Achieving emotional balance is essential for overall well-being, yet many people struggle with emotional imbalance due to stress, lifestyle, and daily challenges. When emotions spiral out of control, they can negatively impact decision-making, relationships, and mental health. However, mastering self-management emotional intelligence allows individuals to regulate their emotional responses, build resilience, and maintain inner stability. Anyone can regain control and enhance their quality of life through emotional self-management techniques—including mindfulness, cognitive strategies, and biofeedback. In this article, we’ll explore the causes of emotional imbalance, its consequences, and effective methods to achieve lasting emotional stability.
What Is Emotional Balance and Why Does It Matter?
Emotions influence every aspect of our lives, from our thoughts and decisions to our relationships and overall well-being. Achieving emotional balance means maintaining a healthy relationship with our emotions—neither suppressing nor being overwhelmed by them. But why is this balance so important, and how does it shape our daily experiences?
Understanding Emotional Balance and Its Role in Well-Being
Emotional balance is the ability to experience emotions fully while controlling how they affect thoughts and behaviors. It doesn’t mean eliminating negative emotions but rather managing them in a way that supports mental and physical health.
When emotions are balanced, we can:

- Handle stress effectively without feeling overwhelmed
- Make rational decisions instead of acting impulsively
- Maintain healthy relationships by responding calmly to challenges
- Improve focus and productivity by reducing emotional distractions
On the other hand, emotional imbalance—whether it’s excessive anxiety, irritability, or emotional numbness—can lead to burnout, poor decision-making, and even physical health issues like high blood pressure or weakened immunity.
How Emotions Shape Your Life and Decision-Making

Our emotions influence how we perceive the world and react to situations. Whether we feel joy, anger, fear, or sadness, these emotions guide our thoughts and behaviors. Studies show that emotional responses can impact decision-making more than logic alone.
For example:
- Stress and frustration can lead to impulsive choices, often driven by short-term relief rather than long-term benefits.
- Fear and anxiety may cause avoidance behaviors, preventing us from taking necessary risks for growth.
- Positive emotions like gratitude and excitement encourage motivation, creativity, and stronger social connections.
Developing self-management emotional intelligence allows individuals to regulate emotions and make thoughtful decisions rather than being controlled by momentary feelings. This skill is essential for success in both personal and professional life.
The Next Step: Learning to Master Emotional Self-Management
Now that we understand why emotional balance matters, we will explore how to self-manage emotions effectively. The following chapter will explore emotional imbalance, its causes, and the consequences of unmanaged emotions.
Emotional Imbalance: Causes, Signs, and Consequences
While emotional ups and downs are a natural part of life, emotional imbalance occurs when negative emotions become overwhelming, persistent, or difficult to manage. It can manifest as mood swings, chronic stress, or emotional numbness, affecting both mental and physical well-being. But what causes emotional imbalance, and what are the long-term consequences?
What Leads to Emotional Imbalance?
Several factors can disrupt emotional stability, making it harder to regulate emotional responses and maintain emotional balance. The most common causes include:
♦ Chronic Stress and Burnout
High-pressure jobs, financial struggles, and personal conflicts can trigger prolonged stress. When stress becomes chronic, it disrupts the brain’s ability to regulate emotions, leading to heightened anxiety, irritability, and exhaustion.
♦ Unresolved Trauma and Emotional Suppression
Past traumatic experiences, whether from childhood, relationships, or major life events, can leave lasting emotional wounds. Suppressing emotions instead of addressing them can cause emotional detachment, outbursts, or unpredictable mood shifts.
♦ Unhealthy Lifestyle Choices
- Poor sleep affects mood regulation and cognitive function, increasing emotional reactivity.
- An unbalanced diet (high sugar, caffeine, processed foods) contributes to mood swings and irritability.
- Lack of physical activity reduces endorphins and serotonin levels, increasing stress and emotional instability.
♦ Hormonal and Neurological Imbalances
Fluctuations in hormones (such as cortisol, serotonin, or dopamine) significantly affect emotional regulation. Conditions like anxiety, depression, and even hormonal imbalances due to thyroid dysfunction or menopause can lead to emotional imbalance.
The Hidden Costs: Health, Relationships, and Performance
Ignoring emotional imbalance can have widespread consequences, affecting every aspect of life.
! Health Consequences
- Increased risk of anxiety, depression, and panic attacks
- Weakened immune system and frequent illnesses
- Sleep disturbances, chronic fatigue, and headaches
- Elevated blood pressure and heart disease risk
! Relationship Struggles
- Difficulty in expressing emotions leads to misunderstandings
- Increased conflicts due to mood swings and emotional outbursts
- Emotional withdrawal or detachment from loved ones
- Loss of social connections due to irritability or lack of engagement
! Impact on Performance and Decision-Making
- Reduced concentration, productivity, and problem-solving abilities
- Poor decision-making due to heightened emotional reactions
- Increased procrastination and lack of motivation
- Higher risk of burnout and job dissatisfaction
Breaking the Cycle: Moving Toward Emotional Self-Management
Now that we understand the dangers of emotional imbalance, the next step is learning how to self-manage emotions effectively. In the next chapter, we’ll explore emotional self-management, why it’s crucial, and how it enhances resilience and mental clarity.
The Power of Emotional Self-Management
In a world full of challenges, setbacks, and uncertainties, mastering emotional self-management is essential for maintaining inner stability and achieving personal and professional success. When emotions are left unchecked, they can dictate decisions, strain relationships, and even harm physical health. But with the right strategies, it’s possible to develop greater control over emotional responses and build resilience in the face of adversity.
What Is Emotional Self-Management and Why Is It Essential?
Emotional self-management is the ability to regulate emotions in a way that supports well-being, decision-making, and interpersonal relationships. It’s a key component of self-management emotional intelligence, enabling individuals to:
- Stay calm under pressure and respond thoughtfully instead of reacting impulsively
- Reduce stress and anxiety by managing emotional triggers effectively
- Improve focus and productivity by minimizing emotional distractions
- Strengthen relationships through better communication and emotional control
People who lack emotional self-management may experience frequent mood swings, struggle with emotional outbursts, or suppress emotions until they build up and cause breakdowns. Over time, poor emotional regulation can lead to chronic stress, burnout, and difficulty adapting to life’s inevitable changes.
How the Self-Management Emotional Intelligence Builds Resilience
Resilience is the ability to bounce back from setbacks, adapt to change, and keep moving forward despite challenges. Developing self-management emotional intelligence is key to building resilience, as it allows individuals to process emotions effectively rather than being controlled by them.
♦ Recognizing and Understanding Emotional Triggers
By identifying emotional triggers—whether it’s criticism, failure, or stress—people can take proactive steps to regulate their emotional responses before they escalate.
♦ Shifting from Reaction to Response
Instead of reacting impulsively, emotionally intelligent individuals pause, assess their feelings, and choose a response that aligns with their long-term goals and values. This skill is particularly valuable in high-stress situations requiring a level-headed approach.
♦ Practicing Mindfulness and Self-Awareness
Mindfulness techniques, such as deep breathing, meditation, or body scanning, help individuals stay present and prevent emotions from spiraling out of control. Increased self-awareness also allows for greater emotional insight and regulation.
♦ Using Biofeedback for Emotional Regulation
Cutting-edge biofeedback technologies provide real-time data on physiological responses, helping users develop better emotional control. Devices like:
- Mendi Headband trains brain activity for better focus and stress management
- NeuroVizr uses light and sound to promote relaxation and emotional balance
- BioSignals 5 sensor biofeedback device optimizes physiological states for stress reduction and self-regulation
- HeartMath biofeedback device helps in relaxation, emotional balance, and better focus.
From Emotional Control to Mastery: What’s Next?
Emotional self-management is the foundation for emotional balance, resilience, and success. As we move forward, we will delve deeper into emotional responses, examine how they shape our interactions, and explore practical strategies to master them effectively.
Mastering Emotional Responses: The Key to Inner Stability
Emotions influence every aspect of life—from decision-making and relationships to performance and well-being. While emotions themselves are neither good nor bad, how we respond to them can make all the difference. Mastering emotional responses allows for greater control, clarity, and resilience, preventing emotional upheavals from taking over.
How to Recognize and Control Your Emotional Responses
Before emotions can be managed, they must first be understood. Emotional responses are automatic reactions triggered by internal or external events. Recognizing them early is the first step toward developing emotional stability.
♦ Identify Emotional Triggers
Understanding what sparks strong emotional reactions—such as criticism, failure, or stress—helps prevent impulsive responses. Keeping an emotional journal or practicing mindfulness can enhance self-awareness.
