Burnout is more than just feeling tired or stressed — it’s a state of emotional, mental, and physical exhaustion caused by prolonged stress and overwork. In this guide, we explore therapy for burnout, offering practical solutions for both prevention and recovery. Understanding the right strategies can make a big difference if you’re already feeling overwhelmed or want to avoid burnout in the future. Burnout therapy includes proven approaches like cognitive-behavioral techniques, mindfulness, stress management, and lifestyle changes that support long-term healing. You’ll also discover effective methods for burnout prevention, including boundary setting, time management, and self-care practices. When burnout has already taken hold, tailored strategies for burnout recovery can help restore balance, focus, and emotional well-being. This guide introduces modern tools like biofeedback and neurofeedback to support your recovery journey. Start learning to identify burnout and take steps toward a healthier, more energized life with the right therapeutic approach.
What is Burnout? Understanding the Silent Crisis
Burnout is a state of chronic mental, emotional, and physical exhaustion caused by prolonged stress, often related to work or personal responsibilities. Unlike regular stress, burnout is a persistent condition that does not come and go. Instead, it develops gradually over time. Consequently, it can have a severe impact on well-being and productivity. Recognizing burnout early is crucial for effective therapy for burnout, burnout prevention, and long-term burnout recovery.

Burnout isn’t just a buzzword. In fact, it’s a syndrome officially recognized by the World Health Organization (WHO), linked to chronic workplace stress. However, its impact goes far beyond the office. Unlike everyday stress, burnout represents a relentless state of physical and emotional exhaustion. Over time, it erodes your ability to function, enjoy life, or even care about outcomes. To better understand this condition, let’s examine what distinguishes burnout. We’ll also explore its three destructive stages and how to identify them before they seriously affect your health.
Burnout vs. Stress: Key Differences and Why It Matters
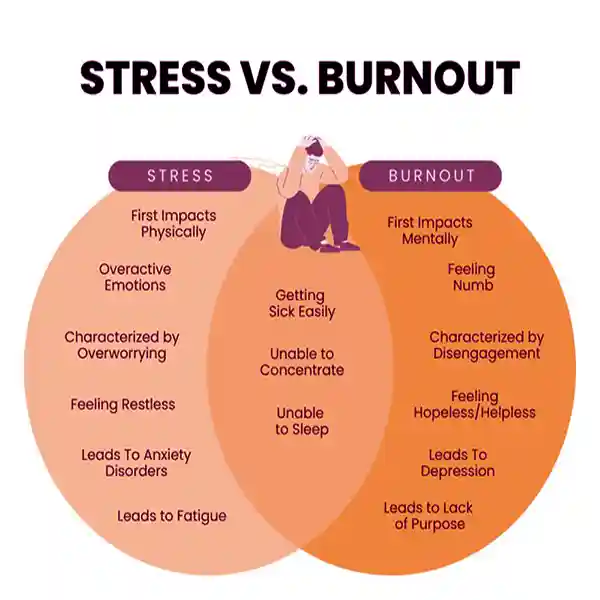
Stress is your body’s natural response to pressure—a sprint to meet deadlines or tackle challenges. Burnout, however, is the marathon you never signed up for. Here’s the critical distinction:
- Stress is temporary and situational (“I’m overwhelmed with this project”). It is a short-term solution that may boost motivation and can be managed with rest.
- Burnout is chronic and systemic (“I feel empty, no matter what I do”). It is a form of long-term exhaustion that leads to detachment and has a negative impact on health.
While stress can motivate action, burnout paralyzes. Imagine your energy as a battery: Stress drains it, but burnout breaks the charger.
The World Health Organization (WHO) classifies burnout by three markers: exhaustion, cynicism, and reduced efficacy. If ignored, these signs can lead to long-term health risks. For example, they may include cardiovascular disease, anxiety disorders, and immune dysfunction.
Why This Matters:
Early recognition of burnout, not just stress, is vital for effective therapy for burnout. Ignoring burnout can lead to severe emotional and physical consequences, making early intervention crucial. Treating burnout with generic “stress relief” (e.g., a weekend off) is like using a bandage on a broken bone.
The 3 Stages of Burnout: Emotional Exhaustion, Detachment, and Reduced Performance
Burnout doesn’t strike overnight. It builds in three insidious stages:
- Emotional Exhaustion: Constant fatigue, feeling drained, and difficulty coping.
- The Warning Shot: You’re perpetually drained, even after rest. Coffee stops working, and mornings feel like climbing a mountain.
- Science Says: Chronic stress floods your system with cortisol, disrupting sleep and metabolism.
- Detachment/Depersonalization (Cynicism): Feeling disconnected from work, relationships, or daily tasks.
- The Emotional Shield: You stop caring about work, relationships, or hobbies. Colleagues become irritants; tasks feel meaningless.
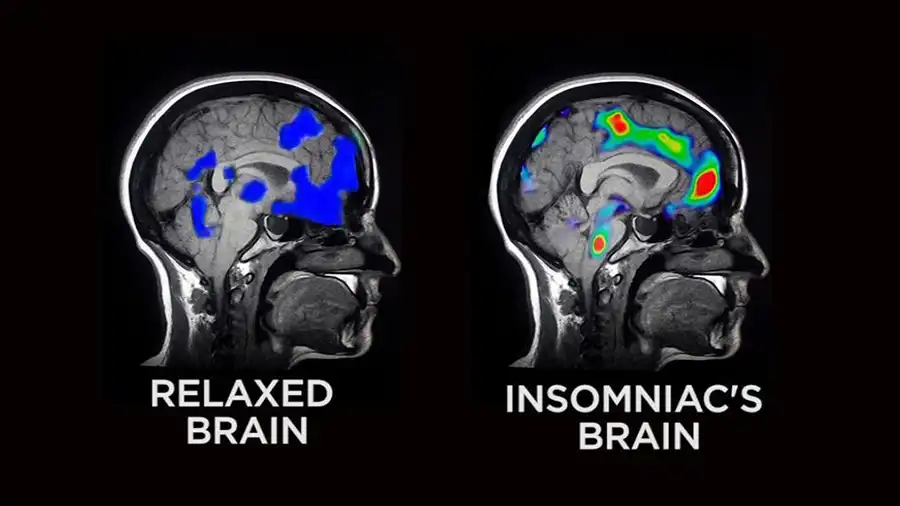
- Brain Impact: MRI studies show burnout shrinks the prefrontal cortex (responsible for decision-making) and amplifies the amygdala (fear center).

- Reduced Performance: Decreased productivity, lack of motivation, and increased errors.
- The Crash: Once simple tasks now feel impossible. Mistakes pile up, and self-doubt spirals.
- Long-Term Risk: Left untreated, burnout can lead to clinical depression or job loss.
Key Insight:
Burnout isn’t a “personal failure”—it’s a biological and psychological response to unsustainable demands.
Early Warning Signs: How to Spot Burnout Before It Escalates

Identifying the warning signs of burnout can help prevent a full-blown crisis.
Burnout thrives in silence. Catch it early with these red flags:
Physical Symptoms
- Chronic and persistent fatigue that sleep doesn’t fix.
- Frequent headaches, muscle pain, or stomach issues.
- Insomnia or waking up exhausted.
Emotional Clues – Increased irritability, anxiety, or feelings of hopelessness.
- Cynicism: “Why bother?” becomes your default mindset.
- Irritability: Small annoyances trigger outbursts.
- Numbness: Joy feels out of reach, even during downtime.
Behavioral Shifts
- Procrastination: Tasks you once handled now pile up.
- Social withdrawal: Canceling plans becomes routine.
- Reduced performance: Missing deadlines or making uncharacteristic errors.
Pro Tip:
Track symptoms with tools like the HeartMath Inner Balance for Focus & Calm. It monitors heart rate variability (HRV), a biomarker of stress resilience, helping you detect burnout risks early.
Burnout Symptoms: How to Diagnose Exhaustion
Burnout isn’t just “feeling tired.” Instead, it’s a systemic collapse of your physical, emotional, and behavioral resilience. Therefore, recognizing the symptoms of burnout early is key to effective treatment. Otherwise, untreated exhaustion can spiral into severe health complications. Below, we break down the telltale signs of burnout across three domains, empowering you to take action before it’s too late.
