeedback training can be applied in real-life speaking situations. Individuals can use the self-regulation techniques acquired during biofeedback therapy to improve their speech fluency.
6. Progress Monitoring:
Biofeedback sessions can track and record progress over time, allowing individuals and therapists to assess the effectiveness of relaxation and self-regulation strategies.
It’s important to note that biofeedback is typically used with other evidence-based stuttering therapy approaches, such as speech modification techniques, stuttering modification strategies, and cognitive-behavioral therapy. A qualified speech-language pathologist or therapist specializing in stuttering therapy can integrate biofeedback into an individualized treatment plan based on the specific needs and goals of the person who stutters.
The effectiveness of biofeedback in stuttering treatment can vary from person to person, and the choice to use biofeedback should be made in consultation with a qualified therapist. When integrated appropriately, biofeedback can help individuals become more aware of and better control the physiological factors contributing to stuttering, ultimately improving speech fluency and communication confidence.
What modalities of biofeedback speech therapy for stuttering can be used for effective treatment?
Several modalities of biofeedback can be utilized for stuttering treatment to assist individuals in gaining better control over physiological processes that may contribute to disfluency. Specifically, these modalities provide real-time feedback on specific physiological indicators, which allows individuals to monitor and adjust their responses. For example, here are some of the biofeedback modalities that can be employed in stuttering treatment:
1. Electromyographic (EMG) Biofeedback speech therapy for stuttering:
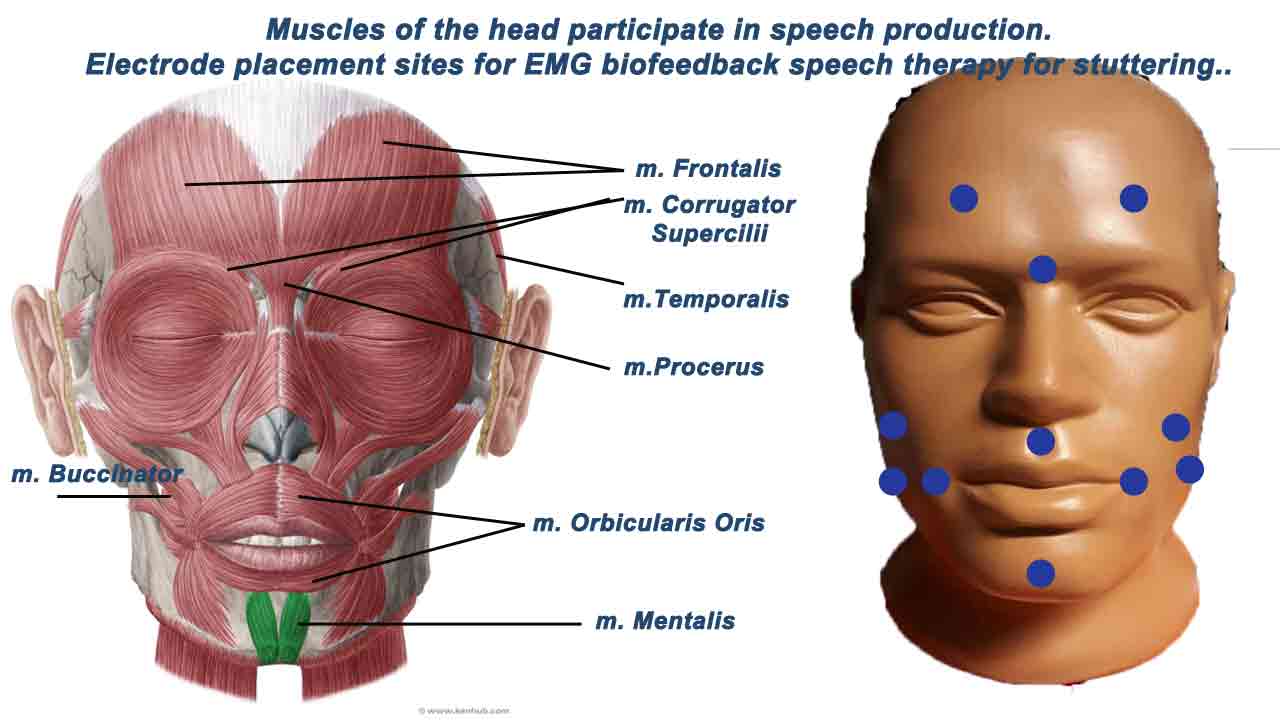
- EMG biofeedback measures muscle activity and tension by using electrodes placed on the skin’s surface or inside the mouth to monitor the activity of speech-related muscles.
- For stuttering treatment, EMG biofeedback can help individuals become aware of excessive tension in muscles involved in speech production (e.g., facial and neck muscles).
- By visualizing muscle activity in real-time, individuals can learn to relax these muscles during speech to reduce tension-related disfluencies.
2. Respiratory Biofeedback:
- Respiratory biofeedback focuses on monitoring and controlling breathing patterns closely related to speech fluency.
- To reduce breath-related disfluencies, individuals can use respiratory biofeedback to adjust their breathing rate, depth, and coordination during speech.
3. Heart Rate Variability (HRV) Biofeedback:
- HRV biofeedback measures the variation in time between successive heartbeats, which reflects the body’s physiological response to stress and relaxation.