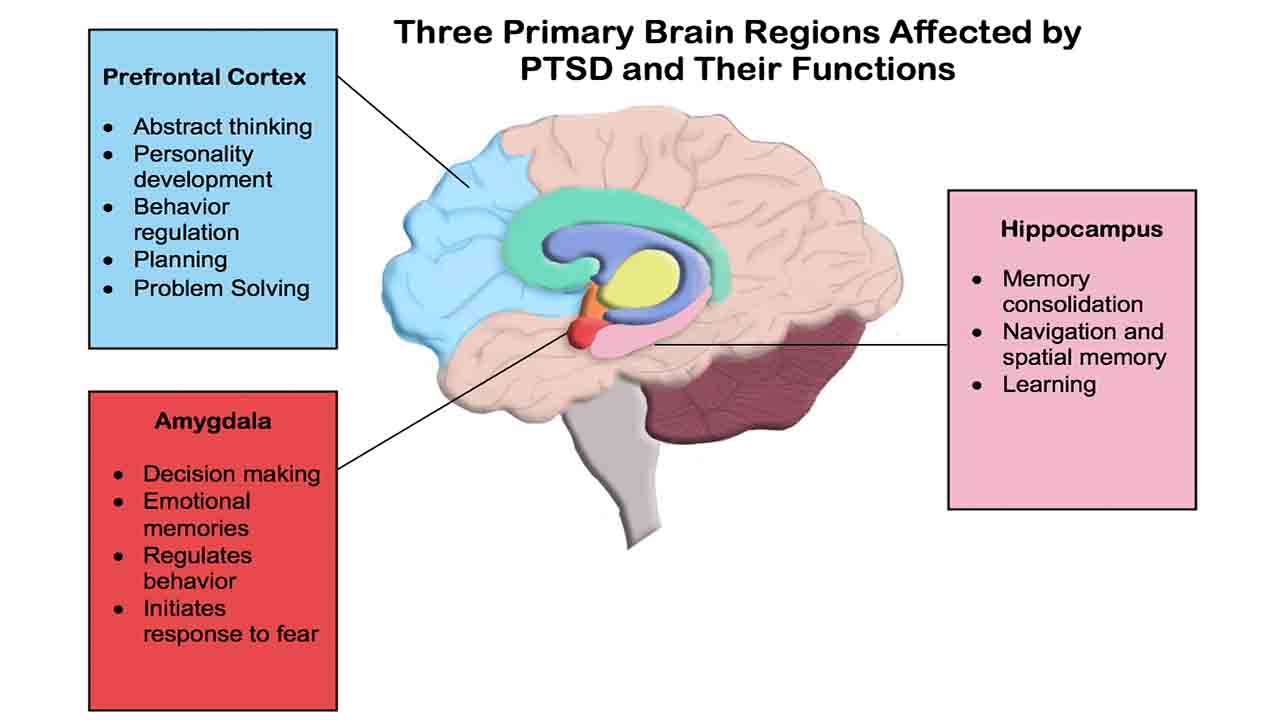
♦ Understand the Role of the Nervous System
When faced with emotional challenges, the brain activates the fight-or-flight response, releasing stress hormones. Learning to regulate this reaction helps prevent emotional overwhelm and promotes clear thinking.
♦ Pause Before Reacting
When emotions rise, take a deep breath, count to five, and assess the situation. This small pause can create space for a thoughtful response instead of an automatic reaction.
♦ Use Biofeedback to Monitor Emotional Responses
Biofeedback tools provide real-time data on physiological reactions, helping individuals gain better control over their emotions:
- Heart Rate Variability (HRV) Biofeedback (BioSignals 5 sensor biofeedback device) (HeartMath HRV biofeedback device) enhances stress resilience.
- Galvanic Skin Response (GSR) Biofeedback (BioSignals 5 sensor biofeedback device) tracks emotional arousal levels.
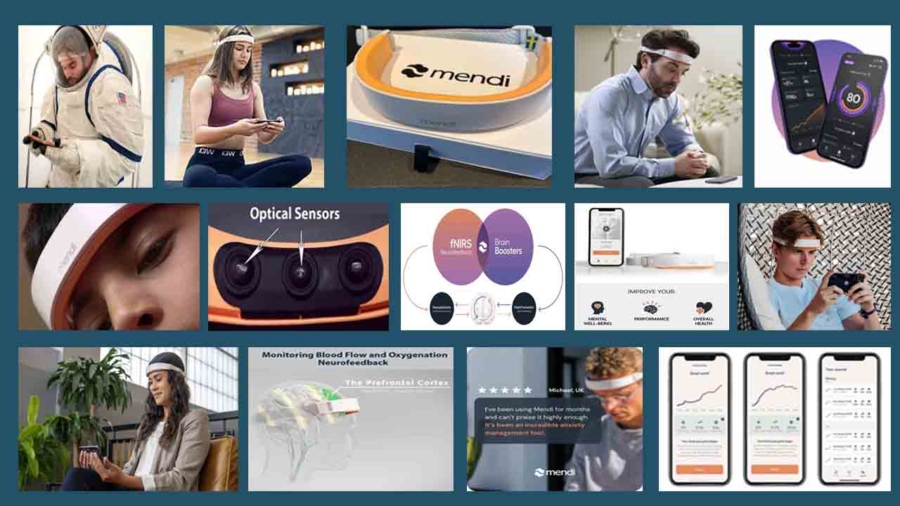
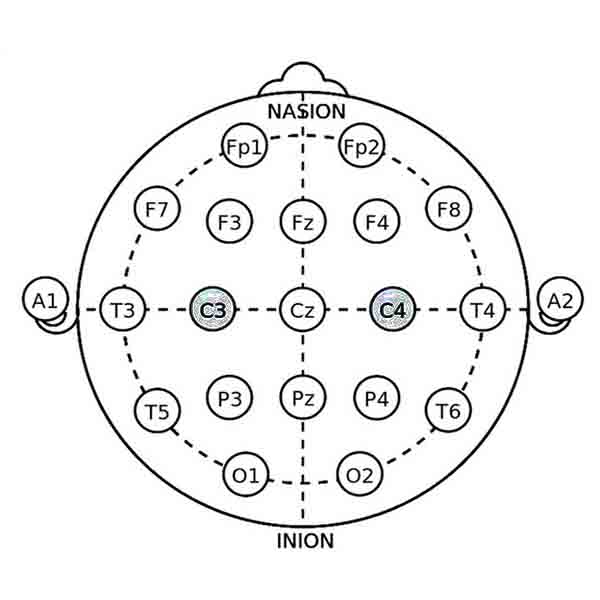
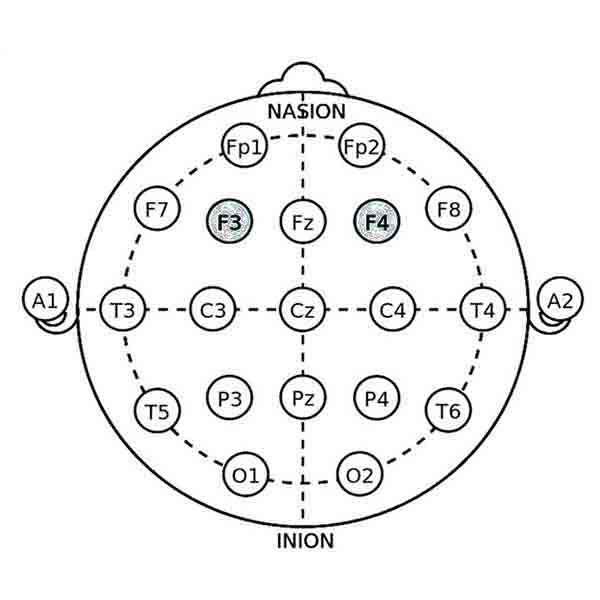
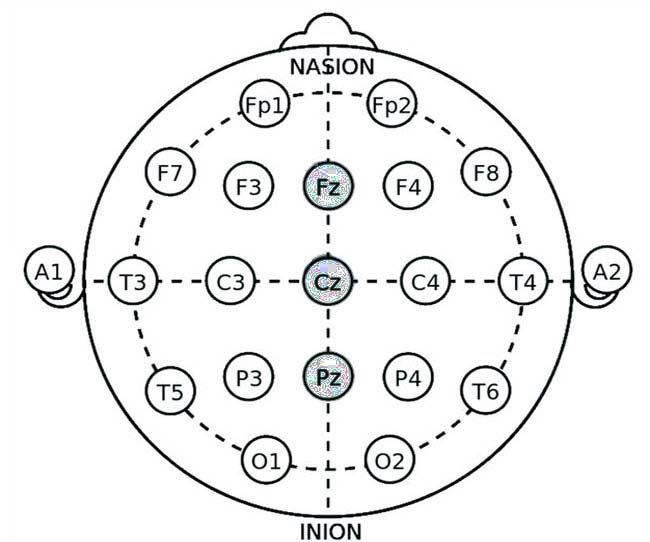
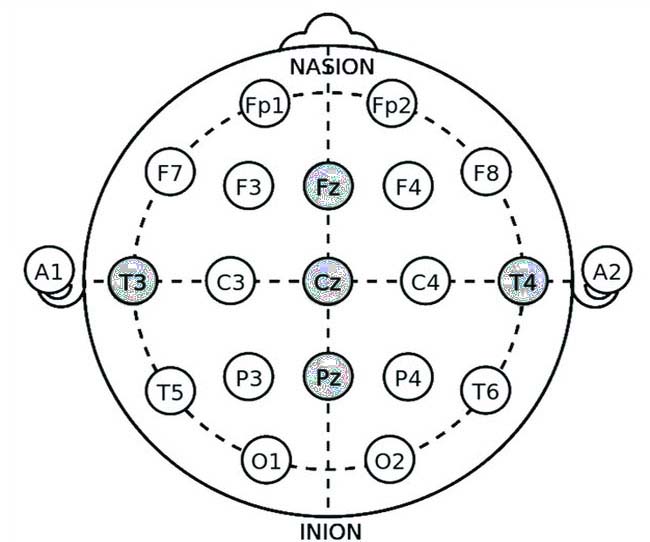
- Mendi Headband improves emotional regulation by strengthening prefrontal cortex activity.