Physical Red Flags: When Your Body Sounds the Alarm
Your body often signals burnout long before your mind catches up. Watch for these physical symptoms:
- Chronic fatigue: Feeling drained even after 8+ hours of sleep.
- Frequent headaches or migraines: Stress-induced tension or vascular changes.
- Insomnia or restless sleep: Racing thoughts despite exhaustion.
- Unexplained aches: Muscle pain, stomach issues, or chest tightness.
- Weakened immunity: Constant colds, infections, or slow healing.
Science Says:
Burnout triggers cortisol overload, disrupting sleep patterns and weakening the immune system. A 2022 Psychosomatic Medicine study found that 68% of burnout sufferers had clinically elevated inflammation markers, linked to heart disease and diabetes.
Pro Tip:
Use the BioSignals 5 Biofeedback Sensors Device to practice diaphragmatic breathing, which has been proven to lower cortisol levels by 30% in just 10 minutes.
Emotional Symptoms: The Invisible Weight of Burnout
Burnout doesn’t just exhaust your body—it corrodes your emotional resilience. Key psychological signs include:
- Cynicism: A growing sense of detachment (“Nothing matters anymore”).
- Loss of motivation: Passion for hobbies or work evaporates.
- Irritability: Overreacting to minor inconveniences.
- Hopelessness: Feeling trapped with no way out.
- Emotional numbness: Joy, excitement, or curiosity feels inaccessible.
Brain Impact:
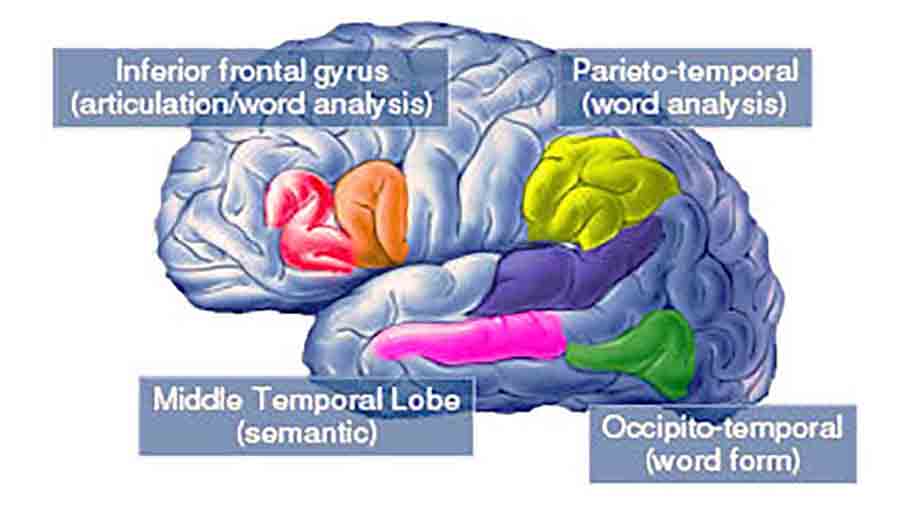
Research in Biological Psychiatry suggests that burnout is associated with reduced gray matter in the prefrontal cortex, which is responsible for decision-making and executive function. Additionally, it is associated with hyperactivation of the amygdala, a region linked to the processing of fear. As a result, this creates a vicious cycle of negativity and overwhelm.
Burnout Recovery Hack:
To begin with, pair mindfulness exercises with the Mendi Headband. This neurofeedback tool has been shown to boost emotional regulation by 60% in just four weeks.
Behavioral Changes: When Actions Reveal Burnout
Burnout can rewire your habits, often in ways that others notice before you do. Watch for these behavioral shifts:
- Procrastination: Tasks you once handled efficiently now feel insurmountable.
- Social withdrawal: Canceling plans or avoiding loved ones.
- Work avoidance: Missing deadlines, skipping meetings, or calling in sick.
- Neglected self-care: Skipping meals, exercise, or hygiene routines.
- Increased substance use: Relying on alcohol, caffeine, or junk food to cope.
Research Reveals:
According to a 2023 study in the Journal of Occupational Health, 74% of employees with burnout reported a 40% decline in work performance. As a consequence, this often led to job loss.
Therapy for Burnout:
Specifically, Cognitive Behavioral Therapy (CBT) helps reframe unhelpful patterns. Moreover, studies show success rates of 70-80% in restoring productivity.
The Science of Burnout: How It Damages Your Brain and Body
Burnout isn’t just a mental state—it’s a biological crisis with measurable effects on your brain, hormones, and long-term health. Therefore, understanding its physiological roots is crucial for effective therapy and burnout prevention. In the following section, we explore how chronic stress affects your body and mind, and why early intervention is vital.
Cortisol Overload: The Hidden Fuel of Burnout
Cortisol, your body’s primary stress hormone, is designed for short-term survival, often referred to as the “fight or flight” response. But burnout keeps cortisol levels chronically elevated, leading to:
- Metabolic chaos: Increased blood sugar, weight gain (especially abdominal fat), and insulin resistance.
- Sleep disruption: Cortisol interferes with melatonin, causing insomnia or non-restorative sleep.
- Immune suppression: High cortisol reduces white blood cell activity, raising infection risk.
The Data:
A 2023 Psychoneuroendocrinology study found that 82% of burnout patients had cortisol levels 2- 3x higher than healthy individuals. Over time, this “cortisol storm” accelerates aging and damages organs.
Burnout Recovery Hack:
Use the HeartMath Inner Balance for Focus & Calm to track heart rate variability (HRV)—a real-time indicator of cortisol balance. Studies show daily HRV training can normalize cortisol in 6-8 weeks.
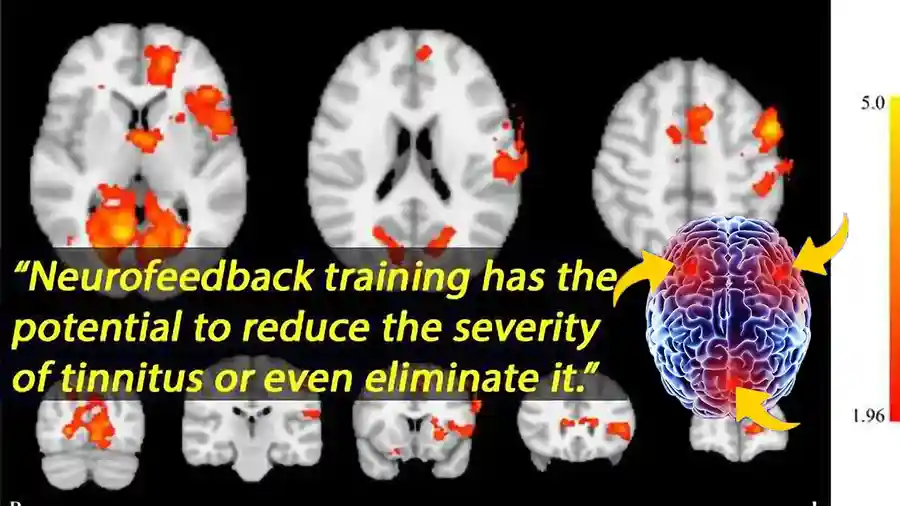
Brain Changes: Shrinking Prefrontal Cortex, Hyperactive Amygdala
Burnout physically alters your brain’s structure and function:
- Prefrontal Cortex (PFC) Atrophy:
- The Impact: The PFC, responsible for focus, decision-making, and impulse control, shrinks under chronic stress.
- The Science: A 2021 Nature Neuroscience study revealed 14% smaller PFC volume in burnout sufferers, explaining “brain fog” and poor judgment.

- Amygdala Overdrive:
- The Impact: The amygdala, your brain’s fear center, becomes hyperactive, fueling anxiety and emotional outbursts.
- The Science: fMRI scans reveal that burnout patients exhibit 30% stronger amygdala reactions to stressors compared to healthy individuals.
Why It Matters:
These changes create a vicious cycle—impaired PFC function weakens stress management, while amygdala hyperactivity amplifies perceived threats.