- It can help individuals learn to manage stress and anxiety levels, which can impact stuttering.
- By increasing heart rate variability, individuals can promote relaxation and reduce the physiological stress response during speaking situations.
4. Skin Conductance Biofeedback:
- Skin conductance biofeedback monitors the electrical conductance of the skin, which can indicate changes in emotional arousal and stress levels.
- Individuals can use skin conductance biofeedback to become aware of stress reactions and learn relaxation techniques to reduce stress-related disfluencies.
5. Temperature Biofeedback:
- Temperature biofeedback measures changes in skin temperature, which emotional and stress responses can influence.
- It can help individuals learn to regulate their body’s temperature and reduce the physiological effects of stress on speech.
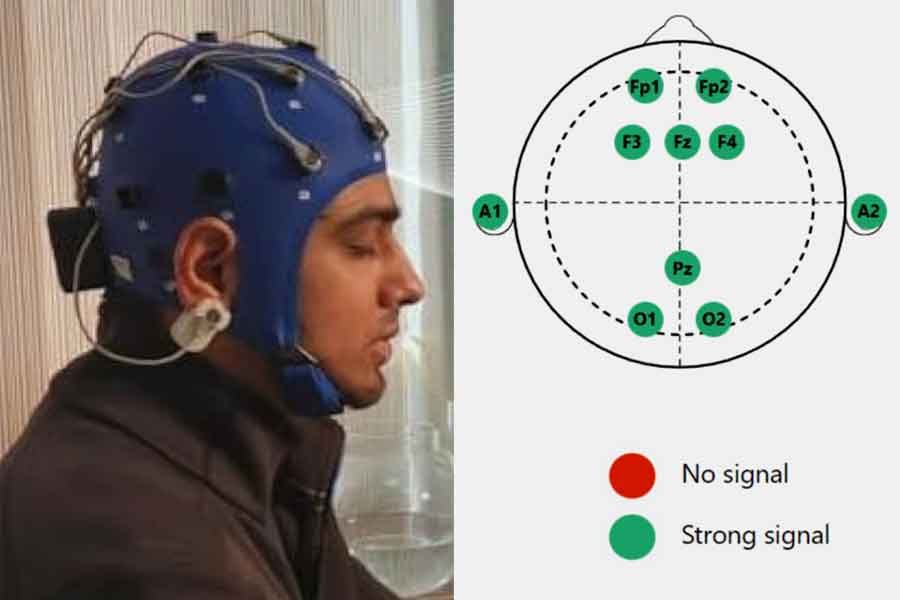
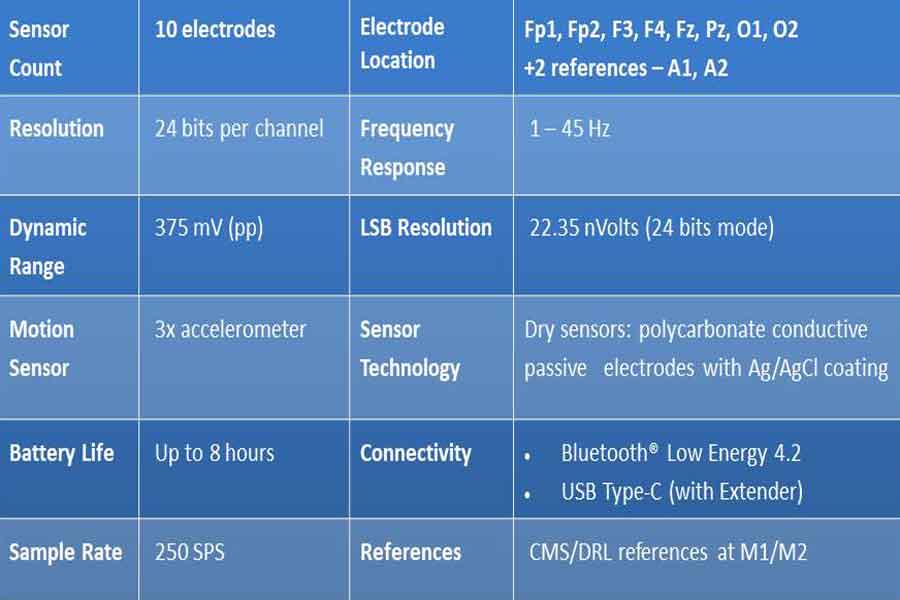
6. Neurofeedback or Brainwave (EEG) Biofeedback speech therapy for stuttering:
EEG biofeedback, or neurofeedback, monitors brainwave activity and provides feedback on brainwave patterns to help individuals regulate brain activity associated with speech production and anxiety.
7. Biofeedback Apps and Software:
- Various biofeedback apps and software programs are available for smartphones and computers.
- These apps may provide visual or auditory feedback on physiological indicators and can be used for self-regulation and practice outside therapy sessions.
The choice of biofeedback modality depends on the specific needs and goals of the individual who stutters. Therefore, it should be determined in collaboration with a qualified speech-language pathologist or therapist who specializes in stuttering therapy. In addition, biofeedback is often integrated into a comprehensive stuttering therapy program. Furthermore, it is combined with other evidence-based therapeutic approaches to help individuals improve speech fluency and enhance communication confidence.
