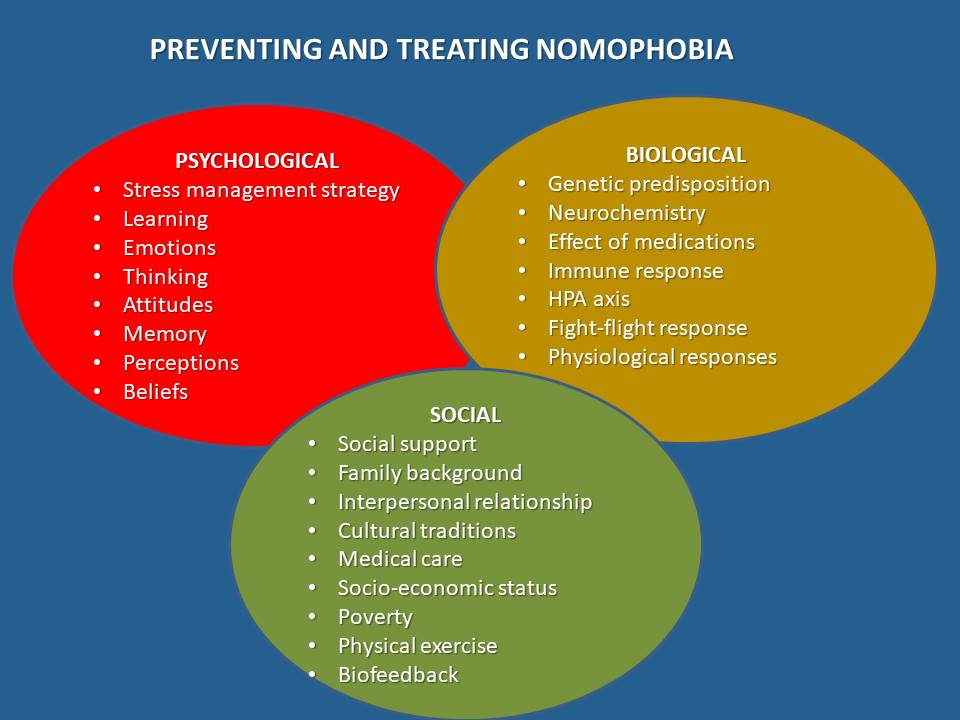
In the digital era, the pervasive phenomenon of Nomophobia, or the fear of being without one’s mobile phone, has given rise to a pressing need for effective interventions. Among the innovative approaches, Nomophobia treatment through biofeedback emerges as a promising solution. Leveraging advanced technology, Biofeedback offers a tailored and dynamic method to address the escalating concerns associated with smartphone dependency. This treatment modality allows individuals to gain insight into their physiological responses during moments of phone separation anxiety, fostering self-awareness and real-time control. By combining the power of biofeedback modalities technology with personalized interventions, Nomophobia treatment aims to empower individuals to manage and alleviate the adverse effects of smartphone-related stress, promoting a healthier and more balanced relationship with digital devices.
What is nomophobia?
New technologies have become an integral part of our lives. Rapidly spreading worldwide, smartphones and their applications play a key role in social connections, expression, information sharing, and achievement development. Smartphones have become essentials rather than accessories due to their capacity to perform many tasks with features including advanced operating systems, touch screens, and internet access. Information is easily transmitted and received through text messages, phone calls, emails, faxes, games, movies, videos, and social media.
Smartphones can also combine services, such as “commutainment” (entertainment and communication) and “edutainment” (education and entertainment). Like other modern technologies, many variables must be considered in evaluating their overall benefit and utility. For example, while smartphones provide ready, convenient access to the internet and a sense of comfort and connection to others, they may also result in unhealthy, harmful psychological dependency, anxiety, and possible fear. Smartphones have countless impacts on our lives, potentially including problematic health issues that may develop due to overuse.
The increasingly symbiotic relationship between humans and their handheld devices has given rise to a new psychological phenomenon known as nomophobia, or the fear of being without one’s mobile phone. This modern malady underscores the profound impact of technology on our lives, raising questions about how it alters not only our behavior but also our very brains.
Is Nomophobia a Mental Disorder or Behavioral Addiction?