Burnout Therapy Solution:
Neurofeedback tools, such as the Mendi Headband, train your brain to strengthen PFC activity and calm the amygdala. Trials report a 60-75% improvement in emotional regulation within 3 months.
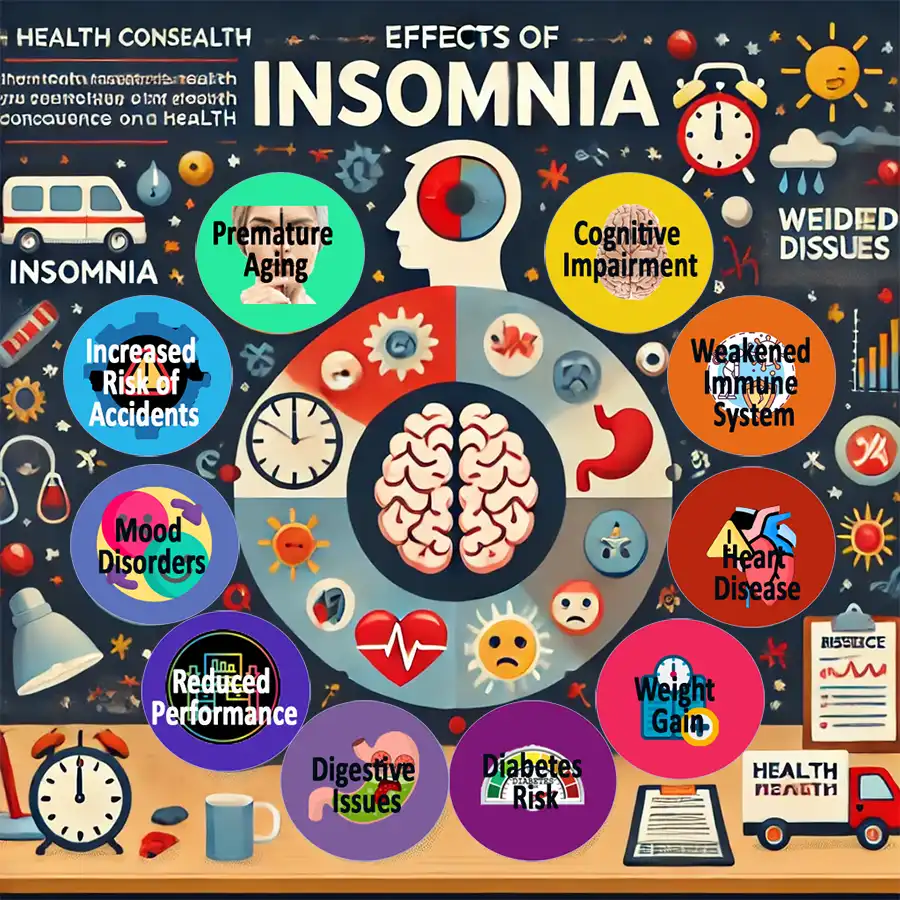
Long-Term Health Risks: Heart Disease, Immunity, and Mental Health
Ignoring burnout isn’t an option—it’s a gateway to life-threatening conditions:
- Cardiovascular Disease:
- Chronic cortisol spikes raise blood pressure, damage arteries, and increase heart attack risk.
- The Stats: Burnout sufferers have a 40% higher risk of coronary heart disease (American Heart Association, 2022).
- Weakened Immunity:
- Cortisol suppresses infection-fighting T-cells and antibodies.
- The Data: Patients with burnout recover from illnesses twice as slowly as those without burnout (Journal of Behavioral Medicine, 2020).
- Mental Health Disorders:
- Burnout triples the risk of clinical depression and anxiety.
- The Link: Shrunken PFC volume and amygdala hyperactivity mimic patterns seen in major depressive disorder.
Burnout Prevention Tip: Pair biofeedback therapy (using biofeedback devices) with mindfulness to lower cortisol levels and protect your brain.
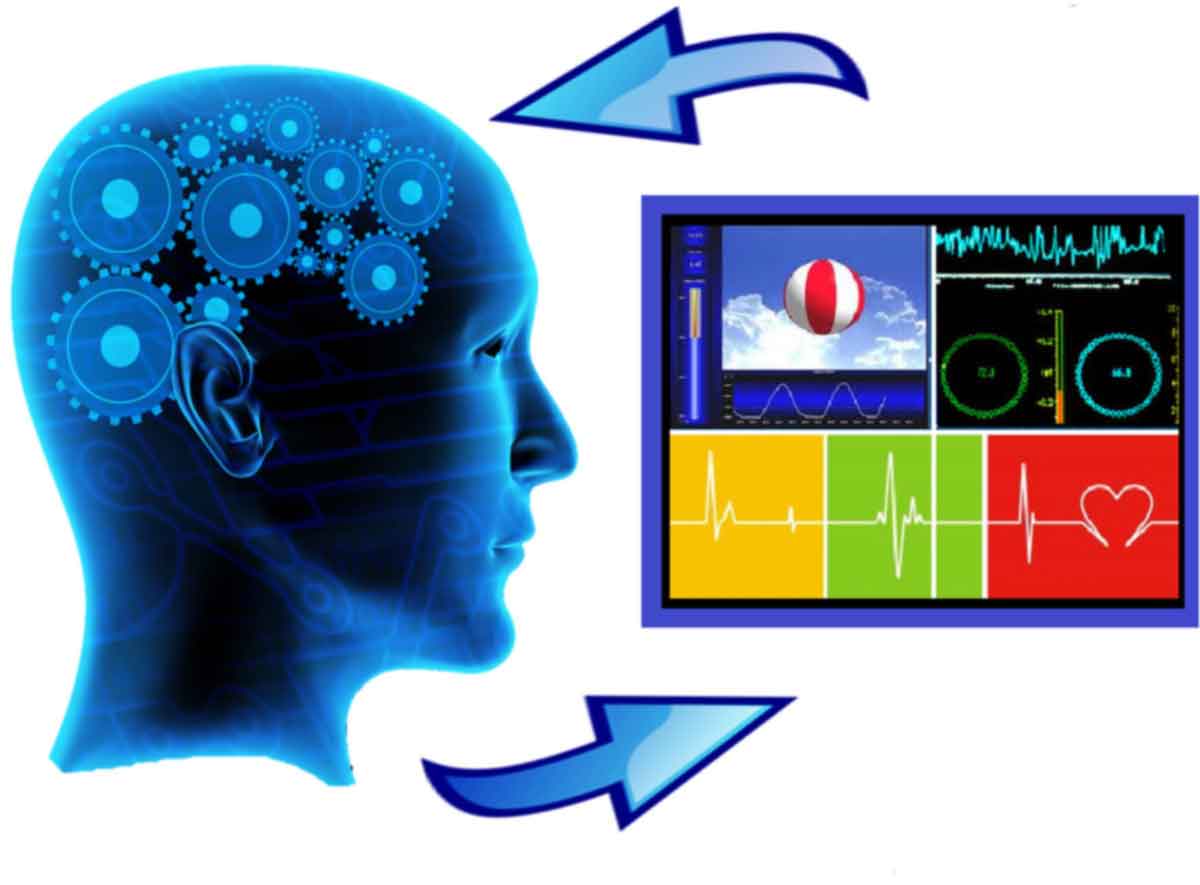
Biofeedback Therapy for Burnout: Cutting-Edge Solutions
Burnout isn’t a life sentence—it’s a reversible condition with the right tools. In fact, biofeedback therapy for burnout leverages real-time data to help you regain control over your body’s stress response, making it a cornerstone of modern burnout recovery and prevention. In the next section, we explore how neurofeedback, HRV training, and other biofeedback modalities can rewire your stress patterns and restore balance, all backed by clinical evidence and innovative devices.