Strategies to Shift from Reactivity to Emotional Control
Developing emotional control requires practice and the right techniques. The following strategies help shift from reactive patterns to intentional responses.
♦ Cognitive Reframing: Change the Narrative
Instead of reacting emotionally to setbacks, shift perspective. Ask: Is there another way to interpret this situation? Reframing negative experiences helps reduce emotional distress.
♦ Breathing Techniques for Instant Calm
Slow, deep breathing activates the parasympathetic nervous system, signaling relaxation. Try 4-3-8 breathing: inhale for 4 seconds, hold for 3, exhale for 8.
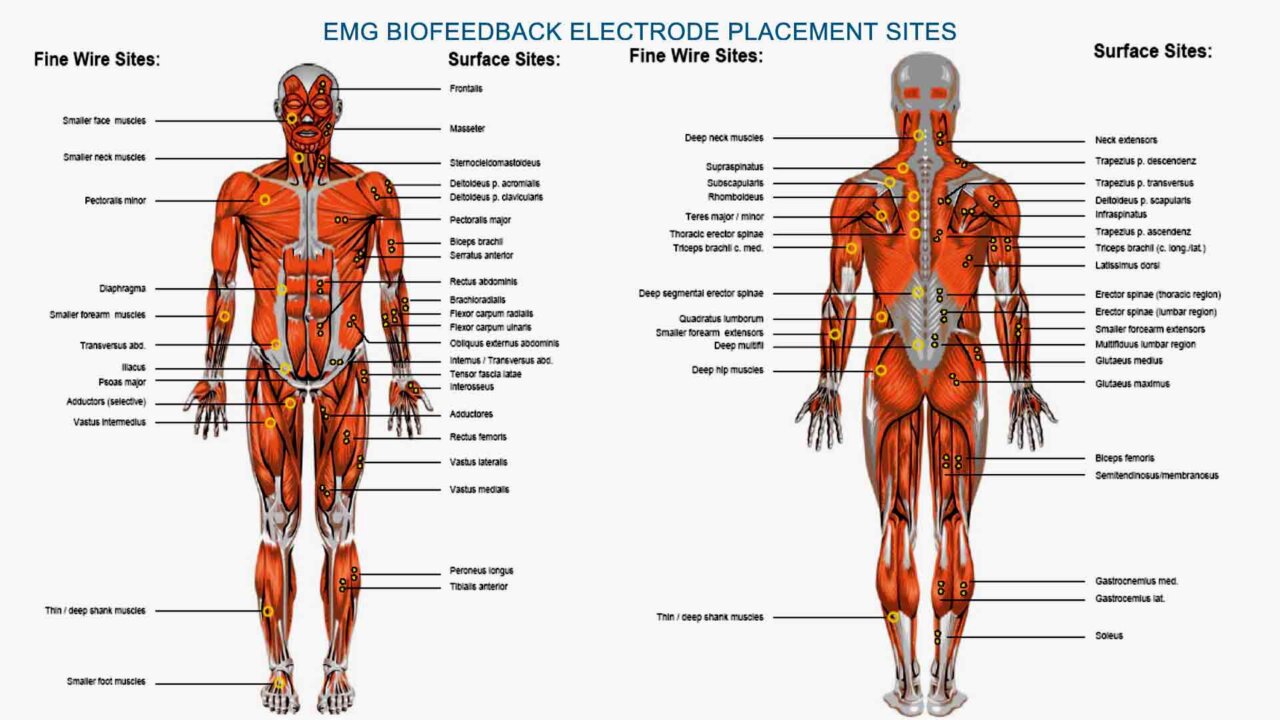
♦ Progressive Muscle Relaxation (PMR)
Tensing and relaxing different muscle groups releases stored emotional tension, bringing immediate calm. The best biofeedback device for muscle relaxation is Neurotrac Simplex.
♦ Mindfulness and Meditation
Regular meditation strengthens self-management and emotional intelligence, improving emotional resilience over time.
Achieving Emotional Balance: What’s Next?
