Panic attacks can be overwhelming and disruptive, leaving individuals feeling helpless and out of control. Fortunately, Cognitive Behavioral Therapy for Panic Disorder is a proven, effective treatment that helps people break free from the cycle of fear and anxiety. By addressing negative thought patterns, gradually exposing individuals to their worries, and teaching coping strategies, CBT for Panic Disorder empowers individuals to manage panic attacks. This evidence-based approach provides long-term relief, giving people the confidence to regain control of their lives. In this article, we’ll explore how CBT for coping with Panic Attacks works, its key techniques, and how it can transform the way individuals respond to anxiety.
Introduction
Experiencing sudden waves of intense fear, a racing heartbeat, dizziness, and shortness of breath can be overwhelming. These are common symptoms of panic attacks, which can strike without warning and significantly impact daily life. If left unmanaged, they may develop into panic disorder, where individuals live in constant fear of the next episode. Fortunately, Cognitive Behavioral Therapy for Panic Disorder has proven to be one of the most effective treatments, offering long-term relief without relying solely on medication.
CBT for Panic Disorder is a structured, evidence-based approach that helps individuals understand and change the negative thought patterns fueling their anxiety. Many panic attacks stem from misinterpreting physical sensations—such as an increased heart rate being mistaken for a heart attack. CBT for coping with Panic Attacks teaches people to challenge these fears, gradually reduce avoidance behaviors, and build confidence in managing their symptoms.
This therapy works through techniques like cognitive restructuring, exposure therapy, and relaxation strategies. Individuals gain greater control over their emotional responses by learning to identify and modify anxious thoughts. Unlike short-term solutions, CBT for Panic Disorder empowers individuals with lasting strategies to prevent future attacks.