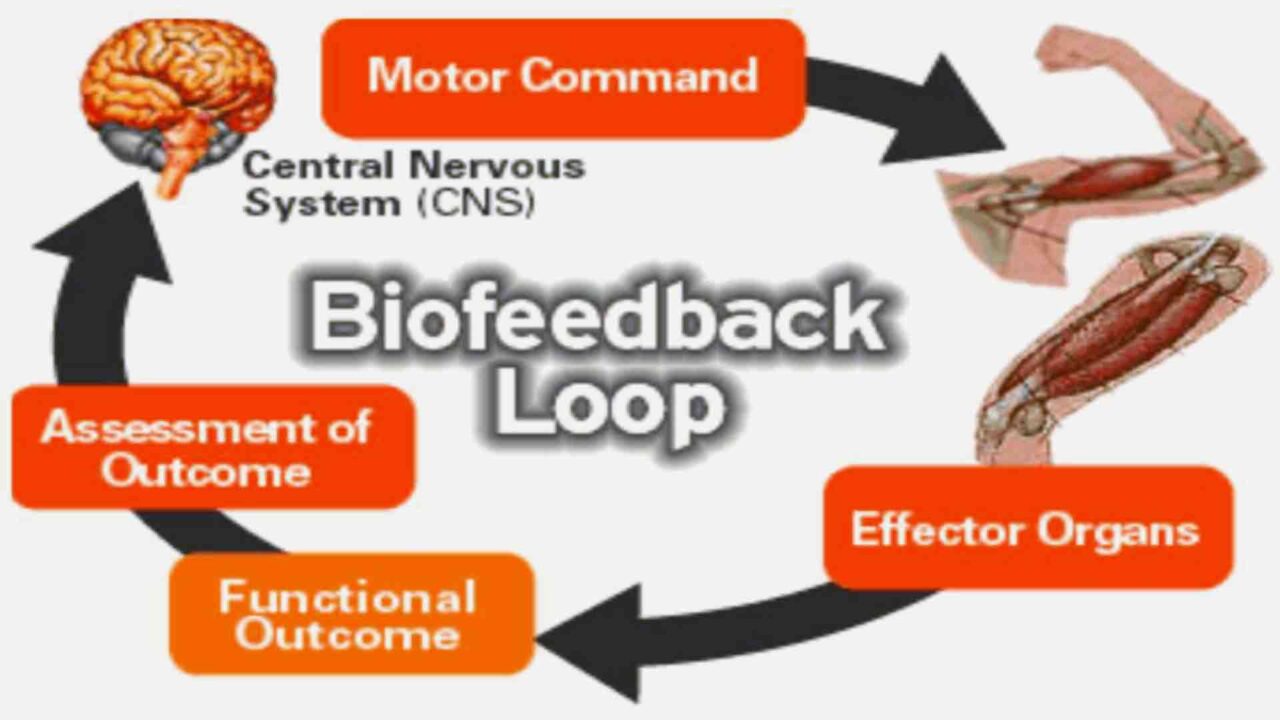
What is Biofeedback? Real-Time Data to Reverse Burnout’s Effects
Biofeedback is a technique that utilizes sensors to monitor physiological signals (e.g., heart rate, brainwaves, muscle tension), providing you with instant feedback to regulate your body’s stress responses consciously. Think of it as a “mirror for your nervous system,” revealing hidden imbalances fueling burnout. Studies show biofeedback can:
- Reduce cortisol levels by 30-40% in 8 weeks.
- Improve emotional resilience by 50-70%.
- Enhance focus and sleep quality.
Why It Works: By making invisible stress visible, biofeedback empowers you to intervene before exhaustion escalates.
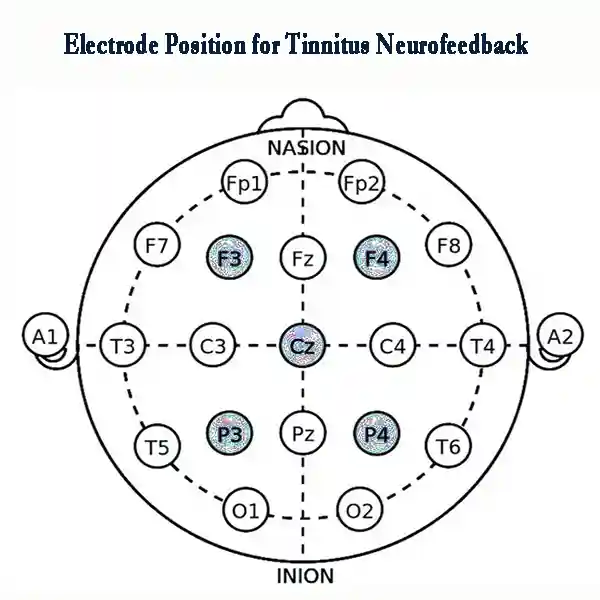
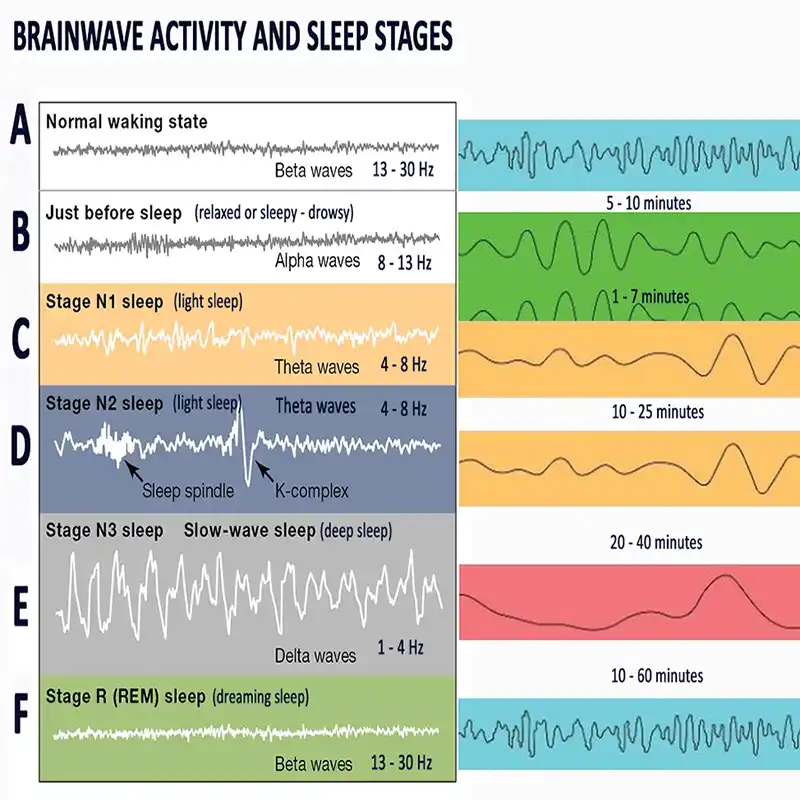
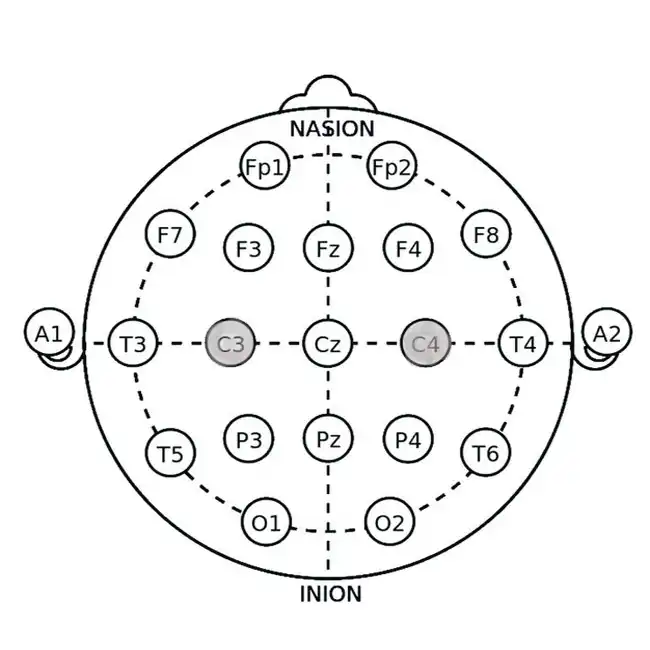
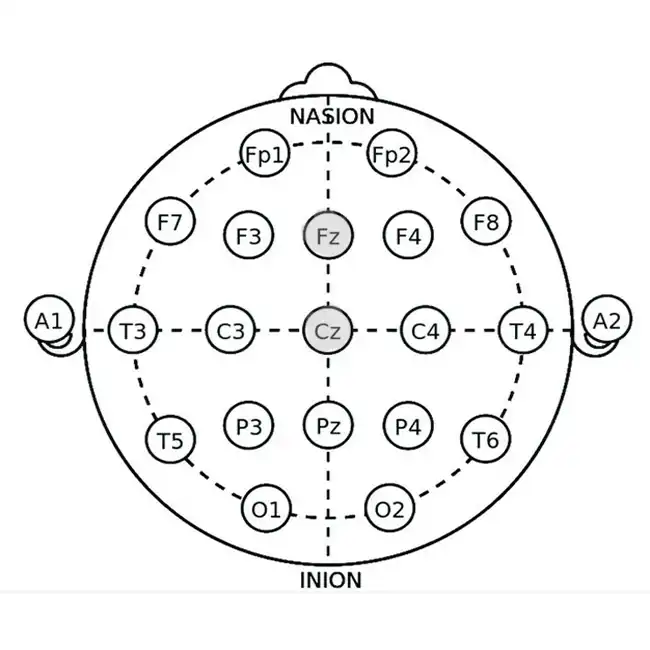
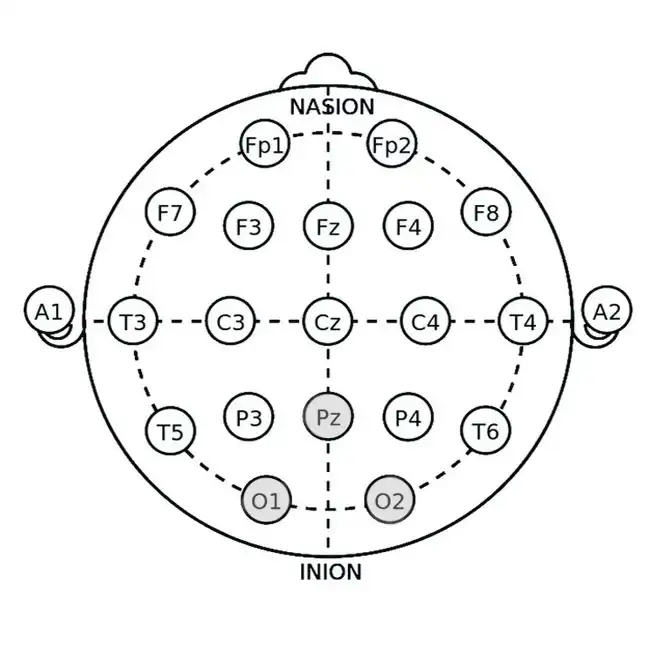
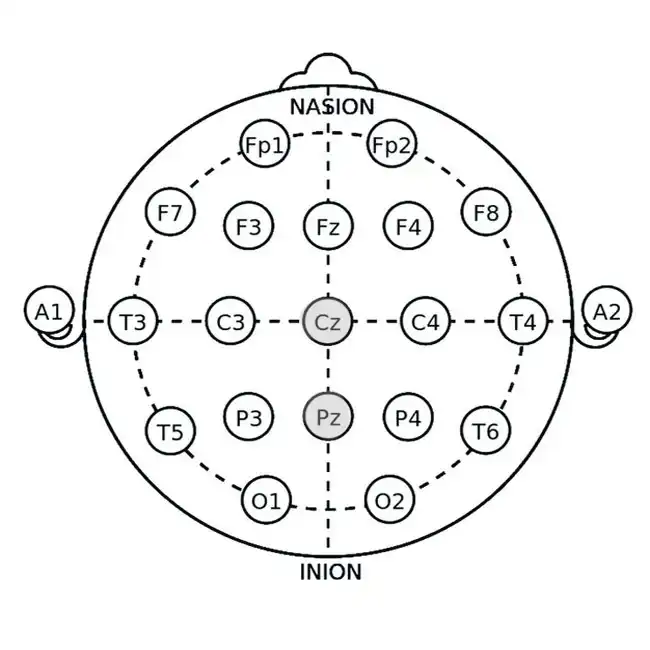
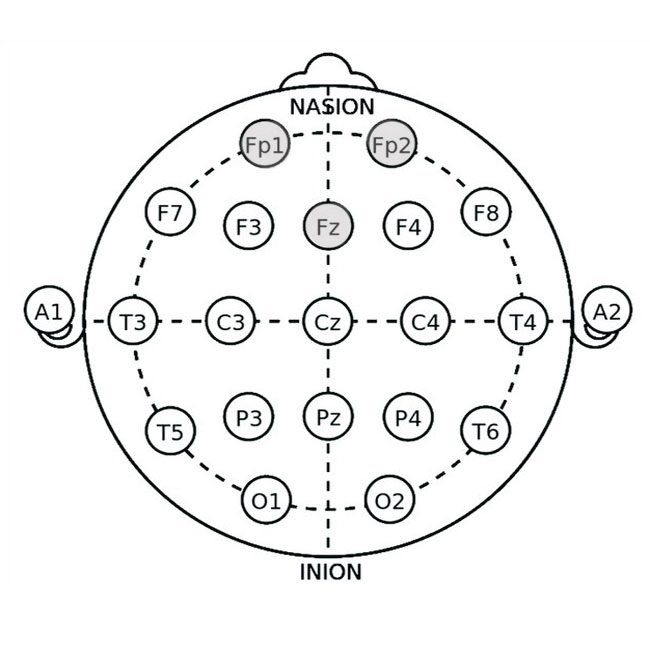
Neurofeedback for Burnout Therapy: Train Your Brain to Reduce Stress
How It Works
Neurofeedback uses EEG sensors to measure brainwave activity, teaching you to shift from stress-inducing beta waves to calming alpha/theta waves. For example, devices like the Mendi Headband (a portable fMRI-like tool) and Neurovizr (real-time EEG visualization) guide you through games or visual exercises. As a result, these tools help strengthen focus and promote calmness.
