Biofeedback Article Category
Our Biofeedback Article Category unlocks the power of your mind-body connection. First, we show you how biofeedback works. Then, we explain why this practice matters. Ultimately, you will learn to use measurable signals for greater self-control.
Discover how biofeedback manages specific conditions. For example, it helps reduce stress and chronic pain. Similarly, it can improve sleep and lower blood pressure. Each article breaks down the science. Therefore, you see exactly how to train your body’s responses.
Next, we compare different biofeedback methods. For instance, heart rate variability (HRV) builds resilience. Meanwhile, muscle feedback (EMG) releases tension. After that, we help you choose the right tools. Consequently, you can meet your personal health goals.
Furthermore, we provide safe, effective, practical tips. You will learn what to expect during a session. Also, you’ll be able to see how to track your progress. Finally, we show you how to adjust your training for the best results.
Follow our Biofeedback Article Category guides. As a result, you will gain direct command over your well-being. In short, you build more profound awareness and lasting balance.
FAQ: Biofeedback Article Category
Biofeedback is a mind-body technique that puts you in control. First, electronic sensors monitor your physiological functions—such as heart rate, muscle tension, and skin temperature—in real time. Next, you observe these unconscious signals on a screen. Then, you consciously influence them through guided mental exercises, breathing, and relaxation techniques. Ultimately, this process promotes self-regulation and directly improves your health.
The most common and researched types include:
- Heart Rate Variability (HRV) Biofeedback: Trains you to create a resilient, balanced heart rhythm linked to stress reduction and better nervous system function.
- Electromyography (EMG) Biofeedback: Measures muscle tension, commonly used for chronic pain, tension headaches, and injury rehabilitation.
- Breathing Biofeedback (Respiratory Feedback): Uses sensors to monitor your breathing rate and patterns. This training helps you develop slower, deeper, and more regular diaphragmatic breathing, which directly calms the nervous system and is foundational for many other biofeedback methods.
- Thermal (Temperature) Biofeedback: Monitors skin temperature, which decreases under stress, to help manage conditions like migraines and Raynaud’s disease.
- Electrodermal Activity (EDA) Biofeedback: Measures sweat gland activity, a direct indicator of sympathetic nervous system arousal and emotional response.
Absolutely. First, consumer-grade wearable devices and mobile apps now make home biofeedback training easily accessible. Therefore, for general stress management and wellness, home practice with guided protocols can be highly effective. However, for specific medical conditions, we recommend a more structured approach. Specifically, you should first consult a certified biofeedback practitioner to establish a solid foundation. Only then can you safely and effectively transition to a sustainable home routine.
Master Pulmonary Rehab Exercises at Home
Are you still struggling to breathe long after your COVID-19 infection has ended? You are not alone. The journey to reclaiming your breath and vitality begins with a powerful, proven solution: pulmonary rehab. This comprehensive guide is your roadmap to recovery, detailing essential pulmonary rehab exercises you can master. Discover how to effectively perform pulmonary…
COVID and Mental Health: A Full Guide
The COVID-19 pandemic has permanently linked the issues of COVID and mental health in our collective consciousness. Many are now grappling with the lingering effects of COVID 19 stress, a confusing battle with COVID and brain fog, and persistent feelings of COVID and anxiety. Understanding the profound impact of COVID 19 and mental health is…
Overwhelmed at Work? Find Balance
Feeling overwhelmed at work can leave you drained, anxious, and struggling to keep up with daily demands. When tasks pile up, deadlines loom, or emotional pressure mounts, it’s easy to spiral into overwhelming stress or even overwhelming depression. But there’s a way to break free: learning how to stop getting overwhelmed and how to stop…
Stop Overthinking: Retrain Your Brain
Do you constantly feel trapped in a cycle of racing thoughts and mental fatigue? Understanding what causes overthinking is the first step toward regaining control of your mind. Many people struggle daily without realizing that effective overthinking treatment exists. From stress and decision paralysis to sleepless nights, the consequences are real—but they are not inevitable.…