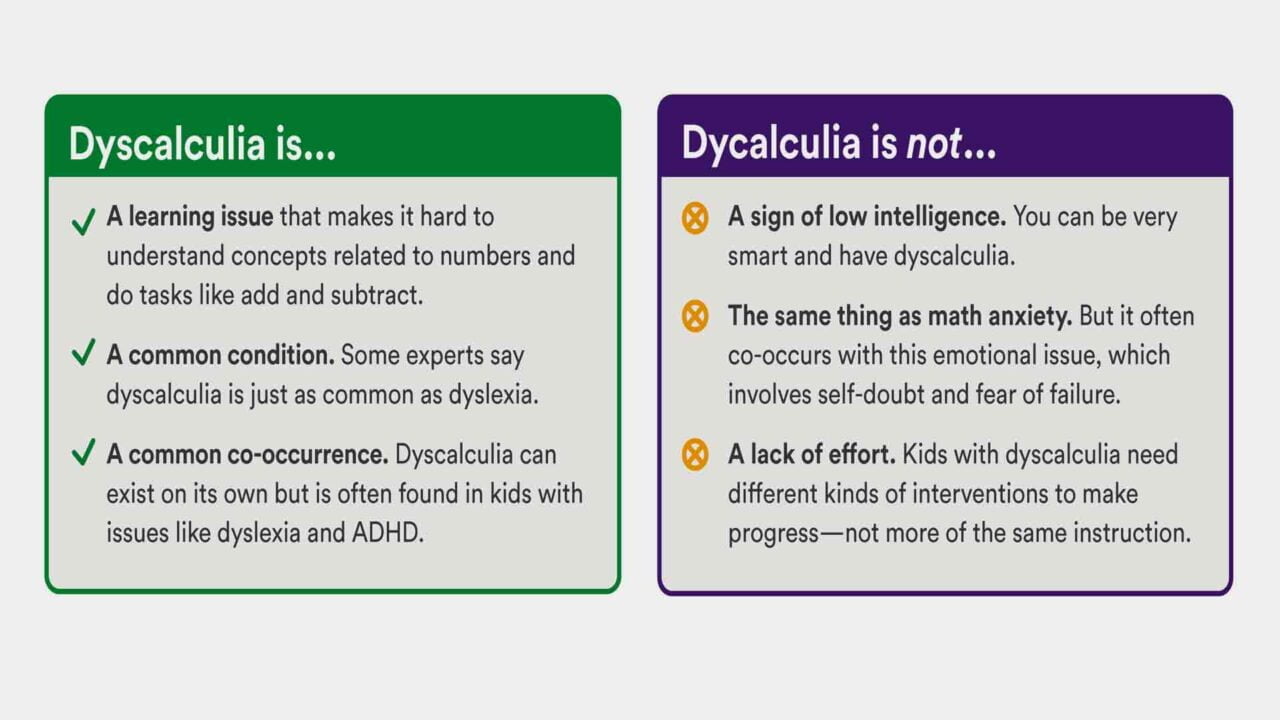
NOMOPHOBIA or NO MObile PHONE PhoBIA describes a psychological condition when people fear being detached from mobile phone connectivity (being out of contact with a mobile phone, having no mobile networks, or having insufficient balance or battery). The term NOMOPHOBIA is constructed from definitions in the DSM-IV; it has been labeled as a “phobia for particular/specific things.”
It’s not officially recognized as a mental disorder in the Diagnostic and Statistical Manual of Mental Disorders (DSM-5). Still, it is often used informally to describe the emotional and psychological distress that can result from being separated from one’s mobile device. While it’s not an officially recognized phobia, it can have a tangible impact on a person’s daily life and mental well-being.
In contrast to other forms of addiction, such as gaming or gambling addiction, which has been categorized as a distinct disease entity according to the International Classification of Disease (ICD), excessive smartphone use is a more general behavioral addiction that has not been officially classified as a disorder. Compared with drug dependence, which affects structural and functional neural correlates through chemical pathways, changes associated with behavioral addiction are more likely through operant learning that involves rewards and punishments for behavioral impacts.