In this article, we’ll explore how Cognitive Behavioral Therapy for Panic Disorder works, the key techniques used, and how you can incorporate them into your life to regain a sense of calm and control.
Understanding Panic Attacks
Panic attacks can feel terrifying, coming out of nowhere and leaving you feeling powerless. Your heart pounds, your breath shortens, and a sense of doom takes over. But what exactly causes them, and how do they affect daily life? To manage panic attacks effectively, it’s essential to understand their causes, triggers, and symptoms—as well as how Cognitive Behavioral Therapy for Panic Disorder can help break the cycle.
Causes and Triggers of Panic Attacks
Panic attacks don’t happen randomly; they often stem from a combination of biological, psychological, and environmental factors. Here are some of the most common causes:
- Genetics: If a close family member struggles with anxiety or panic disorder, you may be more prone to experiencing panic attacks.
- Stress and Trauma: High levels of stress, major life changes, or past traumatic experiences can trigger sudden panic episodes.
- Overactive Fight-or-Flight Response: The body’s natural response to danger can misfire, causing intense fear even when no real threat exists.
- Negative Thinking Patterns: Catastrophic thoughts like “I’m losing control” or “I’m having a heart attack” fuel anxiety and can make a mild sensation escalate into a full-blown panic attack.
- Substance Use: Caffeine, alcohol, and stimulants can heighten anxiety levels and increase the likelihood of panic attacks.
- Health Conditions: Some medical issues, like heart disease, thyroid imbalances, or respiratory conditions, can mimic or trigger panic symptoms.
Understanding what triggers your panic attacks is the first step in managing them. Triggers vary from person to person but may include crowded spaces, social situations, driving, public speaking, or even specific thoughts and memories. CBT for Panic Attacks helps individuals identify and reframe these triggers, reducing their power over time.