By mastering emotional responses, individuals regain control over their inner world, leading to emotional balance and improved decision-making. In the next chapter, we’ll explore advanced emotional self-management techniques, including biofeedback, for long-term emotional stability.
Biofeedback: A Science-Backed Approach to Emotional Balance
Achieving emotional balance requires more than just willpower; instead, it involves training both the mind and body to handle stress in a healthier way. Fortunately, biofeedback offers a cutting-edge, science-backed solution that empowers individuals to regulate their emotional responses. By providing real-time feedback on physiological states, this method not only enhances emotional self-management but also fosters long-term resilience.

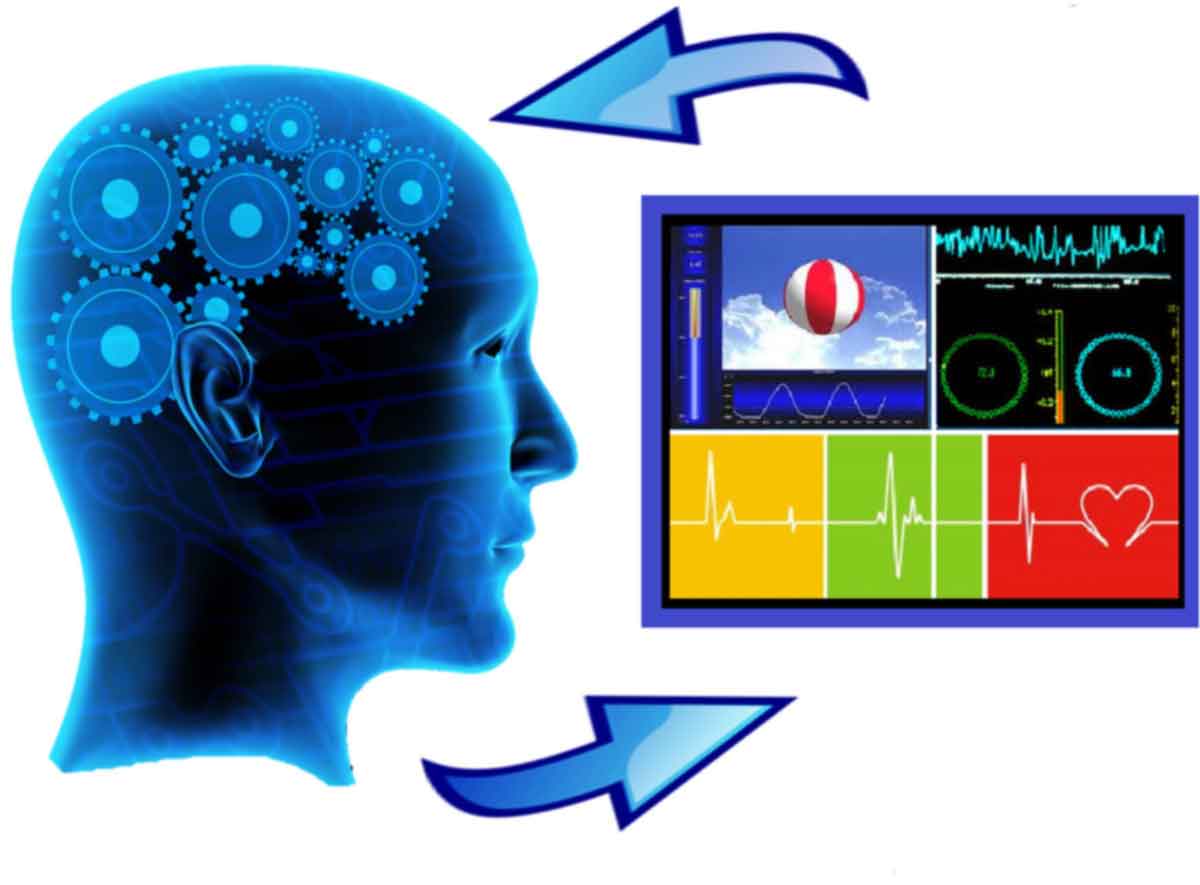
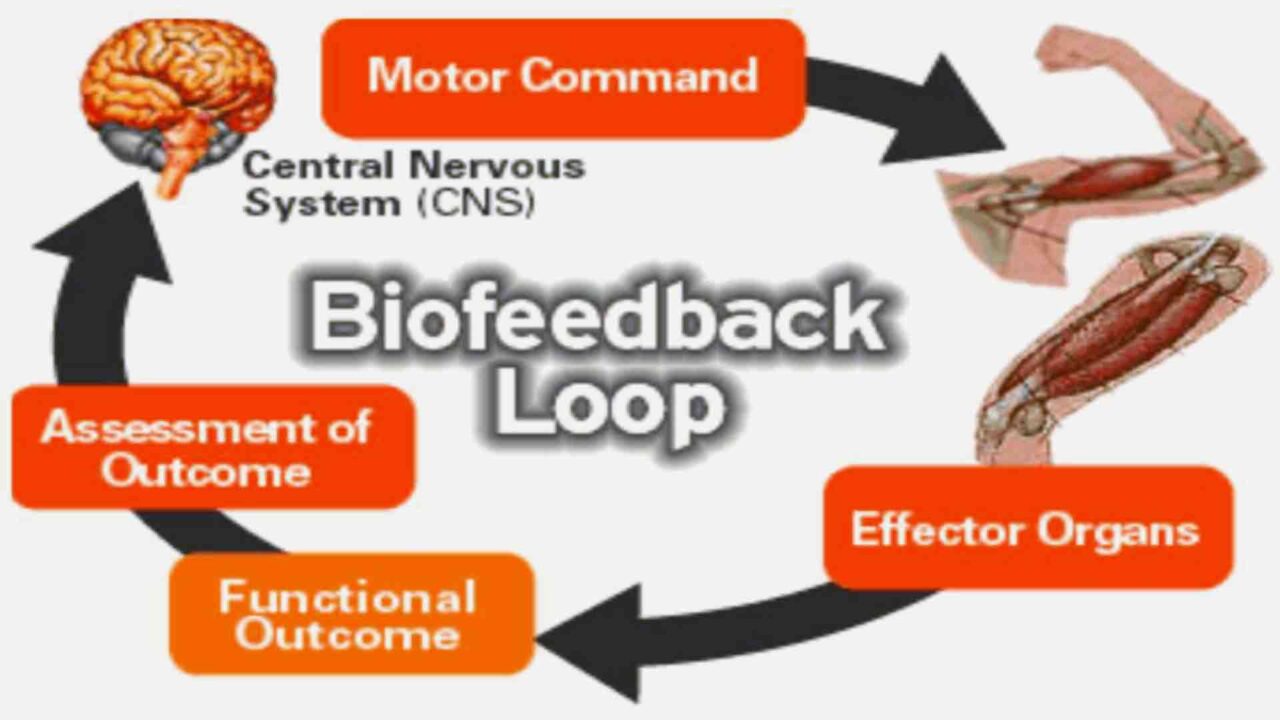
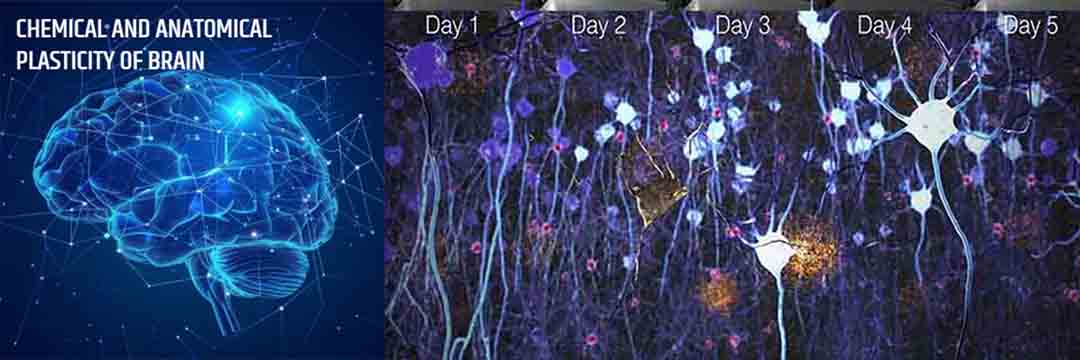
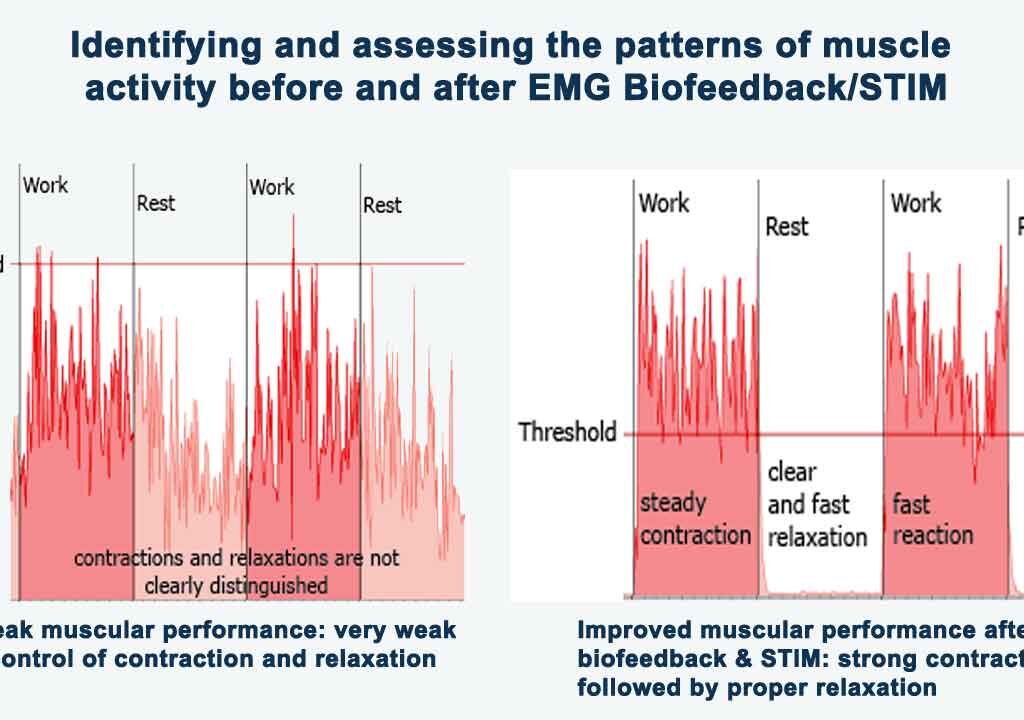
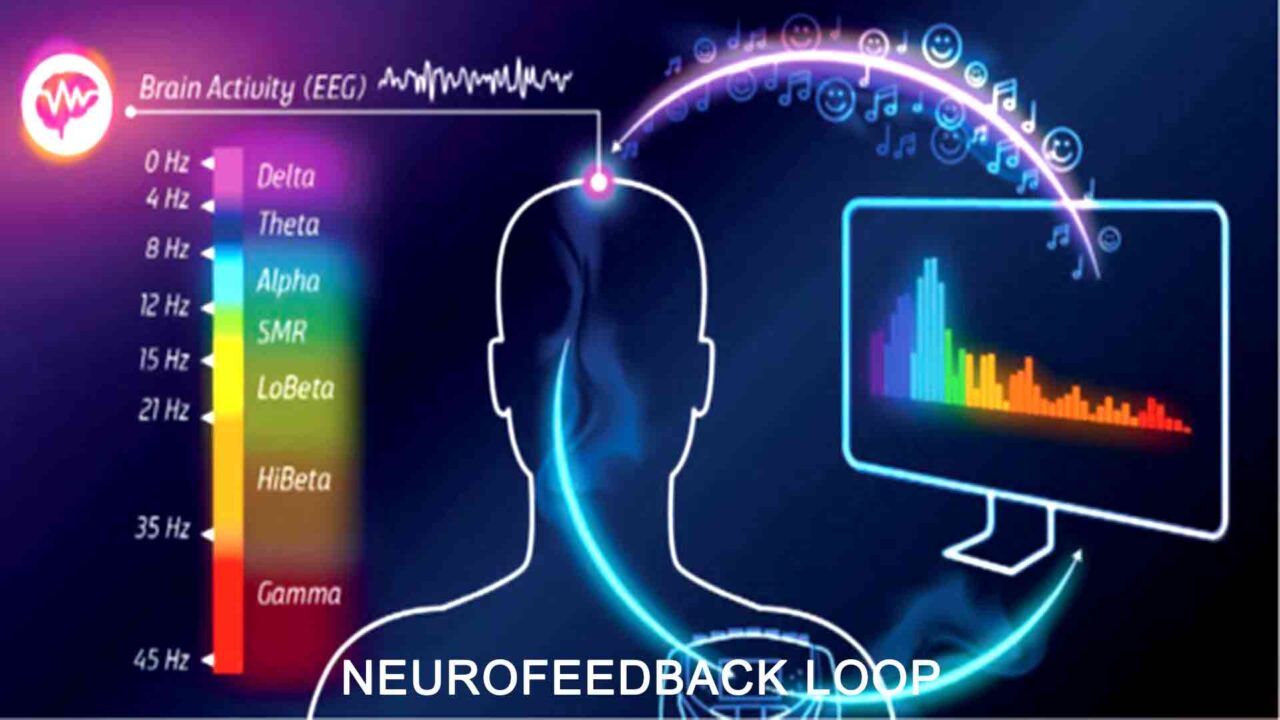
How Biofeedback Trains the Brain for Emotional Self-Management
Biofeedback monitors physiological signals—such as heart rate, brain activity, skin conductivity, and breathing patterns—and displays the data in real-time. Observing these responses allows individuals to control their emotional states and reduce stress more effectively.