MS and Depression: What You Can Do
Living with multiple sclerosis (MS) is challenging enough, but when depression in MS adds another layer of struggle, it can feel overwhelming. Studies show that nearly 50% of people with MS experience depression at some point—a rate much higher than the general population. The connection between MS and depression isn’t just emotional; it’s neurological, with…
Fast MS Pain Relief Using Biofeedback
Living with MS pain relief challenges can be overwhelming, but integrating biofeedback for MS offers new hope. This guide explores Multiple sclerosis and pain management, diving into effective strategies for Multiple Sclerosis pain management and describing how MS and pain management can be enhanced through rewiring the brain and muscle control. With consistent training, MS…
Biofeedback for ADHD & ADD at Home
Struggling with attention, focus, or hyperactivity? You’re not alone. Millions of children and adults live with ADHD or ADD, and many are now turning to biofeedback therapy for ADHD as a safe, effective, and drug-free solution. In this guide, you’ll discover how biofeedback for ADHD and biofeedback for ADD can be used at home to…
Stop Bruxism and TMJ Pain Naturally
Are you struggling with persistent jaw pain, teeth grinding, or jaw tension? You’re not alone. Millions of people silently suffer from bruxism and TMJ disorders—often without even knowing the root cause. Whether you’re clenching your teeth at night or experiencing jaw discomfort during the day, understanding the connection between TMJ and bruxism is crucial for…
Fear Therapy: Cure Phobias Fast
Do you feel paralyzed by irrational fears or phobias that control your life? Fear therapy offers a revolutionary, science-backed solution that goes beyond temporary fixes—rewiring your brain’s fear response for lasting freedom. Unlike traditional approaches, modern fear therapy combines proven techniques like exposure therapy with cutting-edge biofeedback and neurofeedback, giving you real-time control over anxiety…
Therapy for Burnout: Prevent & Recharge
Burnout is more than just feeling tired or stressed — it’s a state of emotional, mental, and physical exhaustion caused by prolonged stress and overwork. In this guide, we explore therapy for burnout, offering practical solutions for both prevention and recovery. Understanding the right strategies can make a big difference if you’re already feeling overwhelmed…
Biofeedback for Tinnitus: Does it work?
Tinnitus is not just an annoying ringing or buzzing in the ears — for many people, it reflects deeper issues involving stress, brain activity, and nervous system imbalances. This is precisely where biofeedback for tinnitus becomes a valuable tool. Unlike conventional therapies, biofeedback for tinnitus focuses on helping individuals regain control over the body’s stress…
CBT for Tinnitus Explained
Tinnitus, characterized by the constant ringing or buzzing in the ears, can significantly affect one’s quality of life, leading to stress, anxiety, and sleep disturbances. While there is no cure for tinnitus, CBT for tinnitus has emerged as one of the most effective non-medical treatments for managing its emotional and psychological impact. Cognitive behavioral therapy…
CBT for Panic Attacks
Panic attacks can be overwhelming and disruptive, leaving individuals feeling helpless and out of control. Fortunately, Cognitive Behavioral Therapy for Panic Disorder is a proven, effective treatment that helps people break free from the cycle of fear and anxiety. By addressing negative thought patterns, gradually exposing individuals to their worries, and teaching coping strategies, CBT…
Total Sleep Management for Insomnia
Struggling with restless nights and constant fatigue? You’re not alone. Millions of people face sleep disturbances, but the good news is that total sleep management offers effective solutions. By combining sleep therapy, biofeedback for insomnia, and neurofeedback for sleep, you can regain control over your sleep patterns. Techniques such as breathing exercises for sleeplessness and…
Emotional Balance vs Emotional Imbalance
Achieving emotional balance is essential for overall well-being, yet many people struggle with emotional imbalance due to stress, lifestyle, and daily challenges. When emotions spiral out of control, they can negatively impact decision-making, relationships, and mental health. However, mastering self-management emotional intelligence allows individuals to regulate their emotional responses, build resilience, and maintain inner stability.…