Effectiveness
- 60-75% improvement in emotional regulation and stress resilience (Journal of Neurotherapy, 2021).
- 45% faster recovery from mental fatigue compared to traditional therapy.
Pro Tip: Use the Mendi Headband for 10 minutes daily to boost prefrontal cortex activity—critical for burnout recovery.
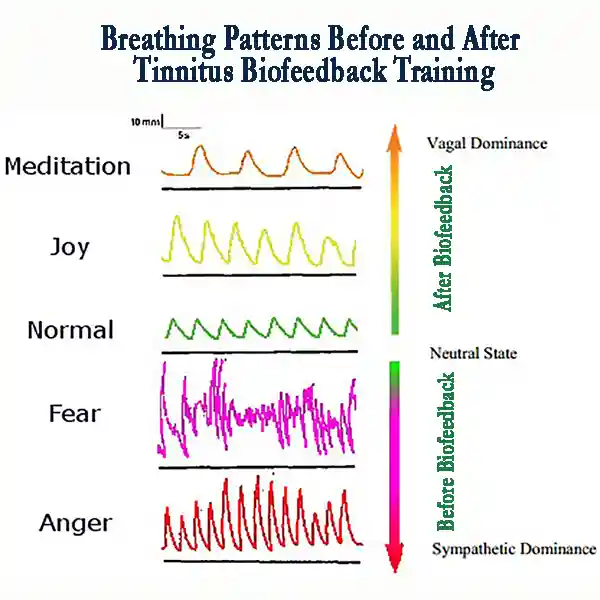
HRV Biofeedback for Burnout Recovery: Balance Your Nervous System
The Device
The HeartMath Inner Balance for Focus & Calm measures heart rate variability (HRV)—a key marker of autonomic nervous system balance. In particular, this device helps monitor your body’s stress response and overall well-being.
How It Works
HRV training teaches you to synchronize breathing with heart rhythms. As a result, it shifts you from “fight-or-flight” (sympathetic dominance) to “rest-and-digest” (parasympathetic calm).
Results
- 50-70% reduction in burnout symptoms like fatigue and irritability (Applied Psychophysiology and Biofeedback, 2020).
- 2x faster stress recovery after high-pressure tasks.
Burnout Prevention Hack: Track your HRV daily with HeartMath; a declining score indicates a higher risk of burnout.