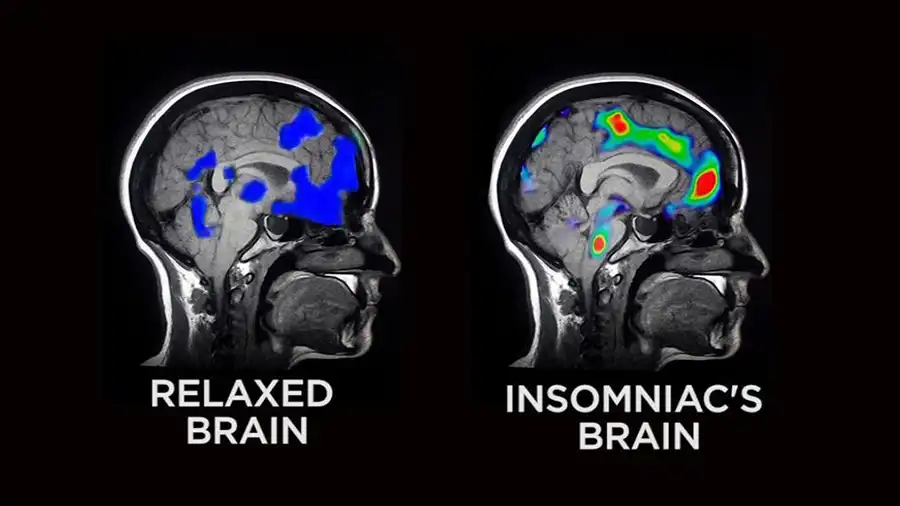
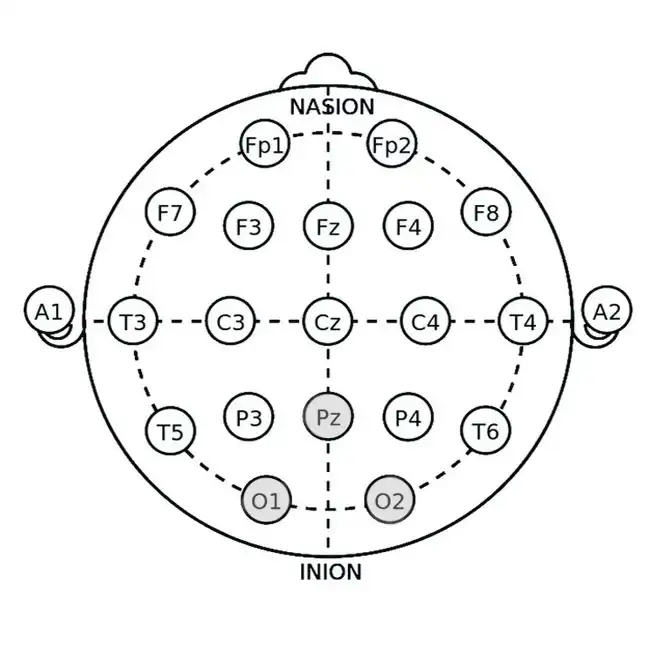
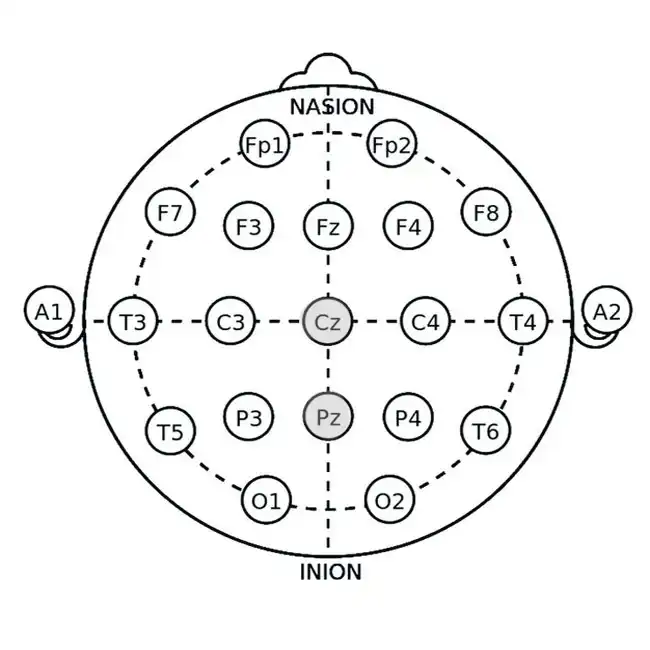
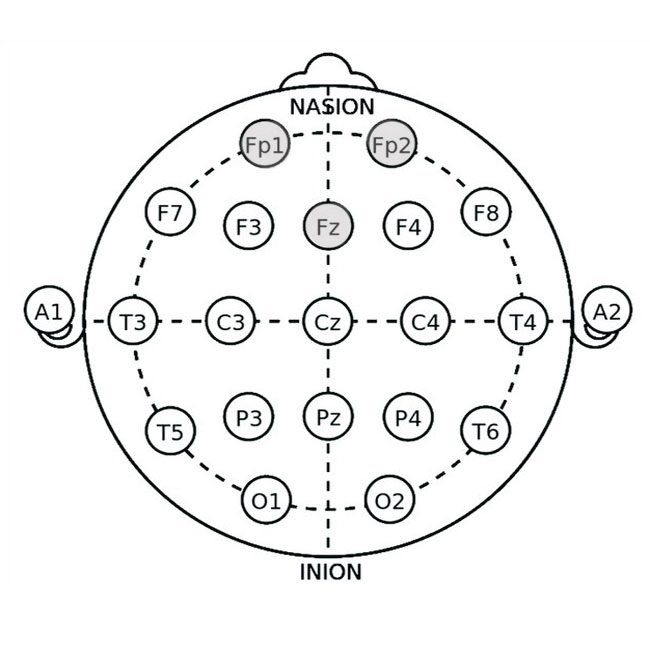
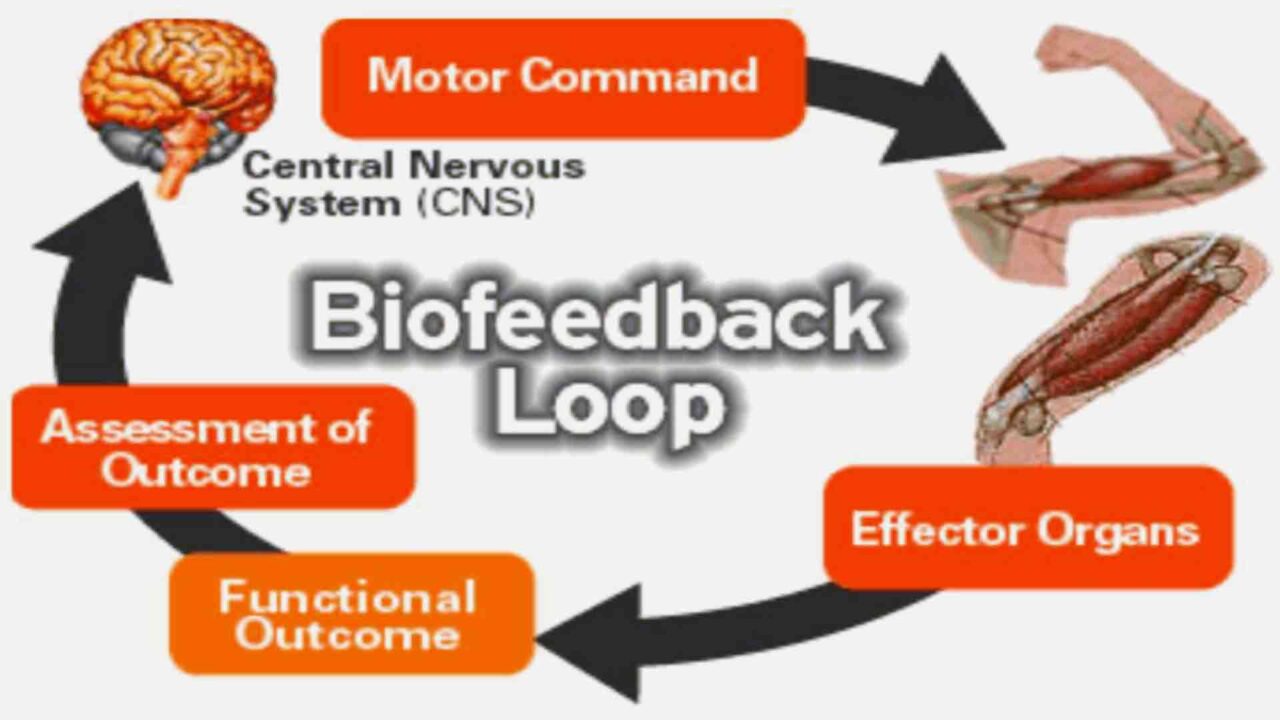
How Panic Attacks Affect the Brain: The Neuroscience of Anxiety
Panic attacks are not just psychological—they have a profound impact on the brain. When experiencing a panic attack, the brain’s fear response system goes into overdrive, triggering intense physical and emotional symptoms. Understanding these neurological changes can help explain why Cognitive Behavioral Therapy for Panic Disorder is so effective in retraining the brain’s response to fear.
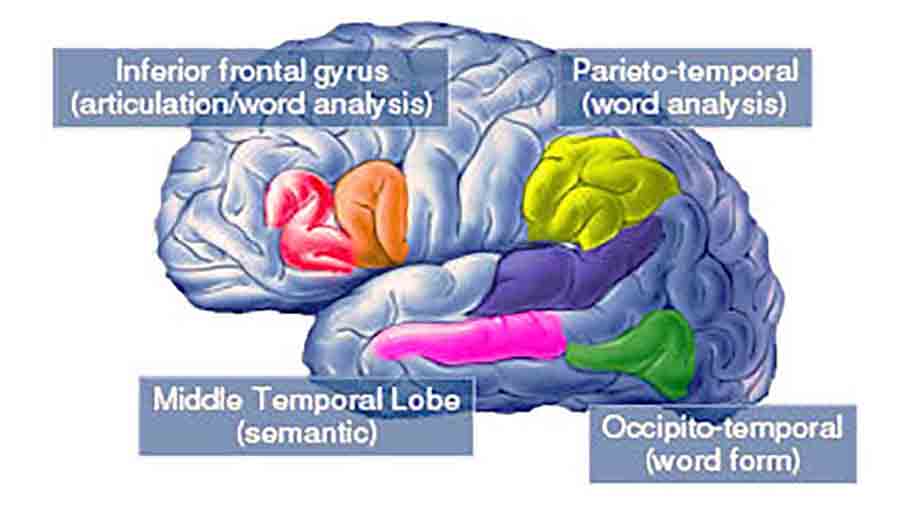
The Role of the Amygdala: The Fear Center
The amygdala, a small structure deep in the brain, detects threats and triggers the body’s fight-or-flight response. In people with panic disorder, the amygdala becomes hyperactive, misinterpreting harmless situations as dangerous, leading to sudden and overwhelming fear. CBT for Panic Disorder helps by teaching individuals to reframe these fearful thoughts and gradually reduce the amygdala’s overreaction.
The Prefrontal Cortex: Regaining Control
The prefrontal cortex is responsible for rational thinking and emotional regulation. During a panic attack, this area of the brain struggles to override the amygdala’s fear signals, making it difficult to think clearly. CBT for Panic Attacks strengthens the prefrontal cortex by training individuals to challenge irrational fears and regain control over their emotions.
The Role of Neurotransmitters: Anxiety and Brain Chemistry
Panic attacks are also influenced by imbalances in brain chemicals like serotonin, norepinephrine, and gamma-aminobutyric acid (GABA). These neurotransmitters regulate mood and stress levels. CBT for Panic Disorder helps restore balance by reducing chronic stress and teaching effective relaxation techniques.