Key Benefits of Biofeedback for Emotional Self-Management
- Enhances awareness of emotional triggers
- Helps shift from emotional imbalance to emotional stability
- Trains the brain for better self-management emotional intelligence
- Reduces stress-related symptoms like anxiety, irritability, and mood swings
The process involves using biofeedback devices that measure biological responses and provide instant feedback. This enables individuals to adjust their breathing, thoughts, or focus to create a state of calm and control.
The Role of Neurofeedback and Physiological Biofeedback
There are two primary types of biofeedback used for emotional regulation:
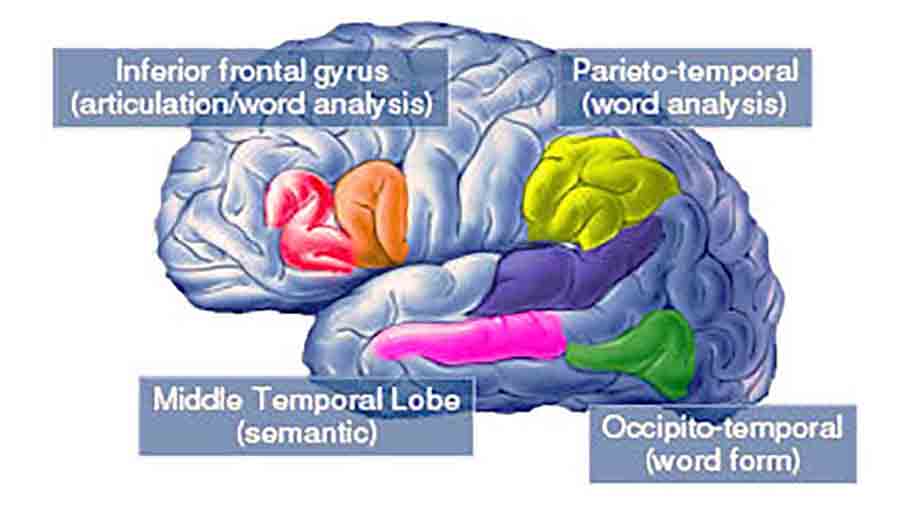
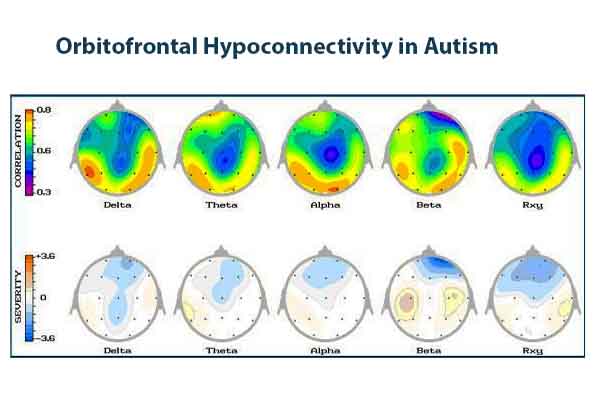
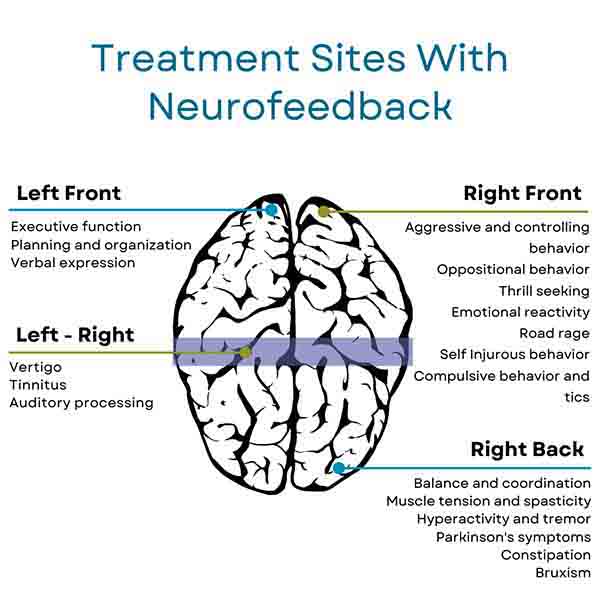
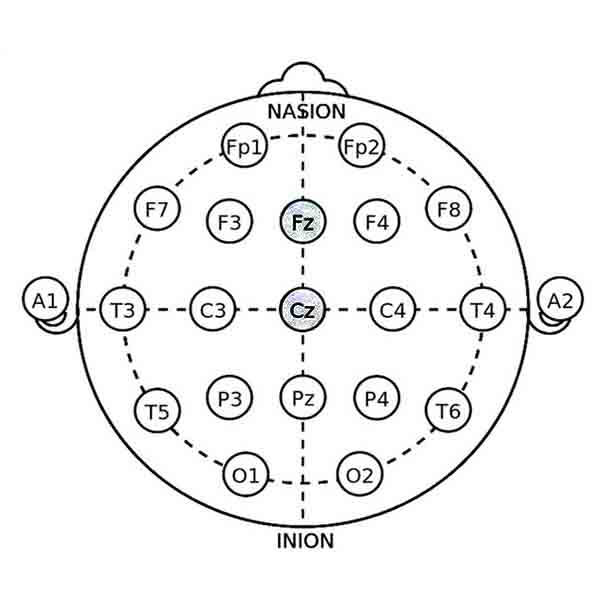
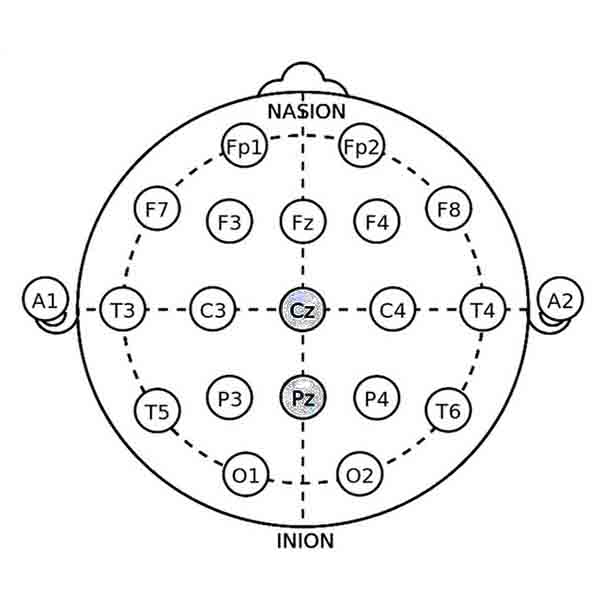
1. Neurofeedback: Training the Brain for Emotional Control
Neurofeedback is a form of biofeedback that focuses on brain activity. It helps individuals regulate emotional responses by training specific brain regions.