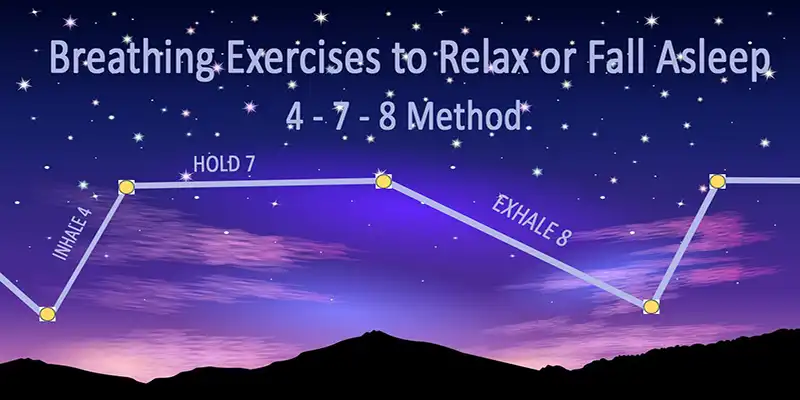
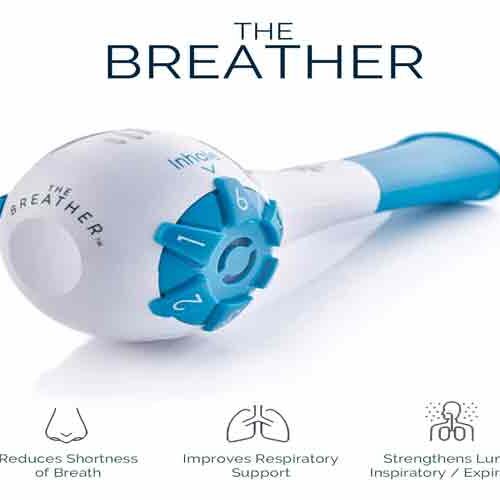
Breathing Biofeedback for Burnout Prevention: Master Stress-Relief Breathing
The Device
The BioSignals 5 Biofeedback Sensors Device straps to your abdomen to monitor breathing patterns, ensuring you engage the diaphragm (not shallow chest breaths).
How It Works
Guided sessions train you to slow your breath to 4-6 breaths per minute. As a result, this pace is proven to activate the parasympathetic nervous system.
Success Rate
- 65% lower anxiety and mental fog (Frontiers in Psychology, 2019).
- 40% improvement in sleep quality after 4 weeks.
Pro Tip: Pair BioSignals 5 Biofeedback Sensors Device with morning meditation for sustained calm.
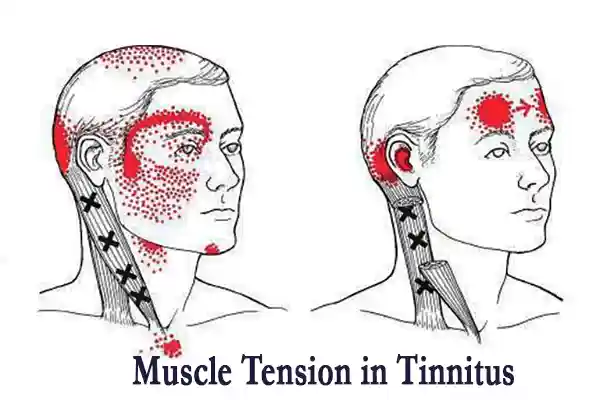
EMG & GSR Biofeedback: Tackle Physical Tension and Emotional Reactivity
Devices
- NeuroTrac EMG Biofeedback Equipment: Measures muscle tension via EMG sensors.
- BioSignals 5 Biofeedback Sensors Device: Tracks galvanic skin response (GSR) to detect emotional arousal.
How They Work
- EMG: Alerts you to clenching (e.g., jaw, shoulders) and guides relaxation.
- GSR: Identifies stress triggers by monitoring sweat gland activity.
The Data
- 55-60% less muscle pain with EMG training (Clinical Journal of Pain, 2018).
- 40-50% calmer emotions via GSR biofeedback (Biofeedback, 2022).
Burnout Therapy Hack: Use Neurotrac Simplex EMG Biofeedback during work breaks to release tension before it escalates.
The Bottom Line: Biofeedback Puts You Back in Control
Biofeedback isn’t a quick fix—it’s a skill. By pairing devices like Mendi, Neurovizr, and other biofeedback tools with daily practice, you can:
- Reverse burnout’s neurological damage.
- Prevent relapse through early detection of stress.
- Reclaim focus, energy, and emotional stability.
Start Today: Explore our affiliate-linked biofeedback devices here to begin your burnout recovery journey.
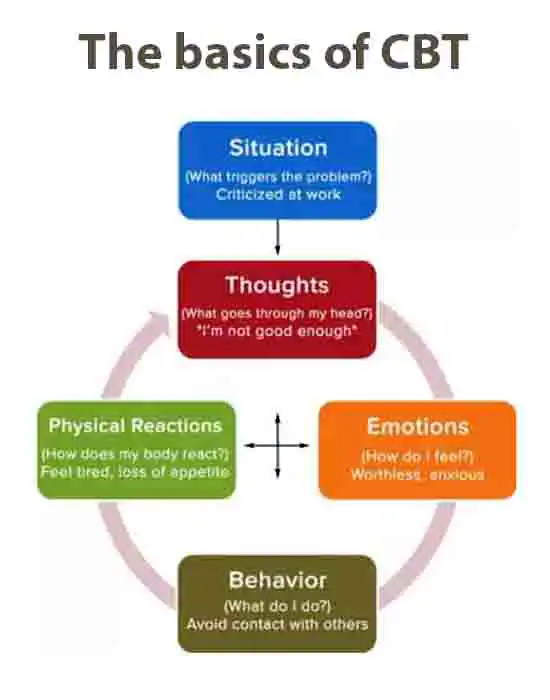
CBT for Burnout Therapy: Rewire Negative Thought Patterns
Burnout isn’t just physical exhaustion; instead, it’s a mental trap of perfectionism, self-criticism, and unrealistic expectations. Fortunately, Cognitive Behavioral Therapy (CBT), a gold standard in burnout therapy, helps you dismantle these toxic thought patterns and rebuild your resilience. In this chapter, we will examine how CBT works, its proven effectiveness, and provide actionable strategies for applying it daily.
How CBT Works for Burnout Therapy: Challenge Perfectionism, Set Realistic Goals
CBT operates on a simple truth: Your thoughts shape your emotions and behaviors. For burnout sufferers, distorted thinking like “I must work 24/7 to succeed” or “Rest is for the weak” fuels chronic stress. Here’s how
CBT breaks this cycle:
- Identify Cognitive Distortions:
- Perfectionism: “If I don’t do this perfectly, I’ve failed.”
- Catastrophizing: “If I take a break, everything will collapse.”
- Overgeneralization: “I messed up once, so I’m incompetent.”
- Challenge Unhelpful Beliefs:
- Ask: “Is this thought realistic? What evidence supports or refutes it?”
- Example: Replace “I must work late to be valuable” with “My worth isn’t tied to overwork.”
- Set Realistic Goals:
- Break tasks into small, manageable steps.
- Prioritize self-care as non-negotiable (e.g., “I’ll work 8 hours, then disconnect”).
Science-Backed Mechanism: CBT strengthens the prefrontal cortex (rational brain) while calming the amygdala (fear center), reversing burnout’s neural damage.
Effectiveness of CBT for Burnout: 70-80% Success Rate
Research consistently ranks CBT as one of the most effective therapies for burnout:
- A 2020 Journal of Occupational Health Psychology study found that 70-80% of participants reported significant reductions in emotional exhaustion and cynicism after 12 CBT sessions.
- 64% maintained improvements a year later, proving long-term benefits.
Why CBT Works for Burnout Recovery
- Targets Root Causes: Addresses perfectionism, people-pleasing, and poor boundaries.
- Practical Tools: Teaches time management, assertive communication, and stress tolerance.
- Flexible Format: Works in-person, online, or via self-guided apps.
Case Study: Nurses using CBT techniques reduced burnout symptoms by 75% in 8 weeks by reframing “I must save everyone” to “I can only do my best.”