Role of EMG biofeedback in the treatment of stuttering
EMG (Electromyography) biofeedback is a therapeutic technique that can be used as a component of the treatment of stuttering. Its primary role is to assist individuals who stutter in gaining greater awareness and control over the muscle tension and coordination involved in speech production. Here’s how EMG biofeedback can be beneficial in the treatment of stuttering:
Benefits of EMG Biofeedback in Stuttering Treatment
1. Muscle Tension Awareness: EMG biofeedback provides real-time feedback on the activity of specific muscles involved in speech production, such as the muscles around the mouth, lips, jaw, and throat. By monitoring muscle activity, individuals who stutter can become more aware of patterns of excessive tension and learn to recognize when they are tensing these muscles unnecessarily.
2. Tension Reduction: The visual or auditory feedback provided by EMG biofeedback can help individuals reduce excessive muscle tension during speech. When they see or hear that they are tensing their speech muscles, they can work to relax and release that tension, which can lead to smoother and more fluent speech.
3. Muscle Coordination: Stuttering often involves disruptions in the coordination of speech muscles. EMG biofeedback can help improve muscle coordination by assisting individuals to learn to activate and deactivate the relevant muscles correctly during speech.
4. Biofeedback-Based Practice: EMG biofeedback allows individuals to practice speech with immediate feedback in a controlled environment. This practice can help them develop new, more fluent speech patterns while reducing tension-related behaviors.
Additional Considerations for EMG Biofeedback
5. Self-Regulation: Individuals can learn to self-regulate their muscle tension and speech patterns over time without needing continuous biofeedback. They can carry the skills and awareness gained from biofeedback sessions into everyday communication.
6. Individualized Therapy: EMG biofeedback can be tailored to the specific needs of each stutterer. Therapists can target specific muscle groups and patterns of tension unique to the individual’s speech difficulties.
It’s important to note that EMG biofeedback is often used as part of a comprehensive stuttering therapy program, which may include other therapeutic approaches such as speech modification techniques, stuttering modification strategies, and cognitive-behavioral therapy. The choice of therapy approaches, including EMG biofeedback, will depend on the individual’s specific needs and goals for improving their fluency and reducing stuttering.
As with any therapeutic intervention, the effectiveness of EMG biofeedback in stuttering treatment can vary from person to person. Therefore, it should be administered and supervised by a qualified speech-language pathologist or therapist specializing in stuttering therapy and can tailor the treatment plan to the individual’s unique needs.
EMG electrode placement sites for biofeedback for stuttering
Electromyography (EMG) biofeedback involves placing electrodes on specific muscle groups associated with speech production and providing visual or auditory feedback to the individual about the activity of these muscles. This feedback can assist in reducing tension and improving muscle coordination during speech. Here are some common electrode placement sites for EMG biofeedback in stuttering therapy:
Head Muscles:
1. Orbicularis Oris Muscle: The orbicularis oris muscle is a circular muscle that surrounds the mouth and plays a significant role in speech production. This muscle controls lip movements during speech, and excessive tension in this muscle can lead to difficulties in articulation and fluency. EMG electrodes can be placed on the corners of the mouth or along the upper and lower lips to monitor muscle activity. This can help individuals become aware of excessive muscle tension and facilitate relaxation.
2. Mentalis Muscle: The mentalis muscle is located in the chin area and can be involved in the lower lip and chin movements during speech. Excessive tension in this muscle can lead to difficulties in articulation and fluency. Electrodes can be placed on the chin to monitor this muscle’s activity and help individuals reduce unnecessary tension.
3. Frontalis Muscle: The frontalis muscle is located in the forehead and involves facial expressions. Although not directly related to speech, it can be monitored to assess overall muscle tension and relaxation.
4. Facial Muscles: Various facial muscles, including the frontalis (forehead) and corrugator supercilii (between the eyebrows), can become tense during stuttering moments, contributing to facial tension that may impact speech.
5. Buccinator Muscle: This muscle is located in the cheeks and controls the oral cavity during speech. Tension in the buccinator muscle can influence articulation.
6. Temporalis Muscle: This muscle is located on the side of the head. It can influence jaw movement and tension.
7. Masseter Muscle: The masseter muscle is part of the jaw muscles and can contribute to jaw tension during speech.
8. Palatal Muscles: These are muscles of the soft palate (velum), such as the palatoglossus and palatopharyngeus, which affect resonance and articulation.