Women’s Wellness Retreat At Home: Tricks
Women’s Wellness Retreat At Home: Tricks Transform your home into a women’s wellness retreat and experience relaxation, stress relief, and improved well-being. A women’s mental health retreat doesn’t have to involve expensive travel—you can create a peaceful and restorative space right at home. Many wellness retreats for women focus on mindfulness, relaxation, and self-care, and…
Best Biofeedback for Pain Relief
Biofeedback and pain management are gaining recognition as a highly effective natural approach to treating various types of pain. Unlike traditional pain relief methods that often rely on medication, biofeedback pain management empowers individuals to take control of their physiological responses, helping to reduce pain and improve overall well-being. By using biofeedback for pain management,…
Advanced Pain Management Techniques
Pain is a complex and universal experience that affects individuals in different ways. Understanding what is pain, its causes, and how it can be managed is essential for improving quality of life. While traditional treatments often focus on short-term solutions, advanced pain management offers innovative methods to address the underlying causes of discomfort. By exploring…
Therapy for Dyslexia-Innovative Approach
Dyslexia is a complex learning disorder that affects individuals’ ability to read, write, and process language effectively. While traditional methods like speech therapy have provided support for years, innovative approaches are now transforming how we approach therapy for dyslexia. Cutting-edge technologies like biofeedback and neurofeedback offer non-invasive solutions directly targeting the brain’s functioning to enhance…
Mental Performance Training: NeuroVizr
Maintaining mental clarity, focus, and emotional balance is more important in today’s fast-paced world. Mental performance training offers a cutting-edge approach to improving brain function, and the NeuroVIZR device takes this concept to the next level. NeuroVIZR stimulates brain activity, promotes neuroplasticity, and enhances cognitive flexibility by combining light and sound therapy with innovative blinking…
HRV Training. How to improve performance
In recent years, integrating HRV training (Heart Rate Variability) with biofeedback guidance has emerged as a promising avenue for enhancing performance across various domains. This approach offers individuals real-time insights and cues to optimize their HRV metrics and overall performance outcomes. HRV, the variation in the time interval between heartbeats, is a window into the…
Secret of Success & Role of Biofeedback
Unlocking the secret of success is a pursuit that captivates individuals across all walks of life. In this quest for excellence, biofeedback modalities serve as powerful tools. They offer valuable insights into the intricate interplay between mind and body. By harnessing the principles of biofeedback, individuals gain the ability to understand their physiological responses. Furthermore,…
Biofeedback Devices for Anxiety Overcome
Managing anxiety can feel overwhelming, but biofeedback devices for anxiety offer a science-backed solution to regain control. These innovative tools provide real-time feedback on physiological responses such as heart rate, skin temperature, and muscle tension, helping individuals identify and manage their stress triggers. By fostering relaxation and teaching self-regulation techniques, biofeedback devices empower users to…
Mini Stroke Recovery and Biofeedback
Mini strokes, also known as transient ischemic attacks (TIAs), are brief episodes of neurological dysfunction caused by a temporary interruption of blood flow to the brain. While they may not cause permanent damage themselves, TIAs are often warning signs of a potential future stroke. Therefore, understanding the process of mini stroke recovery is crucial for…
Biofeedback for Migraines. How to choose
In the realm of headache disorders, migraines stand as a formidable challenge, often disrupting the lives of millions with their debilitating intensity and frequency. Among the myriad therapeutic approaches, biofeedback for migraines has emerged as a promising avenue, gaining increasing recognition. This innovative technique harnesses the body’s inherent ability to regulate physiological processes, offering a…
Nomophobia treatment. Biofeedback.