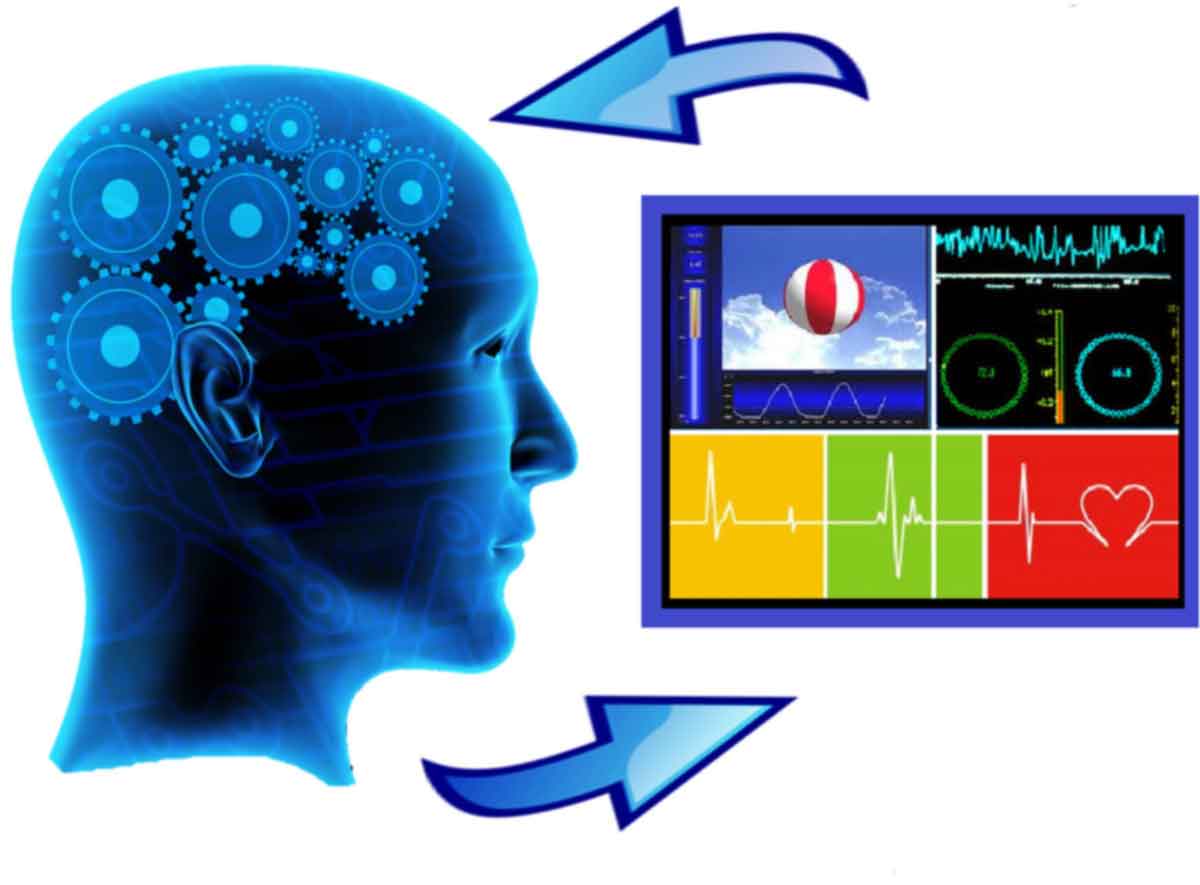
How CBT Rewires the Brain for Long-Term Relief
Through consistent practice, Cognitive Behavioral Therapy for Panic Disorder helps the brain create new neural pathways, replacing anxious thought patterns with more balanced and rational responses. Over time, this process reduces the frequency and intensity of panic attacks, allowing individuals to feel calmer and more in control.
By understanding how panic attacks affect the brain, individuals can see why CBT for Panic Attacks is one of the most effective treatments available. With the proper techniques, it is possible to retrain the brain, break free from anxiety, and live a more peaceful life.
Symptoms and Impact on Daily Life
Panic attacks involve physical and psychological symptoms, lasting from a few minutes to an hour. Some of the most common include:
- Rapid heartbeat or palpitations
- Shortness of breath or choking sensation
- Dizziness or feeling faint
- Chest pain or discomfort
- Sweating and trembling
- A feeling of detachment from reality (derealization)
- Fear of losing control, going crazy, or dying
For individuals with panic disorder, these attacks become frequent and unpredictable, leading to fear of having another attack. This fear can result in avoidance behaviors, such as:
- Avoiding crowded places, public transportation, or social gatherings.
- Constantly checking physical sensations for signs of an attack.
- Relying on “safety behaviors” like carrying medication, always having an exit plan, or needing someone nearby for reassurance.
This cycle of fear and avoidance can severely limit personal freedom, relationships, and work performance. The good news is that CBT for Panic Disorder teaches individuals how to break this cycle, helping them regain confidence and control.

What Is Cognitive Behavioral Therapy (CBT)?
Panic attacks can feel like an unstoppable force, but the good news is that they can be managed—and even prevented. One of the most effective treatments for panic and anxiety is Cognitive Behavioral Therapy for Panic Disorder. Unlike medication, which mainly controls symptoms, CBT for coping with Panic Attacks helps individuals change the thoughts and behaviors that fuel their anxiety, leading to lasting relief.
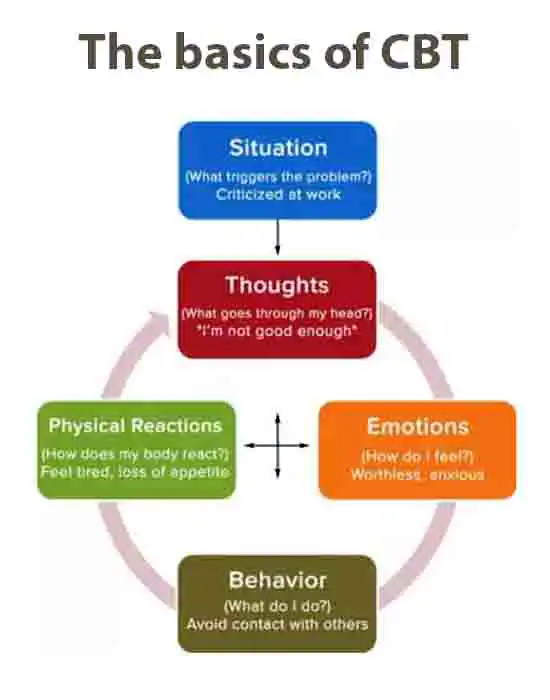
Core Principles of CBT
At its core, Cognitive Behavioral Therapy for Panic Disorder is based on the idea that our thoughts, emotions, and behaviors are interconnected. When a person experiences a panic attack, it’s often due to negative thought patterns that trigger fear and physical symptoms. CBT focuses on:
- Identifying Negative Thought Patterns – Recognizing irrational fears contributing to panic attacks.