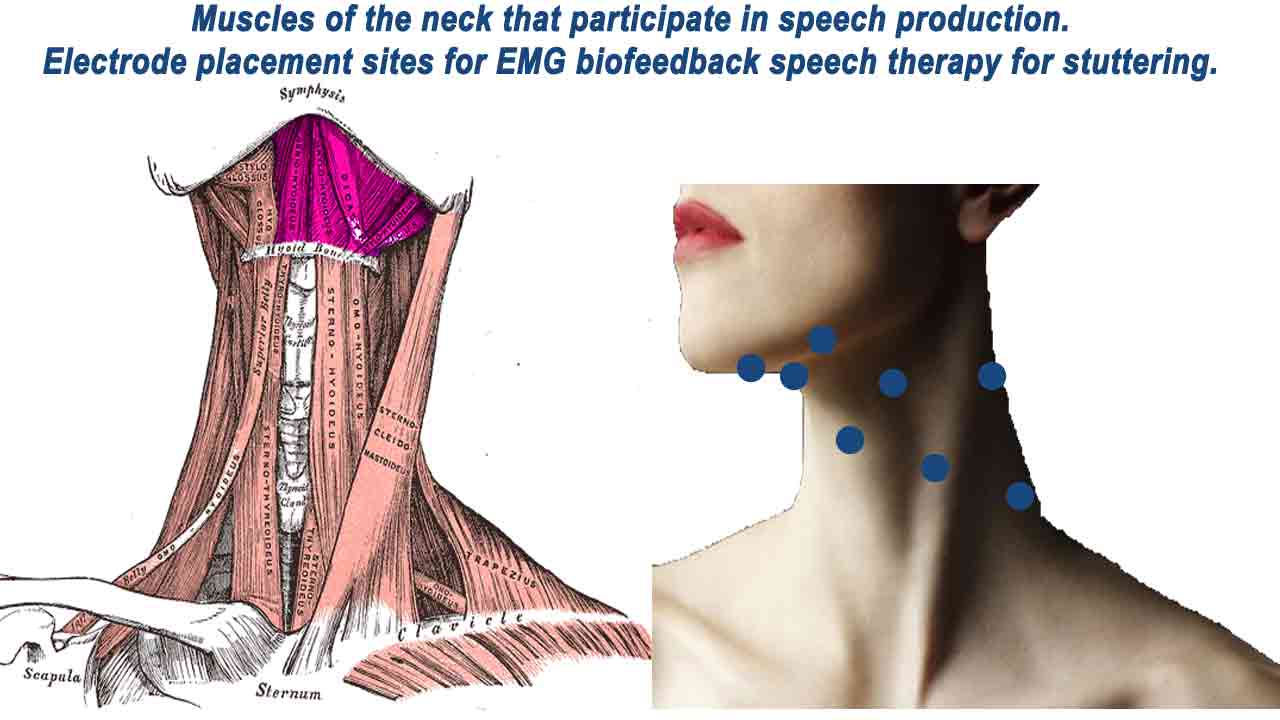
Neck muscles
Upper Neck Muscles
1. Suprahyoid Muscles: The suprahyoid muscles include the digastric and mylohyoid, which play a role in laryngeal control and swallowing. The suprahyoid muscles are located under the chin and beneath the jaw and are involved in jaw and tongue movement during speech, laryngeal control, and swallowing. Tension in these muscles can affect vocal control and fluency.
Electrodes may be placed along the neck or jawline to monitor the activity of these muscles.
2. Infrahyoid Muscles: The infrahyoid muscles (sternohyoid and omohyoid) are under the chin, below the suprahyoid muscles. They can influence laryngeal control and voice production and are also involved in speech-related movements. Monitoring and training these muscles can help reduce tension-related disfluencies.
Electrodes can be placed in the neck area to monitor these muscles.
3. Platysma Muscle: The platysma muscle is a thin sheet covering the front of the neck. It can contribute to neck tension during speech. Electrodes may be placed along the neck to monitor platysma muscle activity.
Lower Neck and Upper Back Muscles
4. Trapezius Muscle: The trapezius muscle is a large muscle that extends down the neck and upper back. Specifically, the upper portion of the trapezius muscle in the neck and upper back can become tense during stuttering. It may contribute to neck and shoulder tension, affecting overall speech tension.
5. Sternocleidomastoid (SCM) Muscle: The sternocleidomastoid muscle runs from the base of the skull to the collarbone and sternum. Tension in the SCM can affect head and neck posture and potentially contribute to speech tension.
6. Scalene Muscles: The scalene muscles are located on the sides of the neck and play a role in neck movement and respiration. Tension in the scalenes can affect overall neck tension and posture during speech.
7. Longus Colli Muscle: This muscle is situated in the anterior (front) of the neck and contributes to neck flexion and head movement. Monitoring and training this muscle can help reduce tension in the front of the neck.
These muscles collectively contribute to the coordination, tension, and control involved in speech production. Monitoring and training them with EMG biofeedback can assist individuals who stutter in becoming more aware of and regulating muscle activity to improve speech fluency and reduce disfluencies.
The electrode placements may vary based on the individual’s unique speech patterns and muscle tension. EMG biofeedback aims to help individuals become more aware of muscle tension patterns and learn to control and reduce tension during speech, ultimately improving fluency.
Role of Breathing Biofeedback in Stuttering Treatment
Breathing biofeedback can be a helpful component of stuttering therapy by assisting individuals in developing better control over their breathing patterns during speech. Proper breathing techniques can contribute to improved speech fluency and reduced stuttering. Here’s the role of breathing biofeedback in the treatment of stuttering and how it can be performed:
1. Increased Awareness: Breathing biofeedback helps individuals become more aware of their breathing patterns, such as shallow or irregular breathing, which can contribute to stuttering.
2. Controlled Breathing: It teaches individuals how to control their breath, allowing for more relaxed and controlled speech production.
3. Reduction of Tension: Proper breathing techniques can help reduce overall muscle tension, including tension in the speech muscles, enhancing speech fluency.
4. Anxiety Management: Breath control techniques can also be beneficial for managing anxiety, which can exacerbate stuttering. Deep, slow breaths can promote relaxation and reduce anxiety-related tension.