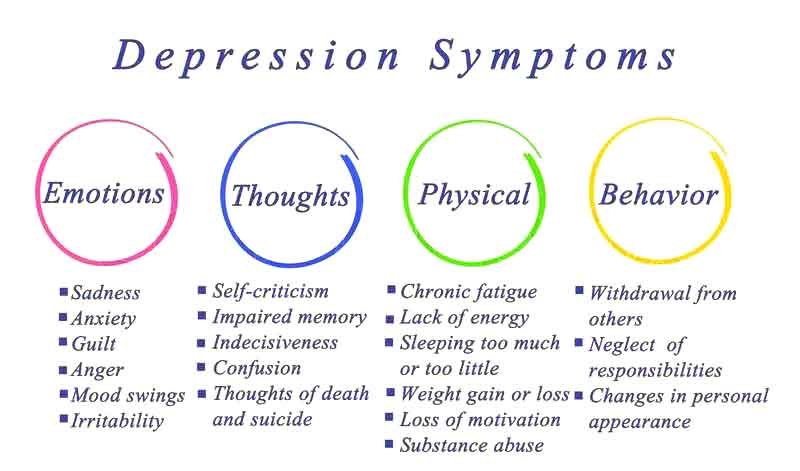
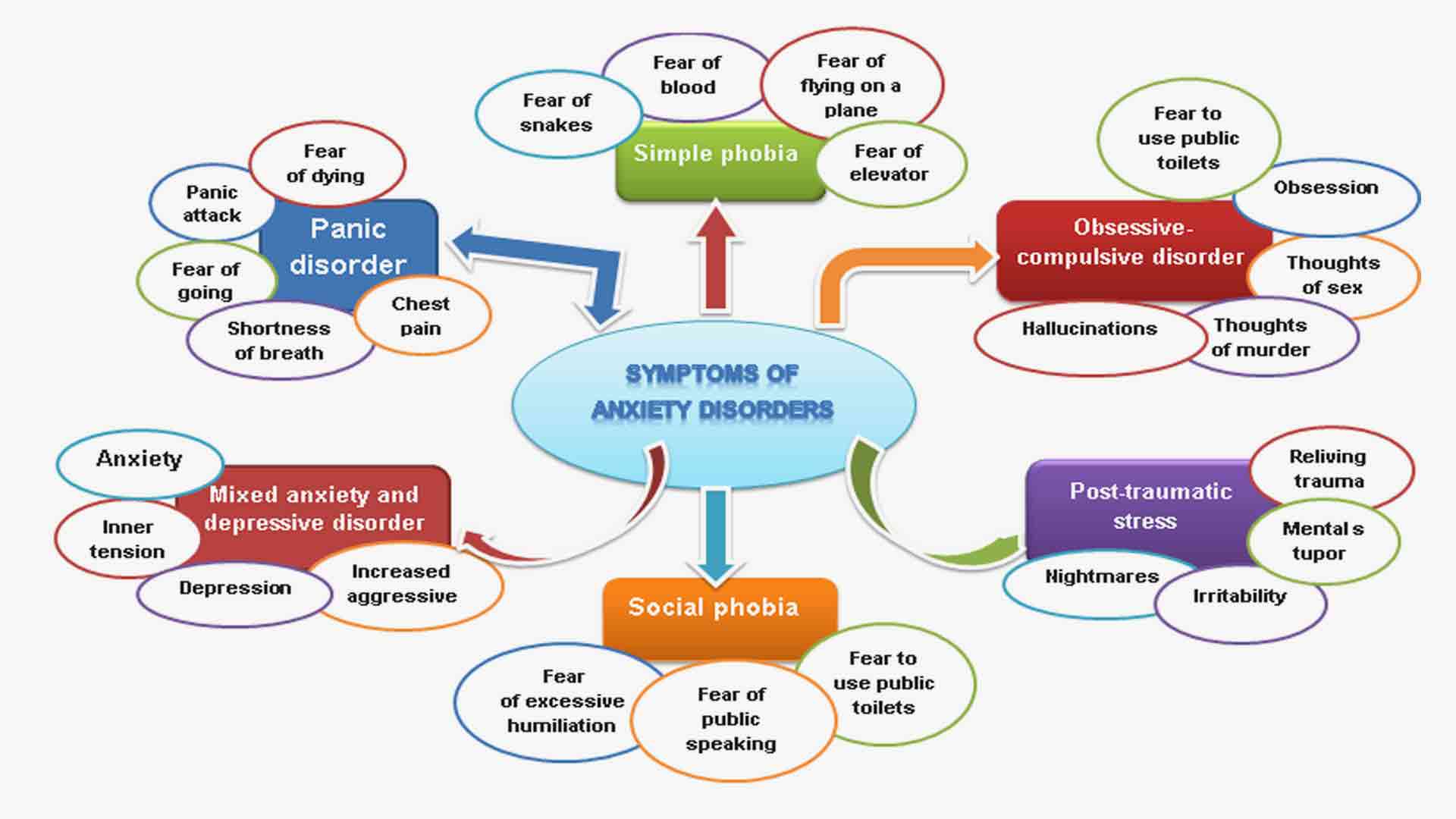
Common symptoms of nomophobia
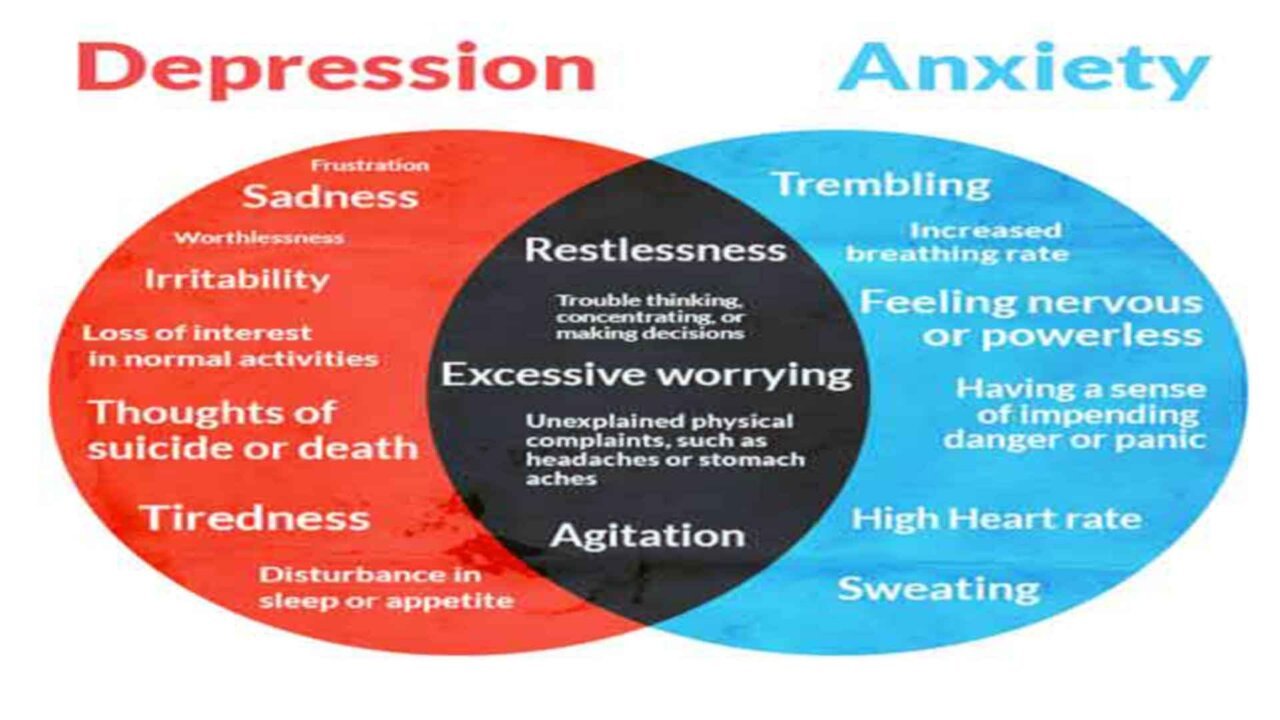
The symptoms of nomophobia include anxiety, panic attacks, and agitation when the phone is not in one’s possession, physical symptoms like trembling, sweating, tachycardia, and disorientation when without the phone, and a persistent need to have the phone within reach at all times. These symptoms are often driven by a deep-seated fear of disconnection, isolation, or the inability to communicate and access information, aligning with the concept of nomophobia.
The below-mentioned signs and symptoms are observed in Nomophobia cases
- Anxiety
- Respiratory alterations
- Trembling
- Perspiration
- Agitation
- Disorientation
- Tachycardia.
- Irritability or restlessness when unable to use the phone.