- Cognitive Restructuring – Replacing fear-based thoughts with more rational, balanced ones.
- Exposure Therapy – Gradually facing feared situations to reduce avoidance behaviors.
- Behavioral Techniques – Practicing relaxation exercises and controlled breathing to calm the nervous system.
Instead of viewing panic attacks as uncontrollable, CBT for coping with Panic Attacks teaches people that fear comes from their interpretation of symptoms, not the symptoms themselves. By shifting these interpretations, individuals can manage panic attacks before they escalate.

How CBT Works for Anxiety and Panic
CBT is structured, goal-oriented, and typically short-term, making it a practical solution for those struggling with panic disorder. Sessions often include:
- Understanding Triggers: Learning what situations or thoughts spark panic attacks.
- Tracking Thought Patterns: Identifying anxious thoughts and how they influence emotions.
- Challenging Catastrophic Thinking: Replacing “I’m going to die” with “This is temporary and will pass.”
- Gradual Exposure: Facing feared situations in a controlled way to reduce panic sensitivity.
- Relaxation and Coping Strategies: To counteract physical symptoms, use deep breathing, mindfulness, and progressive muscle relaxation.
By practicing these techniques, individuals retrain their brains to respond differently to anxiety, reducing both the frequency and intensity of panic attacks.
Evidence-Based Effectiveness of CBT
CBT is widely regarded as the gold standard treatment for coping with panic attacks and panic disorder, with decades of research supporting its effectiveness. Studies show:
- 70–90% of individuals who complete a structured CBT program experience significant reductions in panic symptoms.
- CBT is as effective as medication for treating panic disorder, but with long-term benefits and no side effects.
- CBT prevents relapse, while medication alone often leads to recurrence after stopping treatment.
By addressing both thoughts and behaviors, CBT for Panic Disorder empowers individuals to regain control over their mental well-being. Unlike temporary fixes, it offers a lifelong toolkit for managing anxiety and preventing future attacks.
CBT Techniques for Panic Attacks
Managing panic attacks requires more than just coping in the moment—you need to break the cycle of fear and avoidance. Cognitive Behavioral Therapy for Panic Disorder provides structured, science-backed techniques that help individuals regain control over their anxiety. These methods target both the thoughts that trigger panic and the behaviors that reinforce it. Below are the most effective CBT strategies for coping with Panic Attacks.
Cognitive Restructuring: Changing Thought Patterns
Panic attacks often begin with distorted thinking—misinterpreting bodily sensations as signs of danger. For example, feeling dizzy might lead to the thought, “I’m going to faint,” which increases fear and triggers more symptoms. CBT for Panic Disorder helps individuals recognize and challenge these unhelpful thoughts through:
- Thought Journaling: Writing down anxious thoughts and analyzing their accuracy.
- Reality Testing: Asking, “Has this fear ever actually come true?”
- Balanced Thinking: Replacing panic-driven thoughts with logical alternatives (e.g., “This feeling is temporary, and I am safe.”).
By practicing cognitive restructuring, individuals stop catastrophic thinking before it escalates into a panic attack.
Exposure Therapy: Facing Fears Gradually
Avoidance is a major factor in panic disorder. People often stay away from places or situations that might trigger panic, reinforcing the belief that they are dangerous. CBT for Panic Attacks uses gradual exposure therapy to break this cycle by facing fears in small, controlled steps.
- Interoceptive Exposure: Simulating physical sensations of panic in a safe setting (e.g., spinning in a chair to mimic dizziness).
- Situational Exposure: Facing feared environments (e.g., driving, crowded spaces) gradually and repeatedly.
- Desensitization: Over time, the brain learns that these situations are not dangerous, reducing panic sensitivity.
Regular exposure helps individuals regain confidence and see that panic attacks do not have to control their lives.