Performing Breathing Biofeedback for Stuttering
Here are the general steps for Breathing biofeedback:
1. Assessment: The therapist will first assess the individual’s current breathing patterns and their impact on speech fluency. This may involve monitoring chest, diaphragmatic, or abdominal breathing and the rate and depth of breaths.
2. Sensor Placement: Small sensors or electrodes may be attached to the individual’s chest, abdomen, or other relevant areas to monitor breathing patterns. These sensors are connected to a biofeedback device.
3. Feedback Display: The biofeedback device provides real-time visual or auditory feedback based on the individual’s breathing patterns. This feedback can be displayed on a computer screen or through audio cues.
4. Training: The therapist will guide the individual through exercises and techniques to improve their breathing patterns. This may include exercises to promote diaphragmatic breathing (deep belly breathing) and control breath rate and rhythm.
5. Practice: The individual practices these techniques while receiving feedback from the biofeedback device. They learn to adjust their breathing to achieve smoother and more controlled speech.
6. Generalization: Over time, the goal is for the individual to apply these breathing techniques in everyday communication, not just during therapy sessions. The therapist helps the individual transfer these skills to real-life situations.
7. Progress Monitoring: Progress is monitored throughout therapy to track improvements in breathing patterns and speech fluency. Adjustments to the treatment plan can be made as needed.
The effectiveness of Breathing biofeedback speech therapy for stuttering can vary from person to person, and it is essential to work with a qualified speech-language pathologist or therapist who can tailor the treatment to the individual’s specific needs and goals.
Role of Heart Rate Variability biofeedback speech therapy for stuttering
Heart Rate Variability (HRV) biofeedback is a therapeutic technique for treating stuttering, particularly for managing stress and anxiety, which are known to exacerbate stuttering. HRV biofeedback focuses on regulating the variation in time between successive heartbeats, which reflects the body’s physiological response to stress and relaxation.
Here’s the role of HRV biofeedback in stuttering treatment and how it works:
1. Stress Reduction: Stuttering often occurs or worsens in stressful situations. HRV biofeedback helps individuals learn to manage stress by providing real-time feedback on their physiological responses, such as heart rate variability. By increasing HRV, individuals can promote relaxation and reduce the physiological stress response during speaking situations.
2. Anxiety Management: Anxiety is a common trigger for stuttering. HRV biofeedback can teach individuals to regulate their anxiety levels by monitoring changes in heart rate variability. As they become more skilled in HRV control, they can apply these techniques to reduce anxiety associated with speaking.
3. Emotional Regulation: Stuttering can lead to negative emotions, which can exacerbate speech difficulties. HRV biofeedback can help individuals better control their emotional responses by promoting emotional regulation and resilience.
4. Improved Self-Regulation: HRV biofeedback enhances an individual’s self-regulating physiological responses. This can be especially valuable during stuttering moments, as individuals can learn to stay calm and composed, reducing the likelihood of disfluencies caused by increased tension.
How HRV Biofeedback Works
1. Sensor Placement: HRV biofeedback typically involves placing sensors on the individual’s skin, often on the chest or wrists, to monitor heart rate variability.
2. Data Collection: The sensors continuously collect data on the time intervals between heartbeats (R-R intervals) representing HRV.
3. Real-Time Feedback: The collected data are processed and displayed in real-time on a computer screen or through a mobile app. Individuals can see graphical representations of their HRV.
4. Breathing Techniques: HRV biofeedback often incorporates specific breathing techniques, such as slow, deep diaphragmatic breathing. The individual is guided to synchronize their breathing with the displayed HRV pattern.
5. Feedback and Practice: As individuals practice controlled breathing and see changes in their HRV patterns, they learn to associate specific breathing techniques with increased HRV and reduced stress. This reinforces relaxation and stress reduction skills.
6. Progress Monitoring: Individuals can monitor their progress in increasing HRV and reducing stress and anxiety levels over time. They may see improvements in their ability to remain calm during speaking situations and experience fewer stuttering incidents.
7. Generalization: The self-regulation skills learned through HRV biofeedback can be applied in real-life speaking situations, helping individuals manage stress and anxiety while communicating.
HRV biofeedback, when integrated into a comprehensive stuttering therapy program, can be a valuable tool for individuals seeking to reduce the impact of stress and anxiety on their speech fluency. It empowers them with the skills to regulate their physiological responses better, ultimately contributing to improved speech confidence and fluency.
Role of acoustic biofeedback in stuttering treatment
Acoustic biofeedback is a therapeutic tool used in stuttering treatment to help individuals manage their speech patterns and improve fluency. Specifically, it provides real-time auditory feedback on different aspects of speech. As a result, individuals can monitor and adjust their speech production more effectively. Here’s how acoustic biofeedback plays a role in stuttering treatment:
Introduction to Acoustic Biofeedback in Stuttering Treatment
1. Awareness of Stuttering Patterns: Acoustic biofeedback helps individuals who stutter to become more aware of their patterns, including the frequency and severity of disfluencies (stuttering moments). By hearing their speech in real time, individuals can identify specific problem areas and patterns.
2. Monitoring Speech Rate: Acoustic biofeedback can provide feedback on speech rate or speak too quickly, contributing to stuttering. Individuals can learn to adjust their speaking rate to a more comfortable and controlled pace.