In the digital era, the pervasive phenomenon of Nomophobia, or the fear of being without one’s mobile phone, has given rise to a pressing need for effective interventions. Among the innovative approaches, Nomophobia treatment through biofeedback emerges as a promising solution. Leveraging advanced technology, Biofeedback offers a tailored and dynamic method to address the escalating…
Biofeedback speech therapy for stuttering
Stuttering is an action-induced speech disorder with involuntary, audible, or silent repetitions or prolongations in the utterance of short speech elements (sounds, syllables) and words. Stuttering typically begins in childhood and may persist into adulthood. It can vary in severity, with some individuals experiencing only mild stuttering while others may have more pronounced difficulties speaking…
Pelvic Floor Biofeedback for Urinary incontinence
Urinary incontinence (UI), a prevalent condition affecting individuals across various age groups, can profoundly impact one’s quality of life. The involuntary loss of bladder control can lead to not only physical discomfort but also emotional and social challenges. In pursuing innovative and effective solutions, medical research and treatment has turned its attention to the promising…
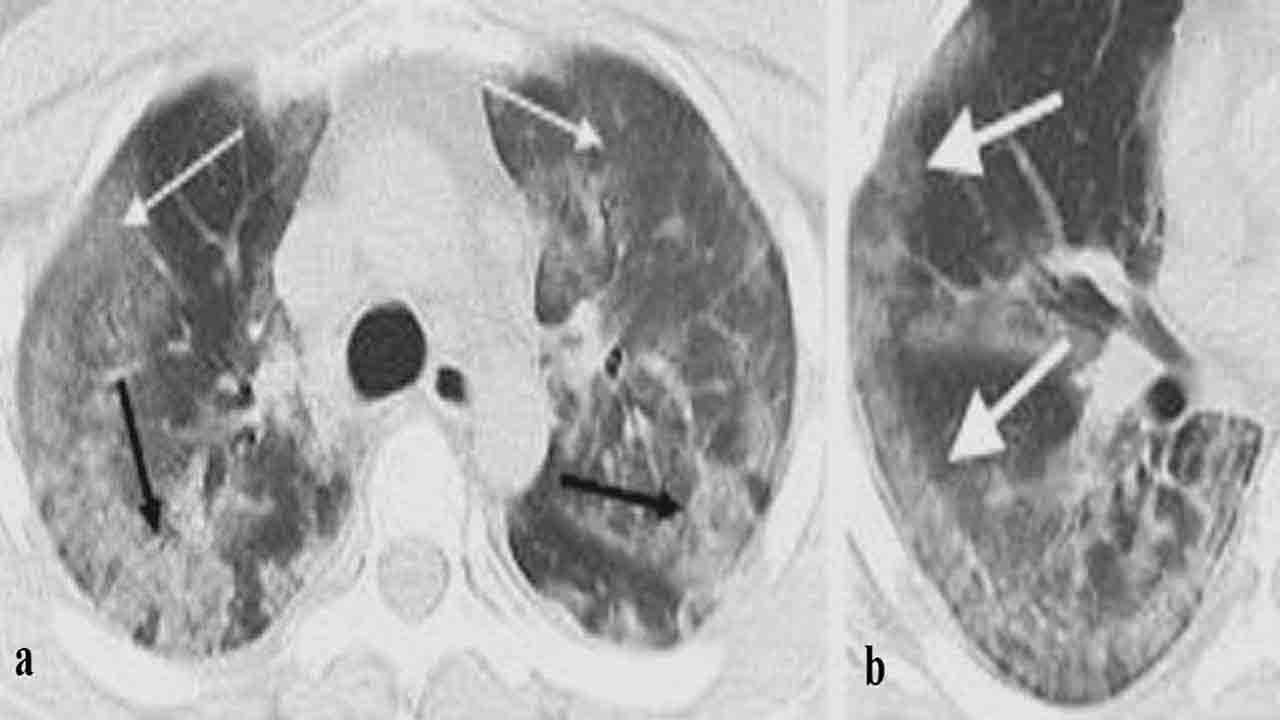
Biofeedback for Pulmonary Rehab-COVID 19
As the world continues to grapple with the effects of COVID-19, the importance of pulmonary rehabilitation has come to the forefront. Pulmonary rehab is essential for patients recovering from the virus, as it helps restore lung function and improve overall health. Incorporating targeted breathing exercises for the lungs can significantly enhance this rehabilitation process, promoting…
Heart Rate Variability in Athletes
Heart rate variability in athletes has gained significant attention as a crucial indicator of physical fitness and recovery. This metric reflects the body’s ability to adapt to stress and is particularly valuable for monitoring the training and performance of athletes. Analyzing the HRV of athletes, coaches, and trainers can gain insights into an athlete’s autonomic…