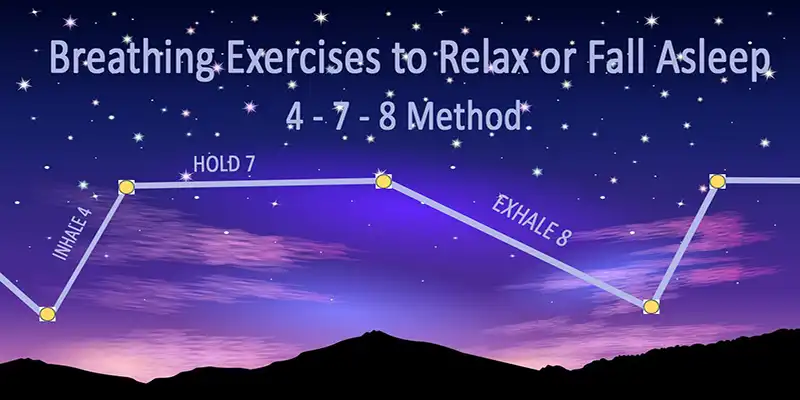
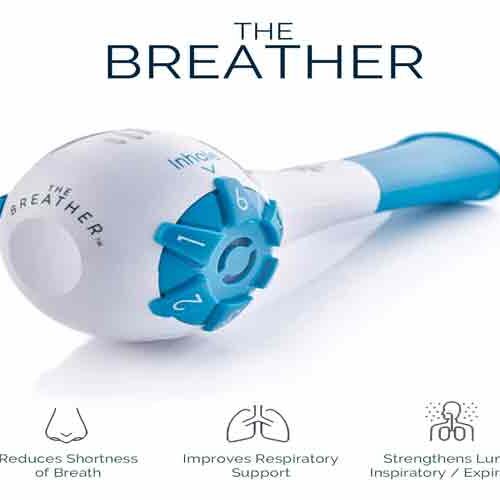
Relaxation Techniques: Breathing & Mindfulness
Panic attacks trigger the fight-or-flight response, flooding the body with adrenaline and causing symptoms like a racing heart, dizziness, and shortness of breath. CBT for Panic Disorder includes relaxation techniques that counteract these effects, helping individuals calm their nervous system:
- Diaphragmatic Breathing: Slowing down breathing to prevent hyperventilation. (Inhale for 4 seconds, hold for 4, exhale for 6.)
- Progressive Muscle Relaxation: Tensing and relaxing muscle groups to release physical tension.
- Mindfulness Meditation: Focusing on the present moment instead of fear-based thoughts.
Practicing these techniques daily helps reduce the intensity of panic attacks and makes them easier to manage.

Behavioral Strategies: Breaking the Fear Cycle
Behavioral patterns often maintain panic disorder. For example, constantly checking your pulse or avoiding physical activity because of fear of a rapid heartbeat reinforces anxiety. CBT for Panic Attacks introduces strategies to change these behaviors:
- Reducing Safety Behaviors: Letting go of crutches, like always carrying water or needing a companion in public.
- Building Tolerance to Discomfort: Engaging in activities that increase heart rate (e.g., exercise) to prove that physical sensations are not dangerous.
- Developing Coping with Panic Attacks Plans: Creating action steps to manage panic when it arises instead of avoiding triggers.
By changing behaviors, individuals break the panic-avoidance cycle and gain greater control over their anxiety.


The CBT Process for Panic Attacks
Overcoming panic attacks doesn’t happen overnight, but Cognitive Behavioral Therapy for Panic Disorder provides a structured approach to long-term relief. The process is tailored to each individual, ensuring that the CBT for Panic Attacks techniques are personalized and effective. Below is a breakdown of how therapy unfolds, from the initial session to measurable progress.
Initial Assessment and Goal Setting
The first step in CBT for Panic Disorder is a thorough assessment. During this stage, a therapist:
- Identifies Triggers: What situations, thoughts, or physical sensations lead to panic attacks?
- Explores Thought Patterns: How does the individual interpret anxiety symptoms?
- Assesses Avoidance Behaviors: What situations or activities does the person avoid due to fear of panic?
- Sets Clear Goals: Examples include reducing panic attacks by 50%, being able to drive alone, or returning to social events.
Establishing these goals helps create a focused treatment plan that keeps therapy on track.
Developing a Personalized Treatment Plan
Once the assessment is complete, a CBT for Panic Attacks treatment plan is created based on individual needs. This typically includes:
- Cognitive Restructuring – Identifying and challenging panic-related thoughts.
- Exposure Therapy – Gradually facing feared situations to reduce avoidance.
- Behavioral Modifications – Reducing safety behaviors that reinforce anxiety.
- Relaxation Techniques – Practicing deep breathing and mindfulness to manage symptoms.
The plan is flexible, allowing adjustments based on progress and challenges.
Session Structure and Homework Assignments
A standard CBT for Panic Disorder session follows a structured format:
- Check-In: Reviewing symptoms, progress, and challenges since the last session.
- Skill Development: Learning and practicing CBT techniques (e.g., cognitive restructuring, exposure exercises).
- Reviewing Homework: Discussing real-life application of strategies outside therapy.
- Planning Next Steps: Assigning new exercises to reinforce learning.
Homework is a key component of CBT for Panic Attacks. It ensures that individuals apply therapy techniques in daily life, accelerating progress.
Measuring Progress and Adjusting Strategies
CBT is goal-oriented, meaning progress is actively tracked. Therapists use:
- Symptom Journals: Recording panic attacks, triggers, and thoughts.
- Behavioral Tracking: Monitoring avoidance patterns and exposure therapy results.
- Cognitive Assessments: Evaluating changes in thought patterns over time.
If a technique isn’t working, the treatment plan is adjusted. This flexibility ensures that therapy remains effective and tailored to the individual’s needs.
Benefits of CBT for Panic Attacks
Cognitive Behavioral Therapy for Panic Disorder is one of the most effective treatments for managing and overcoming panic attacks. Unlike quick fixes, CBT for Panic Attacks provides long-lasting relief by addressing the root causes of anxiety and equipping individuals with tools to manage their symptoms. Below are the key benefits of this approach.
Long-Term Relief and Prevention
One of the biggest advantages of CBT for Panic Disorder is its focus on permanent change. Instead of just treating symptoms, CBT helps individuals:
- Identify Triggers: Understanding what sparks a panic attack reduces fear of the unknown.
- Break the Fear Cycle: Changing negative thought patterns prevents panic attacks from escalating.