3. Smoothness and Fluency: Acoustic biofeedback can highlight moments of speech tension or disruptions in the flow of speech. By listening to their speech in real time, individuals can work on producing smoother, more fluent speech patterns.
4. Pitch and Volume Control: Some acoustic biofeedback systems can provide feedback on pitch and volume variations in speech. This can help individuals achieve consistent pitch and volume levels, contributing to fluency.
Advanced Applications and Benefits of Acoustic Biofeedback
5. Delay or Altered Auditory Feedback: In some cases, acoustic biofeedback systems introduce a slight delay or alter the pitch of the individual’s voice. These alterations can create a “choral” effect, which may reduce stuttering and improve fluency for some individuals.
6. Practice and Self-Regulation: Acoustic biofeedback allows individuals to practice speech techniques and strategies while receiving immediate feedback. With guidance from a speech-language pathologist, they can develop self-regulation skills to adjust their speech in real time.
7. Transfer to Everyday Communication: Acoustic biofeedback therapy aims to help individuals generalize the skills learned in therapy sessions to their everyday communication. They can apply the techniques and strategies to reduce stuttering and improve fluency in real-world situations.
8. Progress Tracking: Acoustic biofeedback sessions can track and record progress. This data can be used to evaluate the effectiveness of therapy and adjust the treatment plan as needed.
The choice of therapy approaches and the inclusion of acoustic biofeedback will depend on the individual’s specific needs and goals for improving their fluency and reducing stuttering.
As with any therapeutic intervention, the effectiveness of acoustic biofeedback in stuttering treatment can vary from person to person. Therefore, it should be administered and supervised by a qualified speech-language pathologist or therapist specializing in stuttering therapy who can tailor the treatment plan to the individual’s needs.
How to perform acoustic biofeedback for stuttering
Performing acoustic biofeedback for stuttering typically involves using specialized equipment and software under the supervision of a qualified speech-language pathologist or therapist specializing in stuttering therapy.
Here’s a general overview of how acoustic biofeedback for stuttering can be performed:
Initial Steps and Setup for Acoustic Biofeedback Therapy
1. Assessment and Evaluation:
- Before starting acoustic biofeedback therapy, the speech-language pathologist (SLP) will conduct a comprehensive assessment to evaluate the individual’s stuttering patterns, speech characteristics, and specific needs.
- The SLP will determine which aspects of speech (e.g., speech rate, fluency, pitch, volume) would benefit from acoustic biofeedback.
2. Selecting and Setting Up Equipment:
- The SLP will choose appropriate acoustic biofeedback equipment and software based on the individual’s therapy goals and needs. This may include software designed for speech therapy that provides real-time auditory feedback.
- The equipment typically includes a microphone to capture the individual’s speech and speakers or headphones to deliver the auditory feedback.
3. Baseline Recording:
- The initial session may involve recording the individual’s baseline speech patterns without biofeedback. This helps establish a starting point for therapy and provides a reference for progress.
Conducting Biofeedback Sessions and Progress Monitoring
4. Biofeedback Sessions:
- During biofeedback sessions, the individual will speak into the microphone while the system provides real-time auditory feedback.
- The feedback may focus on problematic aspects of speech, such as speaking rate, pitch, or fluency. For example, the system might provide auditory cues when the individual speaks too quickly or stutters.
- Based on the feedback provided, the individual will work with the SLP to develop strategies for adjusting their speech. This may involve practicing speaking at a more controlled rate, producing smoother speech, or adjusting pitch and volume.
- The individual and SLP will review and discuss the feedback during the session, identifying areas for improvement and setting goals for future sessions.
5. Practice and Generalization:
- The individual will practice the techniques learned in biofeedback sessions and attempt to generalize them to real-world communication situations.
- The SLP will work with the individual to apply the strategies learned in therapy to everyday speaking scenarios, such as conversations with family and friends and in various social contexts.
6. Progress Tracking and Adjustments:
- Progress will be monitored and tracked throughout therapy using data collected during biofeedback sessions.
- The SLP will make adjustments to the treatment plan based on the individual’s progress, changing therapy goals as needed.
7. Termination and Maintenance:
- Therapy may continue until the individual achieves their therapy goals or experiences significant improvement in fluency and stuttering management.
- After therapy is completed, individuals may benefit from periodic follow-up sessions to maintain their progress and address any challenges.
The SLP will tailor the treatment plan to the individual’s unique needs and provide guidance and support throughout therapy. Acoustic biofeedback is just one component of a comprehensive stuttering therapy program that may include other therapeutic approaches and techniques.
Use of the Forbrain audio-vocal biofeedback device in the treatment of stuttering
The Forbrain audio-vocal biofeedback device was marketed as a tool that combines bone conduction and auditory feedback to help individuals improve their speech and communication skills. It was primarily designed to assist with various speech and language challenges, including stuttering. Here’s how the Forbrain device is typically used and its potential role in the treatment of stuttering:
1. Auditory Feedback: The Forbrain device includes a microphone and bone conduction technology that delivers auditory feedback directly to the wearer’s ears. It enhances the perception of their voice as they speak.
2. Voice Enhancement: Forbrain is designed to provide more precise and resonant auditory feedback, which can help individuals become more aware of their speech patterns, including any stuttering or disfluencies.