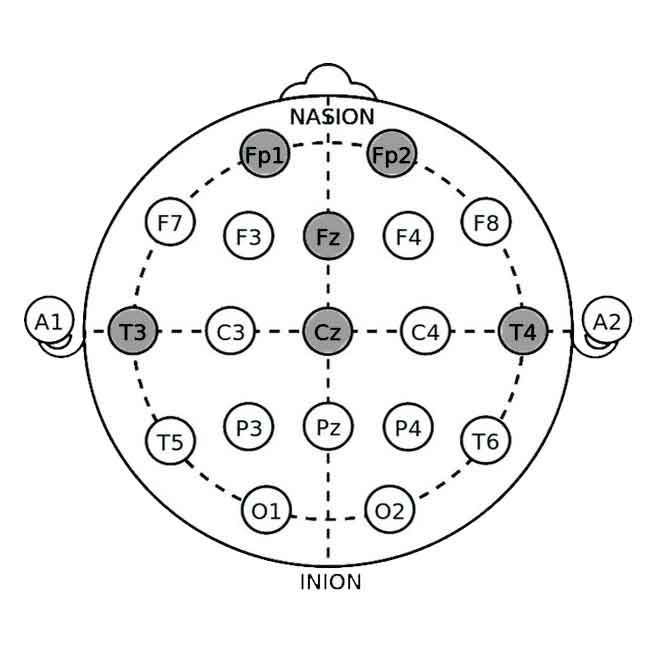
♦ Mendi Headband: Uses blood flow measurement in the prefrontal cortex to enhance focus, emotional stability, and stress resilience.
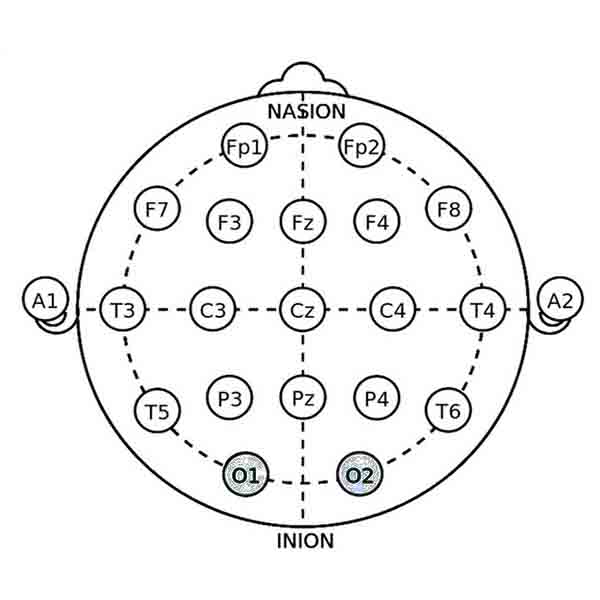
♦ NeuroVizr: Light stimulation influences brainwave activity, promoting relaxation and emotional well-being.
2. Physiological Biofeedback: Regulating the Body’s Emotional Signals
Emotions are deeply connected to physiological responses. Biofeedback devices help regulate these signals for better emotional control.
- Heart Rate Variability (HRV) Biofeedback (BioSignals 5 sensor device): Trains the autonomic nervous system to manage stress and anxiety more effectively.
- Breathing Biofeedback (BioSignals 5 sensor device): Improves breathing patterns for emotional regulation.
- Galvanic Skin Response (GSR) Biofeedback (BioSignals 5 sensor device): Detects emotional arousal and helps individuals learn to calm their reactions.
- Thermal Biofeedback (BioSignals 5 sensor device): Tracks stress-related temperature changes and teaches relaxation techniques.
From Biofeedback to Lasting Emotional Mastery
Biofeedback is a powerful tool for achieving emotional balance. It provides insights into emotional and physiological patterns. By integrating these techniques, individuals can develop long-term emotional resilience and self-regulation skills.
In the next chapter, we’ll explore how to integrate biofeedback techniques into daily life for sustainable emotional well-being.
Top Biofeedback Devices for Emotional Self-Management
Technology has made emotional self-management more accessible than ever. With advanced biofeedback devices, individuals can monitor and regulate their emotional responses, achieving greater emotional balance and resilience. These tools provide real-time feedback, helping users train their nervous system for stress reduction, focus, and overall well-being.
Let’s explore some of the most effective biofeedback and neurofeedback devices for emotional regulation.
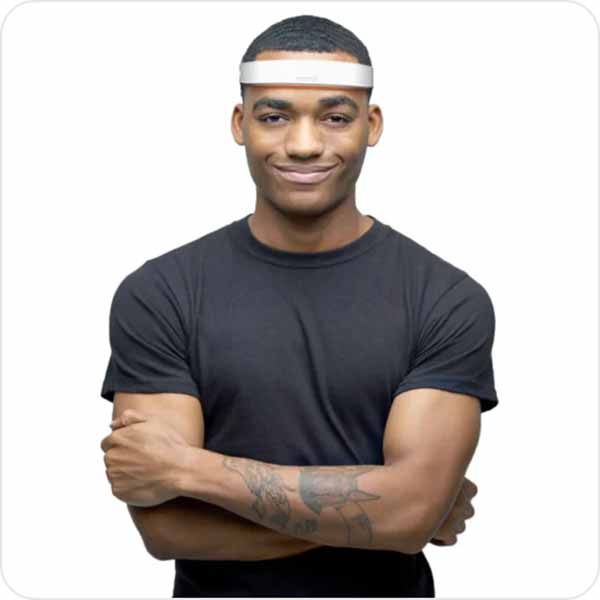
Mendi Headband: Training Blood Flow for a Calmer Mind
The Mendi Headband is a groundbreaking neurofeedback device that enhances emotional regulation by training prefrontal cortex activity. This brain region is responsible for decision-making, impulse control, and emotional balance.
How It Works:
- Uses functional near-infrared spectroscopy (fNIRS) to measure blood flow in the prefrontal cortex.
- Encourages the brain to optimize its function through interactive mental exercises.
- Trains users to stay calm, focused, and emotionally resilient.
Benefits for Emotional Self-Management:
✅ Strengthens self-management emotional intelligence
✅ Reduces stress and anxiety levels
✅ Improves focus and impulse control
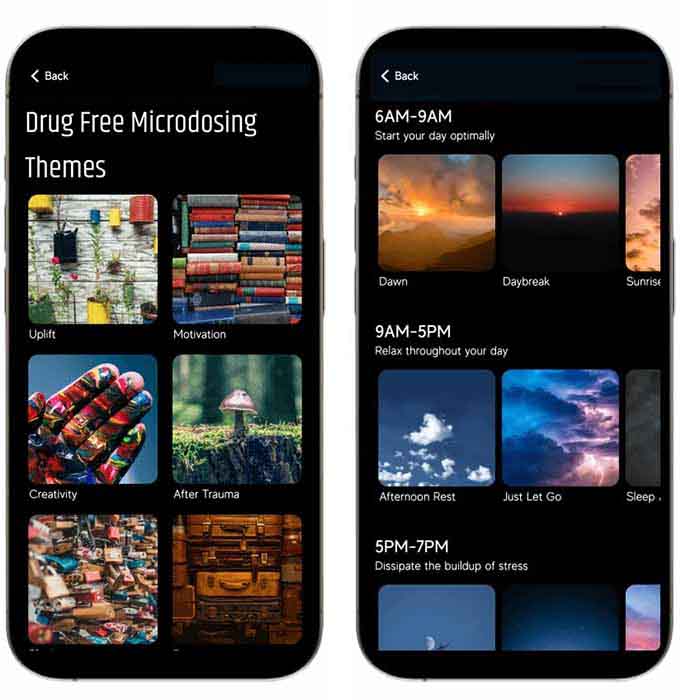
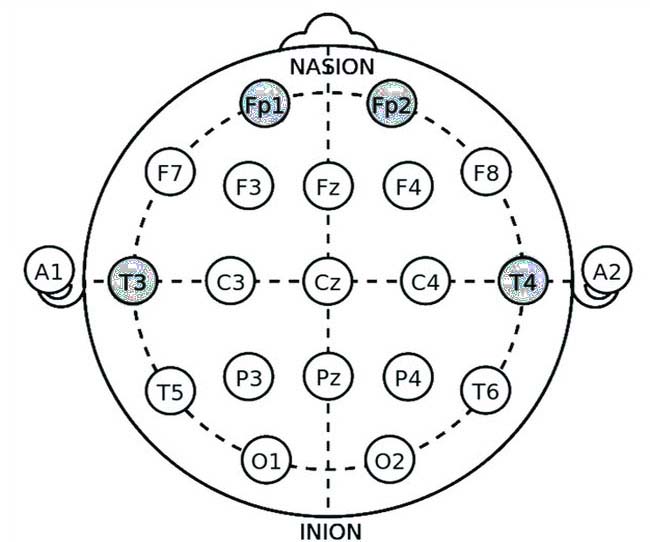
NeuroVizr: Light and Sound for Emotional Regulation
The NeuroVizr is a brainwave entrainment device that uses pulsing light and sound stimulation to influence brain activity and promote emotional stability.
How It Works:
- Uses flashing light frequencies and audio stimulation to guide the brain into desired states (relaxation, focus, or energy).