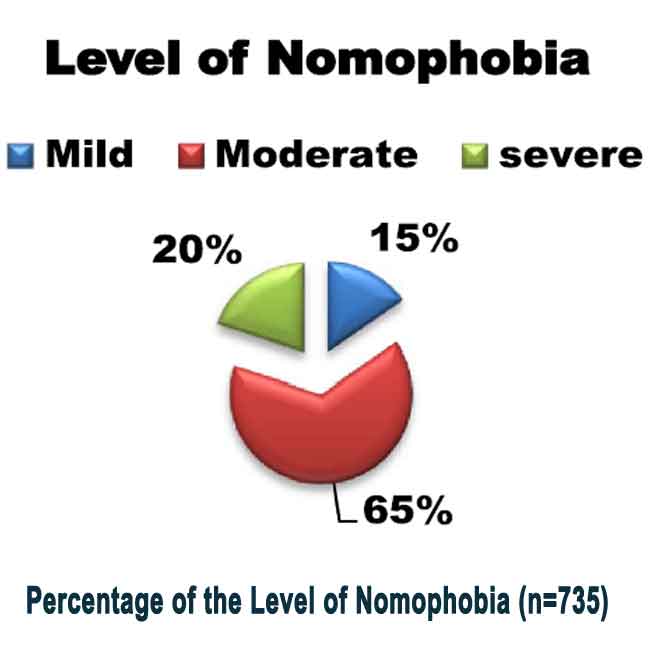
Prevalence of nomophobia
Nomophobia, or the fear of being without a mobile phone, affects a significant percentage of college students. Estimates range from 18.5% to 73%, depending on various factors. These factors include age, gender, self-image, self-esteem, self-efficacy, and impulsivity. People with nomophobia often keep their phones on at all times, even during sleep. Many carry an extra phone, charger, or battery as a backup in case they lose their device or run out of battery.
One study revealed that 95% of individuals use smartphones to watch YouTube, WhatsApp, or other media to help them fall asleep. Furthermore, 72% said they couldn’t be far from their phones and typically keep their devices within five feet. The prevalence of nomophobia is similar in both developed and developing countries, with estimates ranging from 77% to 99%, especially among young adults.

Nomophobia is not limited to adults; children and adolescents are equally susceptible to this phenomenon. Defined as the fear or anxiety associated with being separated from one’s mobile phone, it often manifests as an intense reliance on smartphones for social validation, entertainment, and a sense of security. It can result in various behavioral and emotional changes in young individuals.
Causes and predisposition for nomophobia
- Certain people are more susceptible to developing nomophobia. Factors that can accelerate the chances of developing the condition are the:
- Pre-existing anxiety
- Low self-esteem
- Struggles with emotional regulation
- Insecure attachment styles
- A lack of personal relationships
A variety of predisposing factors can influence nomophobia. These factors can vary from person to person, and the development of nomophobia often results from a combination of multiple influences.
Predisposing factors
- Smartphone Dependency: Excessive smartphone use and reliance on the device for communication, entertainment, and information can predispose individuals to nomophobia. The more dependent one becomes on their smartphone, the more likely they are to experience anxiety when separated from it.
- Attachment Style: People with anxious attachment styles may be more prone to nomophobia, which is characterized by a strong need for emotional closeness and reassurance. In this context, the smartphone often serves as a tool for seeking constant connection and validation. As a result, it can reinforce the need for continual reassurance.
- Social Media Usage: Heavy social media use and the pursuit of social validation online can contribute to nomophobia. Specifically, the constant craving for likes, comments, and interactions amplifies the fear of missing out. Consequently, this intensifies the desire to remain constantly connected.
- Accessibility and Availability of Technology: The ease of access to smartphones and the constant availability of technology can make it more likely for individuals to become dependent on their devices.
- FOMO (Fear of Missing Out): The fear of missing out on social events, news, or online interactions can be a powerful driver of nomophobia. Individuals who experience a strong FOMO are more likely to be anxious when not connected to their phones.
Psychological predisposing factors
- Previous Negative Experiences: Past negative experiences, such as missing important messages or events due to being without a phone, can contribute to the fear of being without one’s mobile device.
- Family or Cultural Factors: Family dynamics and cultural norms can influence smartphone usage and the development of nomophobia. In some cultures, constant connectivity may be emphasized, leading to greater phone dependency.