3. Speech Practice: Users can practice speaking while wearing the device, which provides real-time auditory feedback, allowing individuals to monitor their speech.
4. Attention and Focus: Forbrain also aims to help users improve their attention and concentration. Wearing the device during speech practice may help individuals become more focused on their speech, which can indirectly help reduce stuttering.
5. Neurological Training: Forbrain may promote neuroplasticity, potentially leading to improved speech fluency and reduced stuttering.
Forbrain improves self-awareness, which makes speech easier to correct. It also helps correct the processing of sensory and auditory information and improves listening skills.
Role of neurofeedback in the treatment of stuttering. How to perform?
Brain Regions and Electrodes for Speech Neurofeedback
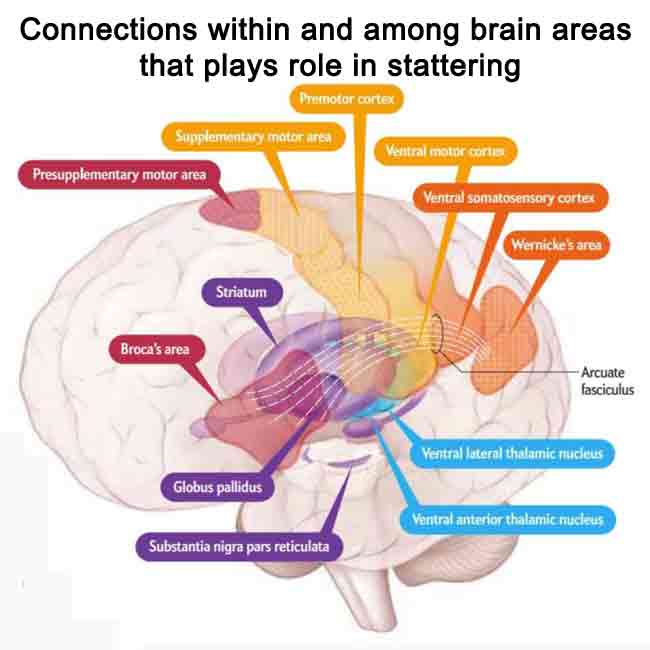
Stuttering has been linked to weakness in the fibers that carry nerve impulses among three regions: the thalamus, which relays sensory signals; the basal ganglia, which coordinates movements; and the cerebral cortex, which is involved in cognition and integration of sensory and motor signals.
There are many connections within and among these brain areas. A key fiber link in the cortex is the arcuate fasciculus, which shows deficiencies in people who stutter. Other potentially poor connections are within the basal ganglia and the network linking all areas, such as the cortico-basal ganglia-thalamocortical loop.
1. Brain Regions Linked to Stuttering
Stuttering has been linked to weaknesses in the neural connections among three key brain regions:
- Thalamus: Relays sensory signals.
- Basal Ganglia: Coordinates movements.
- Cerebral Cortex: Involved in cognition and integration of sensory and motor signals.
2. Key Fiber Links and Deficiencies
Important connections include:
Arcuate Fasciculus: A key fiber link in the cortex that shows deficiencies in individuals who stutter.
Cortico-Basal Ganglia-Thalamocortical Loop: A network linking all areas may exhibit poor connections in stuttering.
Electrode Placement Using the International 10-20 System
The International 10-20 System is a standardized method for electrode placement used in electroencephalography (EEG) to locate specific areas of the scalp relative to underlying brain regions. While the primary focus of the 10-20 system is on general brain activity monitoring, it can be adapted for speech neurofeedback by targeting areas of the brain associated with language and speech processing. Here are some electrode placement sites based on the 10-20 System that can be relevant for speech neurofeedback:
1. Frontal Electrodes:
F7 and F8: These electrodes are located over the left and right frontal lobes. They may be relevant for speech neurofeedback as the frontal lobes involve various aspects of language production and executive functions.
2. Temporal Electrodes:
T3 and T4: These electrodes are positioned over the left and right temporal lobes, which are crucial for language comprehension, auditory processing, and speech.
3. Central Electrodes:
C3 and C4: These electrodes are situated over the central region of the scalp and may be relevant for speech neurofeedback as they are associated with motor functions, including motor control of speech.
4. Parietal Electrodes:
P3 and P4: These electrodes are located over the left and right parietal lobes, which are involved in various aspects of language processing and sensory integration.
5. Frontocentral Electrodes:
FC5 and FC6: Positioned between the frontal and central regions, these electrodes may capture neural activity related to speech planning and execution.
Specific Electrode Areas for Speech Fluency
6. Supplementary Motor Area (SMA):
FCz: Located at the midline of the scalp, FCz is associated with motor planning and may be relevant for speech motor control.
7. Broca’s Area (Left Hemisphere):
F5 and F3: These electrodes are located over the left frontal region and may particularly interest speech neurofeedback, as Broca’s area is essential for language production and speech fluency.
8. Wernicke’s Area (Left Hemisphere):
T5: Positioned over the left temporal lobe, T5 may be associated with language comprehension and processing.
9. Angular Gyrus (Left Hemisphere):
P5: Over the left parietal lobe, P5 may play a role in language processing and comprehension.
Neurofeedback for Stuttering Management
Neurofeedback can be effective in rewiring the brain in the specific brain area responsible for speech fluency and by regulating the conditions concomitant to stuttering.