- Reduce Avoidance Behaviors: Exposure therapy helps individuals regain control over their lives.
Studies show that CBT has lasting effects, with many individuals experiencing significant symptom reduction even years after treatment.
Empowerment and Self-Management Skills
Unlike medication, which relies on external support, CBT for Panic Attacks empowers individuals to become their own therapists. Through CBT, they learn:
- Cognitive Restructuring: How to challenge catastrophic thoughts before they spiral into panic.
- Relaxation Techniques: Breathing and mindfulness exercises that can stop a panic attack in its tracks.
- Behavioral Strategies: Ways to gradually face fears and reduce avoidance patterns.
This sense of control makes individuals feel stronger, more confident, and better equipped to handle future anxiety.
Improved Quality of Life
Panic attacks can be debilitating, affecting work, relationships, and daily activities. By using CBT for Panic Disorder, individuals experience:
- Greater Freedom: No longer avoiding situations out of fear.
- Better Relationships: Reduced anxiety improves social connections.
- Increased Productivity: Less time spent worrying means more focus on goals.
- Overall Well-Being: Reduced stress leads to better physical and mental health.
CBT doesn’t just help with panic—it creates a healthier mindset for life.
Overcoming anxiety and panic is essential for personal success and building the confidence needed for professional achievement.
Challenges and Considerations
While Cognitive Behavioral Therapy for Panic Disorder is highly effective, the journey isn’t always smooth. Some individuals may face challenges in therapy, and in some cases, CBT for Panic Attacks alone may not be enough. Understanding these barriers can help individuals set realistic expectations and maximize their success.
Common Barriers to Success in CBT
Not everyone experiences immediate relief with CBT for Panic Disorder. Some common challenges include:
- Resistance to Change: Adjusting long-held thought patterns can be difficult, especially when panic attacks have been part of daily life for years.
- Avoidance Behaviors: Exposure therapy, a key CBT technique, requires individuals to face their fears gradually. This process can be uncomfortable, and some may struggle with completing exposure exercises.
- Inconsistent Practice: CBT for coping with Panic Attacks is most effective when techniques are practiced regularly outside of therapy sessions. However, a lack of motivation or forgetting to apply strategies in real-life situations can slow progress.
- High Anxiety Levels: Some individuals may feel overwhelmed by their symptoms, making it difficult to engage in therapy effectively.
Overcoming these barriers requires commitment, patience, and sometimes additional support from a therapist or loved ones.
When CBT Might Not Be Enough
While CBT for Panic Disorder is a gold-standard treatment, it may not be the right fit for everyone. In some cases, individuals might:
- Have severe or treatment-resistant anxiety that requires additional interventions.
- Struggle with co-occurring conditions such as depression, PTSD, or other mental health disorders.
- Experience intrusive thoughts that are difficult to control even with cognitive restructuring techniques.
- Find it hard to engage in therapy due to life stressors, trauma, or medical conditions.
If CBT for Panic Attacks alone isn’t providing enough relief, a combined treatment approach may be necessary.
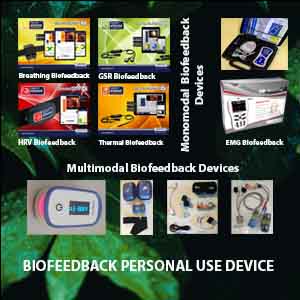
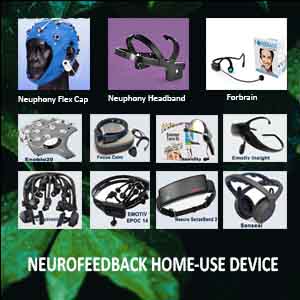
Combining CBT with Other Treatments
For those who need extra support, CBT for Panic Disorder can be combined with other treatments for a more comprehensive approach. These may include:
- Medication: Selective serotonin reuptake inhibitors (SSRIs) or benzodiazepines can help stabilize severe anxiety symptoms, making it easier to engage in therapy.
- Mindfulness and Relaxation Techniques: Practices such as meditation, yoga, and progressive muscle relaxation can enhance CBT strategies.
- Support Groups or Counseling: Connecting with others who experience panic attacks can provide emotional support and additional coping strategies.
- Lifestyle Adjustments: Regular exercise, a healthy diet, and proper sleep can significantly reduce anxiety symptoms and complement CBT.
The key is finding the right balance of treatments to achieve long-term relief.
Tips for Long-Term Panic Attack Management
Managing panic attacks isn’t just about short-term relief—it’s about building lasting resilience. Even after successful Cognitive Behavioral Therapy for Panic Disorder, individuals may experience occasional anxiety spikes. However, with the right strategies, they can prevent relapse and maintain long-term progress.
Preventing Relapse
Even after completing CBT for Panic Attacks, some individuals may experience setbacks. To prevent relapse, it’s essential to:
- Continue Practicing CBT Techniques: Cognitive restructuring, exposure therapy, and relaxation exercises should become lifelong habits.
- Identify Early Warning Signs: Early recognition of triggers and physical sensations can help prevent a full-blown panic attack.
- Avoid Avoidance: Resisting certain situations due to fear can reinforce anxiety. Instead, gradually exposing oneself to triggers helps maintain progress.
- Maintain a Healthy Lifestyle: Regular exercise, balanced nutrition, and sufficient sleep help regulate emotions and reduce stress levels.
- Seek Support When Needed: If anxiety resurfaces, reconnecting with a therapist or support group can help reinforce coping strategies.
By staying proactive, individuals can significantly reduce the likelihood of panic attacks returning.