- Helps regulate emotional responses by influencing neural activity.
- Supports mental clarity and reduces emotional imbalance.
Benefits for Emotional Regulation:
✅ Induces relaxation and emotional stability
✅ Enhances cognitive function and mental clarity
✅ Reduces stress and improves sleep quality
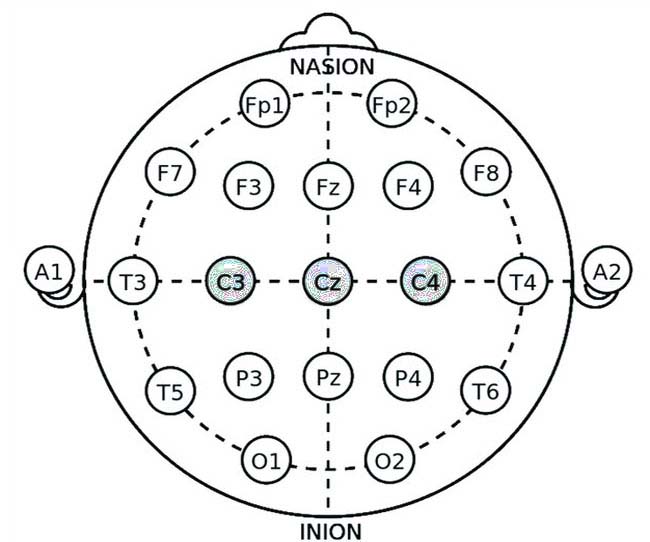
BioSignals HRV, GSR, Thermal, and Breathing: A Holistic Biofeedback Toolkit
While understanding the theory of emotional self-regulation is crucial, the fundamental transformation begins with practice. This is where biofeedback becomes an invaluable tool, acting as a mirror to our internal state. Among the advanced devices available, the Biosignal 5 sensor biofeedback system stands out as a comprehensive toolkit for anyone seeking to achieve deeper emotional balance. It translates the subtle language of the autonomic nervous system (ANS) into precise, real-time data, empowering users to move from feeling overwhelmed by their physiology to actively guiding it.
From Abstract to Tangible: The Principles of Biofeedback
Biofeedback is founded on a simple yet powerful principle: if you can measure a physiological function, you can learn to control it. By receiving immediate feedback about processes typically outside conscious awareness—like heart rate, sweat gland activity, or skin temperature—we can develop strategies to influence them. The Biosignal 5 makes this principle accessible, providing a direct window into the balance between the sympathetic (SNS – “fight-or-flight”) and parasympathetic (PNS – “rest-and-digest”) branches of the ANS.
The Biosignal 5: A Multi-Dimensional Approach to Self-Awareness
What sets the Biosignal 5 apart is its integrated multi-sensor design. Instead of focusing on a single metric, it provides a holistic picture of your autonomic state by simultaneously monitoring four key biosignals:
Heart Rate Variability (HRV): The Rhythm of Resilience
HRV is the subtle variation in time between each heartbeat. It is a primary indicator of ANS flexibility and emotional regulation capacity. A high, complex HRV signifies a healthy balance where the body can efficiently adapt to stress and recover quickly. The Biosignal 5 uses a precise pulse plethysmograph (PPG) sensor to measure HRV. Through guided breathing exercises, users can see in real-time how slow, diaphragmatic breathing increases their HRV, directly strengthening the calming influence of the parasympathetic nervous system.
Galvanic Skin Response (GSR): The Gauge of Arousal
Also known as Electrodermal Activity (EDA), GSR measures the electrical conductivity of your skin, which increases slightly as you sweat. This is one of the most sensitive indicators of emotional arousal and SNS activation. The Biosignal 5’s GSR sensors provide an immediate feedback loop for stress or anxiety. By observing the GSR signal rise during a stressful thought and then fall as you practice a calming technique, you gain concrete evidence of your ability to self-soothe.
Thermal Feedback: The Flow of Relaxation
Peripheral skin temperature is a direct reflection of blood flow. During stress (SNS dominance), blood vessels constrict, moving blood away from the extremities and causing hands and feet to feel cold. As you relax (PNS dominance), these vessels dilate, warming the hands. The Biosignal 5’s temperature sensor allows users to practice “warming their hands” through visualization and relaxation, a classic biofeedback technique that directly trains the body to shift out of a stress state.

Breathing (Respiration): The Lever of Control
Breathing is unique—it is both an automatic and a voluntarily controlled function. The Biosignal 5 includes a respiration belt that tracks breathing rate and depth. Erratic, shallow chest breathing is linked to anxiety, while slow, deep diaphragmatic breathing promotes calm. The device provides real-time feedback on breathing patterns, guiding users to pace their breath in a way that optimally stimulates the vagus nerve and enhances HRV, creating a powerful positive feedback loop for relaxation.
Integrating the Signals for Powerful Insights
The true power of the Biosignal 5 lies in the correlation of these signals. For instance, you might observe a scenario where:
- A stressful thought arises.
- Your GSR spike provides the first clue of arousal.
- Your breathing becomes shallow and rapid.
- Your HRV pattern becomes more rigid.
- Your finger temperature begins to drop.
Witnessing this cascade in real-time makes the mind-body connection undeniable. More importantly, you can then intervene using a breathing or mindfulness technique and watch the entire system return to balance: GSR settles, HRV becomes complex, and temperature rises. This integrated feedback transforms abstract concepts like “calm down” into a tangible, learnable skill.
Conclusion: Empowering Your Self-Management Journey
The Biosignal 5 is more than a device; it is a personal biofeedback laboratory. By making the invisible visible, it demystifies the body’s response to emotion and provides a practical pathway to mastery. In the context of emotional balance and self-management, it serves as a dedicated trainer, helping individuals move from reactive patterns to proactive, conscious control. By regularly engaging with this holistic toolkit, users can rewire their nervous system’s habitual responses, building the resilience and emotional flexibility that are the hallmarks of true well-being.
HeartMath in Regulating Emotional Balance
While many biofeedback methods target the brain or specific stress responses, the HeartMath Institute has pioneered a unique approach focused on the heart. HeartMath techniques are designed to create heart coherence, a state where the heart, brain, and nervous system are in harmonious synchronization. This state is fundamental to achieving deep emotional balance and resilience.
HeartMath operates on the principle that the heart has its own complex nervous system (“the heart-brain”) that communicates with the brain. During stress or emotional imbalance, heart rhythms become erratic and disordered—a pattern known as incoherence. This incoherence signals the brain to activate the stress response, impairing clear thinking and emotional control.
The core of the HeartMath method involves using a biofeedback device, often paired with a sensor on the earlobe or finger, to display your heart rate variability (HRV) in real-time. Through simple exercises like Focused Heart Breathing—where you consciously breathe slowly and evenly while focusing on cultivating a positive emotion, such as appreciation or care—you learn to shift your heart rhythm into a smooth, wave-like pattern of coherence.
The benefits are profound. Achieving heart coherence quickly reduces cortisol levels, calms the nervous system, and enhances cognitive function. By practicing these techniques regularly, individuals can self-generate a state of calm on demand, leading to improved emotional regulation, better decision-making, and a greater capacity to navigate daily challenges with stability and clarity. It effectively trains the body’s intrinsic regulatory systems to support, rather than undermine, emotional well-being.
Choosing the Right Biofeedback Device for Your Needs
Each biofeedback device offers unique benefits, but the best choice depends on individual goals:
- For cognitive and emotional control → Mendi Headband
- For brainwave and sensory regulation → NeuroVizr
- For heart rate-based emotional self-management → BioSignals 5 sensor device or HeartMath
- For stress detection and control → BioSignals 5 sensor device
- For relaxation and thermal biofeedback → BioSignals 5 sensor device
- For breath-based emotional regulation → BioSignals 5 sensor device
Harnessing Biofeedback for Lasting Emotional Balance
By integrating biofeedback technology, individuals can train their minds and bodies for long-term emotional stability. In the next chapter, we’ll explore practical strategies for incorporating biofeedback into daily life for sustainable emotional well-being.
How to Build Lasting Emotional Balance in Daily Life
Achieving emotional balance is not a one-time effort—it’s a lifelong practice that requires self-awareness, consistency, and the right tools. By integrating biofeedback, mindfulness, and self-reflection into daily life, you can build emotional resilience and enhance your overall well-being.
In this chapter, we’ll explore practical strategies for mastering your emotional responses, reducing stress, and cultivating long-term emotional self-management.
Practical Techniques for Everyday Emotional Mastery
Maintaining emotional balance involves recognizing emotional triggers, regulating stress, and making intentional lifestyle choices. Here are key techniques to develop emotional stability:
Monitor and Regulate Your Stress Levels with Biofeedback
📌 Why It Works: Stress disrupts emotional balance. Biofeedback helps you track and regulate physiological responses linked to stress and emotional arousal.