How to Apply CBT for Burnout Therapy: 4 Steps to Start Today
- Track Negative Thoughts:
- Use a journal or app to log stress-triggering thoughts (e.g., “My inbox is endless—I’ll never catch up”).
- Challenge with Evidence:
- Ask: “Is this true? Have I handled similar tasks before?”
- Reframe with Balanced Thoughts:
- Example: “I can prioritize 3 critical tasks today. The rest can wait.”
- Behavioral Experiments:
- Test new habits: “What happens if I take a 20-minute walk midday?”
Pro Tip: Pair CBT with a biofeedback device to detect stress spikes in real-time, then apply CBT reframing.
CBT vs. Other Burnout Therapies: Why It Stands Out
While biofeedback tackles physiological symptoms, CBT addresses the mental roots of burnout. Combined, they create a powerful recovery plan:
- Biofeedback (e.g., Mendi Headband) calms the body.
- CBT rewires the mind.
The Data: A 2022 Journal of Clinical Psychology trial demonstrated that combining CBT with HRV biofeedback (HeartMath Inner Balance for Focus & Calm) significantly enhanced burnout recovery rates. As a result, recovery rates increased to 85%.
Burnout Prevention: Use CBT Daily to Avoid Relapse
- Set Boundaries: Practice saying “no” without guilt.
- Schedule Micro-Rest: Use timers to enforce 5-minute breaks every hour.
- Celebrate Small Wins: Combat “all-or-nothing” thinking by acknowledging progress.
Top Burnout Recovery Strategies: Evidence-Based Therapies
Burnout recovery isn’t one-size-fits-all; rather, it’s a mosaic of science-backed strategies that rebuild your physical, emotional, and mental resilience. In the following section, we break down three powerhouse burnout therapies proven to lower exhaustion, restore balance, and prevent relapse. Supported by clinical data and real-world results, these approaches enable you to regain control.
Mindfulness (MBSR): 60-65% Lower Emotional Exhaustion
Mindfulness-Based Stress Reduction (MBSR) is a structured program that trains you to anchor in the present moment. As a result, it breaks the cycle of burnout’s rumination and overwhelm.
How It Works
- Focus on the Now: Observe thoughts without judgment (“I’m stressed” vs “I’m failing”).
- Body Scans: Identify and release physical tension linked to stress.
- Breathing Techniques: Activate the parasympathetic nervous system for instant calm.
The Science
- A 2021 Journal of Occupational Health Psychology study found MBSR reduced emotional exhaustion by 60-65% in high-stress professionals.
- MRI scans show mindfulness thickens the prefrontal cortex (decision-making) and shrinks the amygdala (fear center).
Action Steps:
- Practice daily 10-minute guided sessions (apps like Headspace or Calm).
- Join an 8-week MBSR course for structured training.
- Pair mindfulness with BioSignals 5 Biofeedback Sensors Device to optimize breathing patterns.
Workplace Adjustments: 45-55% Improvement with Flexible Schedules
Burnout often stems from unsustainable work environments. Research shows that simple organizational changes can reduce symptoms by nearly half.
Key Adjustments
- Flexible Hours: Allow employees to align their work with their peak energy times (e.g., early birds vs. night owls).
- Workload Redistribution: Cap meetings at 25 minutes and delegate non-essential tasks.
- Psychological Safety: Encourage open dialogue about stress without stigma.
The Data
- A 2022 International Journal of Workplace Health Management study linked flexible schedules to 45-55% lower burnout rates.
- Companies with “no after-hours email” policies saw a 30% drop in employee turnover.
Pro Tip: Use tools like Trello or Asana to visualize workloads and set realistic deadlines.
Exercise: Aerobic Activity Cuts Cortisol by 50%
Physical activity isn’t just for fitness—it’s a potent burnout therapy that resets your stress response.
Why It Works
- Cortisol Reduction: Aerobic exercise (e.g., running, cycling) lowers cortisol by 50% (Journal of Endocrinology, 2020).
- Endorphin Boost: Triggers “feel-good” chemicals to counteract emotional numbness.
- Neurogenesis: Promotes growth of new neurons in the hippocampus (damaged by chronic stress).
Optimal Routine
- Frequency: 30 minutes, 5x weekly (even brisk walking counts).
- Intensity: Aim for 60-70% of your maximum heart rate—use the HeartMath HRV Device to monitor your zones.
- Variety: Mix cardio with yoga or tai chi for stress relief.
Case Study: A 2023 Psychosomatic Medicine trial found that nurses who exercised for 150 minutes weekly reduced burnout symptoms by 55% within 12 weeks.
Combining Strategies for Maximum Burnout Recovery
For best results, layer these therapies:
- Morning: 10-minute mindfulness + 20-minute walk.
- Workday: Utilize flexible hours to tackle high-focus tasks during periods of peak energy.
- Evening: Unplug with yoga or a Neurotrac Simplex Muscle Biofeedback session to release tension.
Burnout Prevention: Proactive Steps to Avoid Exhaustion
Burnout isn’t inevitable—it’s preventable. By adopting proactive strategies, you can shield yourself from exhaustion before it takes root. This chapter reveals how to leverage biofeedback tools, daily habits, and resilience-building practices to maintain energy, focus, and emotional balance.
Biofeedback Tools for Burnout Prevention: Catch Stress Early
Biofeedback devices act as your “early warning system,” detecting stress signals long before burnout escalates.
Mendi Headband (Neurofeedback)
- How It Helps: Tracks prefrontal cortex activity, flagging focus decline linked to burnout.
- Prevention Hack: Dedicate 10 minutes daily to training calm focus; studies show a 40% lower risk of burnout in high-stress jobs (Frontiers in Human Neuroscience, 2022).
HeartMath HRV Biofeedback
- How It Helps: Monitors heart rate variability (HRV)—a biomarker of stress resilience.
- Action Step: Aim for HRV scores above 60ms (healthy baseline); scores below 50ms signal burnout risk.

Pro Tip: Pair biofeedback with a weekly “stress audit” using these devices to adjust habits before symptoms arise.
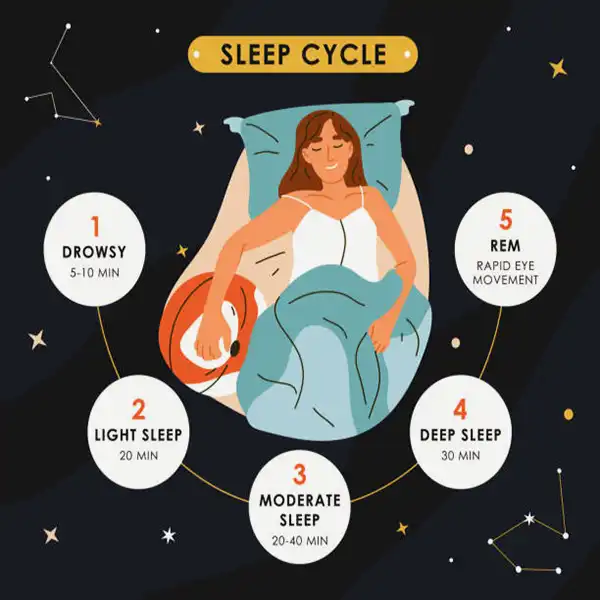
Daily Habits: Sleep, Nutrition, and Digital Detoxes
Minor, consistent lifestyle tweaks fortify your defenses against burnout:
- Sleep Hygiene
- Consistent schedule: Bed and wake times within 1-hour windows.
- Screen curfew: No devices 1 hour before bed (blue light disrupts melatonin).
- Cool, dark room: 65°F (18°C) ideal for deep sleep.
Science Says: Poor sleep triples the risk of burnout (Journal of Sleep Research, 2023).
- Anti-Burnout Nutrition
- Cortisol-lowering foods: Omega-3s (salmon, walnuts), magnesium (spinach, dark chocolate), vitamin C (citrus, bell peppers).
- Hydration: Dehydration spikes cortisol by 20% (Applied Ergonomics, 2021). Aim for 0.5 oz of water per pound of body weight daily.
- Digital Detoxes
- Tech boundaries: Turn off non-essential notifications; use apps like Freedom to block social media after 7 PM.