- High Stress and Anxiety Levels: Individuals experiencing high levels of stress and anxiety may be more susceptible to developing nomophobia. In these cases, the smartphone often becomes a tool for distraction and a coping mechanism for anxiety. Over time, this reliance on the device can grow, reinforcing the dependency.
- Low Self-Esteem: Individuals with low self-esteem may use their smartphones to boost their self-worth through social media validation. The fear of being without the device can be linked to a fear of losing this source of self-esteem.
- Peer Pressure: Social pressures and peer influence can play a significant role in developing nomophobia. If a person’s peers are constantly connected and expect them to be as well, it can create a fear of social exclusion.

11. Childhood Exposure: Early exposure to smartphones and mobile technology can impact a person’s attachment to these devices. Growing up with constant access to smartphones can contribute to a stronger dependency.
It’s important to note that these factors can interact and compound, leading to the development of nomophobia. Additionally, individual vulnerabilities and predispositions can vary, making each person’s experience of nomophobia unique. Understanding these predisposing factors can help address and manage nomophobia through awareness, self-regulation, and, if necessary, professional support.
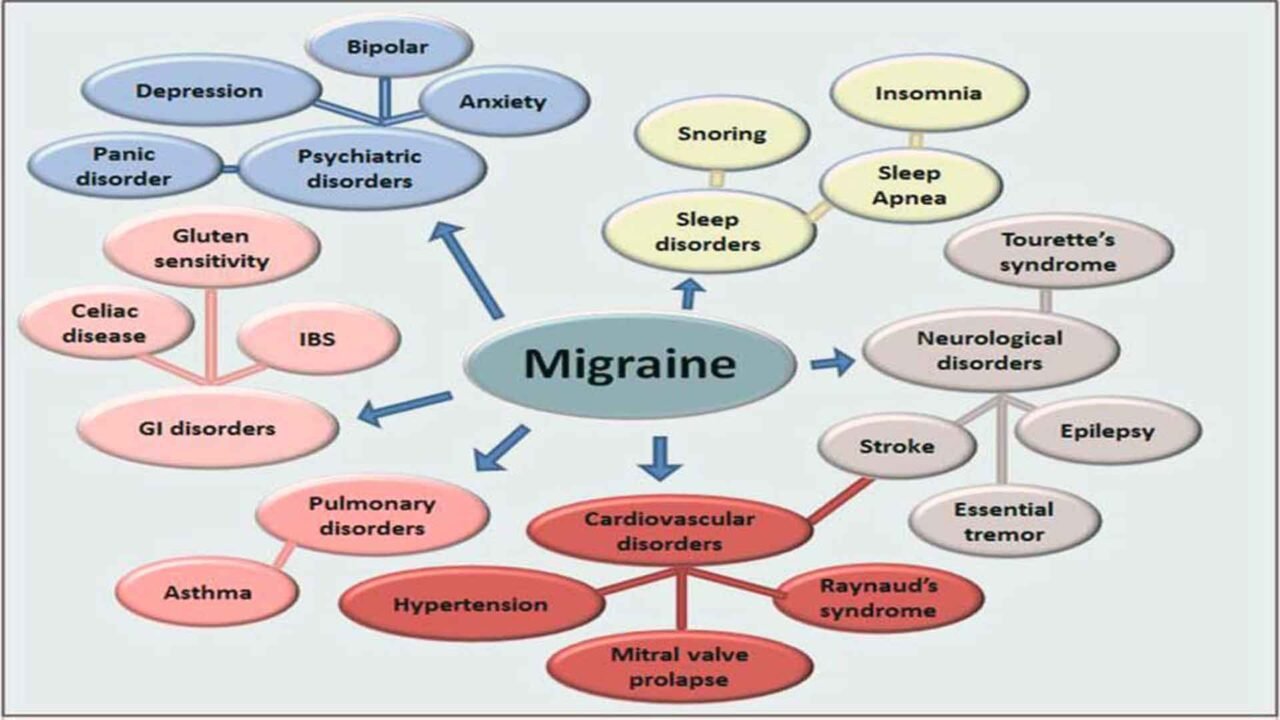
What mental conditions can contribute to and potentially accelerate development of nomophobia
Several mental health conditions and psychological factors can contribute to and potentially accelerate the development of nomophobia (the fear of being without one’s mobile phone). It’s important to note that these conditions may not directly cause nomophobia but can increase the likelihood and severity of the condition.