1. Stress and Anxiety Management: Stress and anxiety can often exacerbate stuttering. Neurofeedback may help individuals learn to regulate their stress response and reduce anxiety levels, indirectly contributing to improved fluency by reducing tension associated with stuttering.
2. Attention and Concentration: Neurofeedback can be used to train individuals to enhance their attention and concentration abilities. Improved attention control may help individuals who stutter maintain focus on their speech and reduce the likelihood of stuttering interruptions.
3. Relaxation and Self-Regulation: Neurofeedback can teach individuals self-regulation skills, which may be beneficial for managing emotional responses and muscle tension during speech production.
It’s important to note that the choice of electrode placement should be guided by the specific objectives of the speech neurofeedback therapy and the individual’s unique needs. Electrode positions can be adjusted to target brain regions associated with speech production, language comprehension, and fluency. Additionally, a qualified clinician or therapist with expertise in neurofeedback for speech and language disorders should be consulted to determine the most appropriate electrode montage for achieving therapeutic goals.
The electronic devices that can be used for treatment of stuttering
Several electronic devices and technologies can be used to assist in the treatment and management of stuttering. These devices often use traditional speech therapy techniques to provide real-time feedback and enhance therapy outcomes. Here is a list of some electronic devices and their descriptions:
Wearable and Tactile Devices
1. SpeechEasy Device:
- SpeechEasy is a wearable electronic device that resembles a hearing aid. It uses delayed auditory feedback (DAF) or altered auditory feedback (AAF) to provide real-time auditory feedback to stuttering individuals.
- How It Works: When the person speaks, their voice is slightly delayed or altered in pitch, which can reduce the frequency and severity of stuttering.
2. VibroTactile Feedback Devices:
- These devices provide tactile (vibratory) feedback to help individuals monitor and control their speech rate and fluency.
- How They Work: VibroTactile feedback devices can be worn as wristbands or placed on the skin. They vibrate in response to specific speech patterns, providing a tactile cue to slow down or ease tension.
3. FluencyMaster Device:
- FluencyMaster is a handheld electronic device designed to assist individuals in practicing fluency-enhancing techniques.
- How It Works: The device generates a metronome-like beat with which individuals can synchronize their speech to achieve a more controlled and fluent speech pattern.
Digital and Biofeedback Tools
4. Apps and Software:
- Various smartphone and computer apps are available to support individuals in practicing speech techniques and monitoring their progress.
- Some apps provide visual or auditory feedback, such as fluency charts or metronome-like cues, to assist with speech modification and fluency shaping.
5. Voice Analysis Software:
- Specialized voice analysis software can analyze speech patterns and provide visual feedback on pitch, intensity, and speech rate.
- This software can help individuals and therapists track progress and identify areas for improvement.
6. Biofeedback Devices:
- Biofeedback devices can monitor physiological indicators of stress and tension, which can be associated with stuttering.
- They may include sensors for measuring muscle tension, heart rate variability, or skin conductance. The data can help individuals learn to manage stress during speech.
7. Mobile Communication Devices:
- Mobile devices such as smartphones and tablets offer various apps and tools to aid individuals in communication, including text-to-speech apps, speech synthesis software, and augmentative and alternative communication (AAC) apps.
It’s important to note that the effectiveness of electronic devices in stuttering treatment can vary from person to person. These devices are often used as adjuncts to traditional speech therapy techniques, and selecting a specific device should be based on an individual’s needs, goals, and preferences. A qualified speech-language pathologist or therapist specializing in stuttering therapy can help assess whether and how these devices may be beneficial and guide their use.
Conclusion
Biofeedback Speech Therapy for Stuttering represents a promising and innovative approach to stuttering treatment. This therapeutic method harnesses the power of real-time physiological feedback to empower individuals who stutter with tools for enhanced fluency and communication confidence. Through the precise monitoring and training of muscles, breathing patterns, and even neural activity, biofeedback speech therapy offers a holistic approach to address the multifaceted challenges associated with stuttering.
By delving into biofeedback speech therapy’s principles, techniques, and potential benefits for stuttering, we have uncovered a dynamic strategy that goes beyond traditional interventions. It equips individuals to gain better control over muscle tension, reduce stress and anxiety, and even modulate neural patterns related to speech production.
Biofeedback speech therapy for stuttering is a testament to the evolution of speech therapy practices, driven by a commitment to improving the lives of those affected by stuttering. This innovative approach reflects the interdisciplinary nature of stuttering therapy, drawing on insights from psychology, physiology, and neurology to provide a comprehensive toolkit for clinicians and individuals alike.
As we look ahead, the continued research and application of biofeedback techniques in stuttering therapy promise even more personalized and effective treatments. Tailoring therapy plans to each individual’s unique needs, addressing their specific muscle tension patterns, emotional triggers, and neural responses, is a significant advancement in the field.
Biofeedback Speech Therapy for Stuttering reminds us that innovation, coupled with a deep understanding of the challenges faced by individuals who stutter, can lead to transformative results. As clinicians and researchers continue to explore the potential of biofeedback in stuttering therapy, we can anticipate brighter prospects for those seeking to unlock the fluent and confident communicators within themselves.



















Add a Comment