Building Resilience and Coping Skills
Beyond preventing relapse, the goal of CBT for Panic Disorder is to build emotional resilience. Here are key ways to strengthen mental well-being:
- Develop a Growth Mindset: Viewing challenges as learning experiences rather than setbacks helps maintain confidence in handling anxiety.
- Stay Consistent with Self-Care: Regular mindfulness exercises, deep breathing, and progressive muscle relaxation keep anxiety in check.
- Engage in Positive Social Interactions: Support from friends, family, or support groups provides encouragement and reduces feelings of isolation.
- Set Realistic Goals: Small, achievable milestones create a sense of progress and reduce overwhelming feelings.
- Practice Self-Compassion: Being kind to oneself and acknowledging progress (even if slow) makes a significant difference in long-term recovery.
CBT for Panic Attacks doesn’t just teach coping skills—it empowers individuals to take control of their mental health for life.
Conclusion
Coping with panic attacks is possible with the right approach. Cognitive Behavioral Therapy for Panic Disorder has helped countless individuals regain control over their anxiety and improve their quality of life. By addressing unhelpful thought patterns, gradually facing fears, and learning effective coping strategies, people can achieve long-term relief from panic attacks.
Key Takeaways
- CBT for Panic Attacks is highly effective, providing long-term solutions rather than temporary relief.
- Panic attacks are treatable, and understanding their causes, symptoms, and triggers is the first step toward recovery.
- CBT techniques, such as cognitive restructuring, exposure therapy, and relaxation strategies, empower individuals to break free from the fear cycle.
- Consistency and practice are key—applying CBT techniques regularly strengthens resilience and prevents relapse.
- Additional support, such as medication or mindfulness practices, may enhance results for those who need extra help.
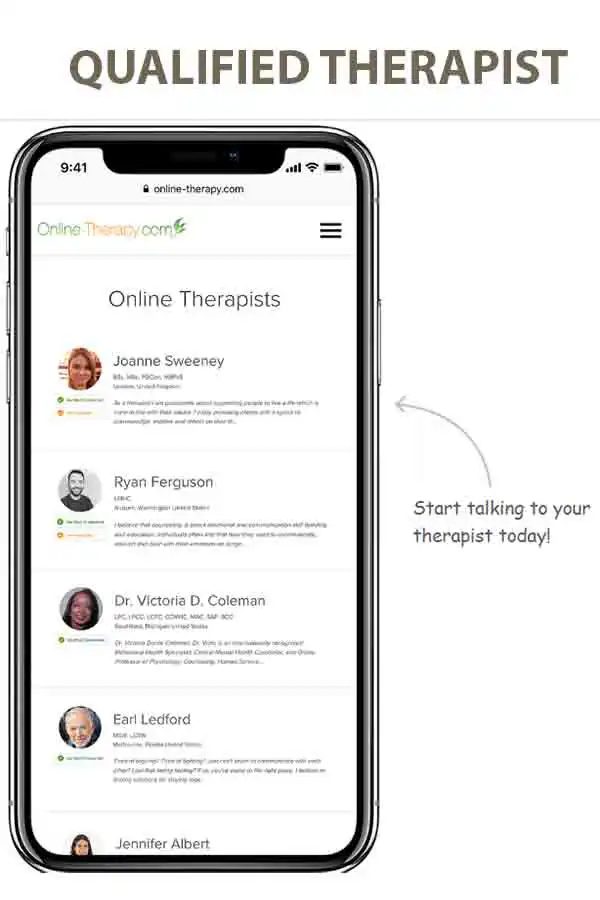
Encouragement for Seeking Help
If you or someone you know is struggling with panic attacks, remember that help is available, and recovery is possible. Seeking professional guidance from a CBT-trained therapist can provide the tools needed to overcome anxiety and regain confidence.
For those who prefer a self-help approach, many resources—including online CBT therapy, CBT workbooks, guided programs, and mindfulness practices—can support the journey toward healing.
You are not alone. With the right strategies, you can manage panic attacks and live a calmer, more fulfilling life.
FAQ: CBT for Panic Attacks
Cognitive Behavioral Therapy (CBT) for panic attacks is a structured, evidence-based approach that helps individuals understand and change the thoughts and behaviors that trigger or worsen panic attacks. It teaches how to manage fear before it spirals out of control.
CBT addresses the cycle of fear, teaching you to:
- Recognize and challenge irrational thoughts
- Respond differently to physical symptoms
- Desensitize yourself to triggers
This helps reduce both the frequency and intensity of panic attacks.
CBT is considered the gold standard treatment for panic disorder. Most people experience significant and lasting relief, often within 8–16 sessions.
- Cognitive restructuring to challenge catastrophic thinking
- Interoceptive exposure to reduce fear of physical sensations
- Relaxation and breathing techniques
- Behavioral experiments to test feared outcomes
- Journaling and thought tracking
Most people notice improvement within a few weeks, with substantial progress occurring within 2–3 months, especially if they practice the techniques regularly.
CBT offers long-term relief without side effects, while medication (like SSRIs or benzodiazepines) may only offer temporary symptom control. In many cases, CBT is more effective, especially for preventing future attacks.
Yes. By teaching you to respond calmly to early signs of panic, CBT breaks the cycle of anxiety, builds resilience, and gives you tools to stay panic-free in the long run.
You can:
- Find a local CBT therapist
- Use an online CBT program, like the one mentioned in the article
- Practice the techniques described in the article to get started right away