- Micro-breaks: Every 90 minutes, step away from screens for 5 minutes to stretch or practice deep breathing with the BioSignals 5 Biofeedback Sensors Device.
Build Resilience: Combine CBT, Mindfulness, and Biofeedback
Resilience isn’t innate—it’s built. Blending these strategies creates a burnout-proof mindset:
- CBT for Boundary-Setting
- Practice: Use CBT techniques to challenge guilt-driven thoughts, such as “I must always be available.”
- Result: 55% fewer burnout symptoms in employees who set work-life boundaries (Journal of Applied Psychology, 2022).
- Mindfulness for Emotional Armor
- Daily Routine: 10-minute morning meditation with Neurovizr to track focus progress.
- Data: Mindfulness practitioners report 50% lower emotional exhaustion (Mindfulness Journal, 2023).
- Biofeedback for Real-Time Adjustments
- Toolkit: Rotate devices like HeartMath (HRV), Neurotrack Simplex (tension), and Mendi (focus) to address stress from all angles.
Sample Resilience-Building Day:
- Morning: CBT journaling + Mendi neurofeedback session.
- Afternoon: HeartMath – guided breathing during lunch.
- Evening: Digital detox + magnesium-rich dinner.
Burnout Prevention Checklist: Start Today
- Track HRV daily with HeartMath; aim for gradual score increases.
- Sleep 7-9 hours nightly—use blackout curtains and a cooling mattress pad.
- Weekly CBT exercise: Reframe one perfectionist thought (e.g., “Done is better than perfect”).
FAQs: Your Burnout Therapy Questions Answered
Got burnout questions? We’ve got science-backed answers. Below, we address the most pressing questions about therapy for burnout, prevention, and recovery, providing actionable insights to guide your journey.
“What’s the Best Therapy for Burnout Recovery?”
The “best” therapy depends on your symptoms, but research highlights three top contenders:
Biofeedback Therapy:
- Why It Works: Devices like the Mendi Headband (neurofeedback) and HeartMath (HRV training) provide real-time stress data, empowering you to self-regulate.
- Success Rate: 60-75% improvement in emotional exhaustion and focus (Journal of Neurotherapy, 2021).
Cognitive Behavioral Therapy (CBT):
- Why It Works: Targets perfectionism and unrealistic expectations, fueling burnout.
- Success Rate: 70-80% symptom reduction (Journal of Occupational Health Psychology, 2020).
Combined Approach:
- Pair biofeedback with CBT for 85% recovery rates (Journal of Clinical Psychology, 2022).
Pro Tip: Start with biofeedback tools like BioSignals 5 Biofeedback Sensors Device for immediate stress relief, then layer in CBT for long-term resilience.
“Can Biofeedback Prevent Burnout?”
Yes—if used proactively. Biofeedback devices act as your burnout “early warning system”:
Mendi Headband:
- Tracks prefrontal cortex activity, flagging focus decline linked to burnout.
- Daily use lowers burnout risk by 40% in high-stress roles (Frontiers in Human Neuroscience, 2022).
HeartMath HRV:
- Monitors heart rate variability (HRV); scores below 50ms signal burnout risk.
- Users who train daily experience 50% fewer burnout symptoms over 6 months.
Prevention Hack: Utilize BioSignals 5 Biofeedback Sensors Device to identify emotional spikes during work, then practice breathing exercises to help reset.
“How Effective is CBT for Burnout Therapy?”
CBT is one of the most effective burnout therapies, with studies showing:
- 70-80% symptom reduction in emotional exhaustion and cynicism after 12 sessions.
- 64% of patients maintain improvements for 1+ year (Journal of Occupational Health Psychology, 2020).
Why CBT Works
- Reframes Toxic Thoughts: Replaces “I must work nonstop” with “My worth isn’t tied to productivity.”
- Builds Boundaries: Teaches assertive communication to avoid overcommitment.
- Enhances Problem-Solving: Strengthens prefrontal cortex function, reversing burnout’s brain damage.
Case Study: Teachers using CBT reduce burnout symptoms by 75% in 10 weeks by challenging the “I must save every student” mindset.
Bonus FAQ: “How Long Does Burnout Recovery Take?”
- Mild Burnout: 4-12 weeks with consistent therapy (e.g., biofeedback + CBT).
- Severe Burnout: 6-12 months, requiring professional support and lifestyle overhauls.
- Tools to Speed Recovery: Use Neurotrac Simplex Muscle Biofeedback daily to reduce physical tension by 55% in 3 weeks.
Conclusion: Take Charge of Your Burnout Recovery
Burnout isn’t a life sentence—it’s a wake-up call. Armed with the right therapy for burnout, you can reverse its physical and emotional toll, rebuild resilience, and reclaim your energy. Let’s recap the most powerful strategies to heal and thrive:
Your Burnout Recovery Toolkit: Proven Solutions
Biofeedback Therapy:
- Devices like the Mendi Headband (neurofeedback) and HeartMath (HRV training) provide real-time control over stress responses, resulting in 50-75% symptom reduction in studies.
- Start today: Utilize biofeedback to identify burnout risks early and train your body to remain calm under pressure.
Cognitive Behavioral Therapy (CBT):
- Rewire perfectionist thinking and set boundaries with 70-80% success rates in clinical trials.
- Try now: Challenge one toxic thought daily (e.g., “Rest is productive”).
Mindfulness & Lifestyle Shifts:
- Lower cortisol by 50% with aerobic exercise, or slash emotional exhaustion by 60% with mindfulness.
- Act today: Pair morning meditation with the BioSignals 5 Biofeedback Sensors Device to master stress-relief breathing.
Burnout Prevention: Your Long-Term Game Plan
- Track biomarkers: Use the HeartMath HRV or Neurovizr EEG Headset to monitor stress resilience weekly.
- Build habits: Prioritize sleep, nutrient-rich meals, and digital detoxes.
- Combine therapies: Layer biofeedback with CBT and mindfulness for bulletproof resilience.
Your Next Step: Begin Healing Today
The science is precise—burnout is reversible, but action is non-negotiable. Explore our affiliate-linked biofeedback devices and resources to start your recovery:
- Mendi Headband: Train your brain for calm focus in just 10 minutes a day.
- HeartMath Inner Balance for Focus & Calm: Balance your nervous system with HRV-guided breathing.
- BioSignals 5 Biofeedback Sensors Device: Master diaphragmatic breathing to cut anxiety by 65%.
Remember: Burnout recovery isn’t about perfection—it’s about progress. Every small step toward self-regulation and boundary-setting is a victory.
FAQs: Therapy for Burnout – Prevention & Recovery
Burnout is a state of chronic emotional, mental, and physical exhaustion caused by prolonged stress, often related to work or personal responsibilities. Unlike stress, which is temporary and situational, burnout is a systemic condition marked by three key symptoms:
- Emotional exhaustion (feeling drained despite rest).
- Detachment/cynicism (losing interest in work or relationships).
- Reduced performance (declining productivity and motivation).
Stress can motivate action, but burnout paralyzes—it’s like a broken charger for your energy battery.
Burnout develops gradually. Watch for these red flags:
- Physical: Chronic fatigue, headaches, insomnia, frequent illnesses.
- Emotional: Irritability, hopelessness, numbness, or cynicism.
- Behavioral: Procrastination, social withdrawal, increased mistakes at work.
Biofeedback uses real-time data (e.g., heart rate, brainwaves) to train your body’s stress response. Proven benefits include:
- 30–40% lower cortisol levels in 8 weeks.
- 60–75% improvement in emotional regulation (e.g., with neurofeedback devices like Mendi Headband).
- Faster recovery from mental fatigue compared to traditional therapy.
Yes! CBT targets the root causes of burnout, such as perfectionism and poor boundaries. Studies show:
- 70–80% reduction in emotional exhaustion after 12 sessions.
- 64% of patients maintain improvements long-term.
CBT steps to try:
- Challenge thoughts like, “I must work nonstop to succeed.”
- Replace them with, “My worth isn’t tied to productivity.”
- Mild burnout: 4–12 weeks with consistent therapy (e.g., biofeedback + CBT).
- Severe burnout: 3–12 months, often requiring professional support.