✅ Use HeartMath or BioSignals 5 sensor device to monitor and improve heart rate variability for emotional resilience.
✅ Practice GSR biofeedback to track emotional arousal and develop better stress control.
✅ Train your brain with the Mendi Headband to strengthen cognitive and emotional regulation.
Practice Deep Breathing for Instant Emotional Control
📌 Why It Works: Conscious breathing slows the heart rate, reduces cortisol (stress hormone), and activates the parasympathetic nervous system, promoting calmness.
✅ Use BioSignals 5 sensor device to track and improve your breathing patterns.
✅ Try box breathing (inhale for 4 seconds, hold for 4 seconds, exhale for 4 seconds, hold for 4 seconds).
✅ Engage in diaphragmatic breathing to shift from reactive to controlled responses.
Strengthen Self-Awareness with Emotional Journaling
📌 Why It Works: Writing down your thoughts and emotions helps identify patterns, triggers, and areas for growth.
✅ Reflect on emotional triggers and note how you respond to stressful situations.
✅ Keep a mood journal to track daily emotional shifts.
✅ Pair journaling with biofeedback to monitor progress in emotional regulation.
Use Mindfulness to Stay Present and Reduce Overwhelm
📌 Why It Works: Mindfulness helps break the cycle of emotional reactivity by bringing attention to the present moment.
✅ Practice mindfulness meditation for 5–10 minutes daily.
✅ Use NeuroVizr’s light and sound technology to enhance meditation and mental clarity.
✅ Engage in mindful walking or mindful eating to stay grounded.
Develop Healthy Sleep and Lifestyle Habits
📌 Why It Works: Poor sleep and unhealthy habits contribute to emotional imbalance and increased stress. Optimizing your routine supports emotional stability.
✅ Maintain consistent sleep schedules for better mood regulation.
✅ Engage in regular physical activity to balance stress hormones.
✅ Reduce caffeine, sugar, and processed foods, which can impact emotional health.
Cognitive Behavioral Therapy (CBT) for Emotional Balance
Cognitive Behavioral Therapy (CBT) is one of the most effective psychological approaches to managing emotions. It focuses on changing negative thought patterns and behaviors contributing to emotional imbalance.
How CBT Helps with Emotional Self-Management
📌 Why It Works: Your thoughts directly influence your emotions and reactions. By reshaping your thinking patterns, you can improve emotional resilience and avoid unnecessary distress.
✅ Identify Cognitive Distortions: Learn to recognize exaggerated negative thoughts (e.g., “I always fail,” “No one likes me”) and replace them with more balanced, realistic perspectives.
✅ Challenge Negative Thoughts: Ask yourself, Is this thought based on facts or assumptions? Reframing irrational thoughts reduces emotional distress.
✅ Practice Thought Replacement: Replace automatic negative thoughts with constructive affirmations (e.g., “I can handle this,” “I am capable of learning and adapting”).
Integrating CBT with Biofeedback and Mindfulness
📌 Why It Works: Combining CBT with biofeedback and mindfulness creates a powerful, science-backed approach to emotional self-management.
✅ Use biofeedback tools (HRV, GSR, Mendi Headband) to track physiological responses while practicing CBT techniques.
✅ Apply CBT strategies during mindfulness sessions to reinforce new thinking habits.
✅ Journaling CBT exercises alongside biofeedback data helps visualize progress and reinforce positive change.
Combining Biofeedback, Mindfulness, and CBT for Long-Term Emotional Balance
For lasting emotional self-management, it’s essential to combine multiple techniques that reinforce each other. Here’s how:
✔ Start your day with mindfulness practice and a quick HRV biofeedback session.
✔ Use biofeedback tools throughout the day to monitor emotional responses.
✔ Apply CBT techniques when negative thoughts arise to shift toward a balanced perspective.
✔ Journal in the evening to reflect on emotional patterns and progress.
✔ Incorporate breathwork whenever you feel stress building up.
Final Thoughts: Mastering Emotional Balance for Life
Developing emotional balance is a continuous process, but with biofeedback, mindfulness, and CBT, you can create a solid foundation for long-term emotional intelligence and resilience.
By implementing these strategies into daily life, you’ll enhance your ability to stay calm, focused, and in control—no matter what challenges come your way.
Conclusion: Take Control of Your Emotional Well-Being
Emotional well-being is not just about managing stress—it’s about thriving in all aspects of life. By prioritizing self-management emotional intelligence, you can cultivate resilience, enhance decision-making, and improve your overall quality of life. Throughout this article, we’ve explored the causes of emotional imbalance, the power of emotional self-management, and the science-backed tools like biofeedback and neurofeedback that can help you take control of your emotions.
Now, let’s wrap up with key insights and actionable next steps.
Why Prioritizing Self-Management Emotional Intelligence Transforms Lives
Developing self-management emotional intelligence isn’t just a personal goal—it’s a transformational skill that affects every area of your life:
✅ Better Decision-Making – Emotional clarity leads to smarter choices in personal and professional life.
✅ Stronger Relationships – Managing your emotional responses fosters healthier communication and deeper connections.
✅ Improved Mental and Physical Health – Reducing emotional imbalance lowers stress, improves sleep, and enhances overall well-being.
✅ Higher Performance and Productivity – Emotional regulation boosts focus, motivation, and resilience, whether in academics, sports, or the workplace.
When you take charge of your emotions, you don’t just react to life—you actively shape it to align with your goals and values.
FAQ - Emotional Balance vs Emotional Imbalance
Emotional balance is the ability to experience a full range of emotions without being overwhelmed by them. It enables you to handle stress effectively, make rational decisions, maintain healthy relationships, and enhance your focus. According to the article, emotional imbalance can lead to burnout, poor decision-making, and physical health issues, making emotional balance crucial for overall well-being.
Self-management emotional intelligence is a key component of emotional intelligence (EQ) that involves the ability to regulate your emotions in a way that supports well-being and decision-making. It enables you to stay calm under pressure, reduce stress, improve focus, and strengthen relationships by responding thoughtfully instead of reacting impulsively.
Biofeedback is a science-backed approach that utilizes devices to provide real-time data on physiological signals, such as heart rate, brain activity, and skin conductivity. This feedback helps individuals consciously regulate these responses, thereby enhancing emotional control, reducing stress-related symptoms such as anxiety, and fostering long-term emotional resilience.
- For cognitive and emotional control: Mendi Headband (Neurofeedback)
- For brainwave entrainment: NeuroVizr (Light and Sound)
- For heart rate-based training: HeartMath (HRV Biofeedback)
- For stress detection: BioSignals 5 sensor device (HRV, Temperature, GSR, and Breathing Biofeedback)
- Pause and Breathe: Take a deep breath and count to five before reacting.
- 4-7-8 Breathing: Inhale for 4 seconds, hold for 7, exhale for 8 to activate calm.
- Cognitive Reframing: Ask yourself if there’s another way to interpret the situation to reduce distress.
Your Next Steps to Achieve Lasting Emotional Balance
Ready to take control of your emotional well-being? Here’s a roadmap to get started:
Step 1: Start Tracking Your Emotional Patterns
📌 Why? Awareness is the first step to change.
✅ Keep an emotional journal to track your triggers and responses.
✅ Use biofeedback devices (HRV, GSR, Mendi Headband) to monitor stress and emotional fluctuations.
Step 2: Implement Daily Emotional Self-Management Techniques
📌 Why? Small habits lead to long-term transformation.
✅ Practice breathwork and relaxation techniques (BioSignals 5 sensor device, HeartMath HRV training).
✅ Incorporate mindfulness and meditation (with NeuroVizr for enhanced focus).
✅ Apply CBT strategies to shift negative thinking patterns and reframe stressors.
Step 3: Train Your Brain with Biofeedback
📌 Why? Biofeedback strengthens emotional resilience by optimizing brain function.
✅ Use the Mendi Headband to improve emotional regulation and mental clarity.
✅ Practice GSR and thermal biofeedback to train your stress response.
✅ Experiment with light and sound neurofeedback (NeuroVizr) for deeper relaxation.
Step 4: Stay Consistent and Measure Progress
📌 Why? Long-term success requires consistency.
✅ Set reminders to practice biofeedback, mindfulness, and emotional reflection daily.
✅ Regularly assess your emotional resilience and progress through self-check-ins.
✅ Join communities or programs focused on emotional well-being for support and motivation.
Final Thought: Take the First Step Today!
Emotional mastery doesn’t happen overnight, but each small step brings you closer to lasting balance and control. Whether you start by practicing mindfulness, using biofeedback, or applying CBT techniques, the key is to take action.
Your emotional well-being is in your hands—embrace the journey and start building the balanced, resilient life you deserve!