Mental health conditions
- Generalized Anxiety Disorder (GAD): Individuals with Generalized Anxiety Disorder (GAD) often experience excessive and uncontrollable worry about many areas of their lives. As a result, this chronic anxiety can increase their susceptibility to the fear and stress linked to being without their mobile phones. Consequently, the anxiety associated with separation from their phones may be heightened in those with GAD.
- Social Anxiety Disorder: Social anxiety often includes a fear of social interactions and judgment. In response, smartphones can act as a coping mechanism by offering a distraction and creating a buffer from direct social engagement. As a result, this reliance on phones can increase, potentially deepening the dependency on the device to avoid uncomfortable face-to-face interactions.
- Obsessive-Compulsive Disorder (OCD): Obsessive-Compulsive Disorder (OCD) is characterized by intrusive and distressing thoughts (obsessions) and repetitive behaviors or mental acts (compulsions). In this context, checking and rechecking the smartphone for messages or notifications can become a compulsive behavior. Consequently, this behavior can intensify the fear of being without the phone, reinforcing the cycle of dependence.
- Attention-Deficit/Hyperactivity Disorder (ADHD): ADHD is associated with challenges in impulse control and attention regulation. As a result, individuals with ADHD may be more prone to excessive smartphone use. Consequently, this increased usage can elevate the risk of developing nomophobia.
- Post-Traumatic Stress Disorder (PTSD): PTSD can lead to hypervigilance and heightened anxiety. In this scenario, constantly checking the smartphone may serve as a strategy to remain alert for potential threats. As a result, this behavior can contribute to increased phone dependence.
Psychological factors
- Depression: People with depression may turn to their smartphones for distraction and emotional relief. In this way, constant smartphone use can temporarily escape negative emotions. Consequently, this reliance on the device can develop into a dependency, further reinforcing its role in managing their emotional state.
- Substance Abuse Disorders: Individuals with substance abuse issues may use smartphones to connect with their support networks or to distract themselves from cravings and withdrawal symptoms. In this context, smartphones can become crucial for managing their condition. As a result, this can lead to a strong dependence on the device.
- Negative Body Image and Eating Disorders: Individuals with body image issues may use their phones for reassurance or distraction. In this context, the fear of being without a smartphone can be closely linked to the fear of confronting negative body image thoughts without a distraction. Thus, the reliance on the phone can intensify, serving as a way to avoid these distressing thoughts.
- Stress and Burnout: Chronic stress and burnout often require constant distraction and relief. As a result, individuals may turn to their smartphones excessively, seeking an escape from their stress and burnout. Consequently, this can lead to increased smartphone usage and dependence.
- Cyberbullying: Experiences of cyberbullying can lead to increased phone reliance, as individuals may want to stay informed about online threats or negative comments.
It’s essential to recognize that these mental health conditions can interact with individual vulnerabilities and other life circumstances, potentially accelerating the development of nomophobia. Therefore, treating and managing the underlying mental health condition is crucial, as is addressing smartphone dependency. By doing so, individuals can prevent or alleviate nomophobia. If you or someone you know is experiencing these mental health conditions along with smartphone-related anxieties, seeking professional help is advisable.
Impact of nomophobia to the health
Nomophobia can have various effects on an individual’s health, encompassing both mental and physical well-being. Here are some ways in which nomophobia can impact health.
Mental Health Impacts
- Increased Stress and Anxiety: The constant need to be connected and the fear of missing out can lead to heightened stress and anxiety levels. The anticipation of not having a mobile phone or being unable to check messages may induce a persistent state of anxiety.
- Sleep Disturbances: Excessive use of mobile phones, especially before bedtime, can disrupt sleep patterns. Screens emit blue light that can interfere with the production of melatonin, a hormone essential for sleep regulation, potentially leading to insomnia.
- Impaired Cognitive Function: Constantly checking messages and notifications can contribute to cognitive overload. This continuous cognitive stimulation may affect concentration, memory, and overall cognitive function.
- Social Isolation: Paradoxically, while mobile phones facilitate virtual connections, nomophobia can lead to social isolation. Individuals may withdraw from face-to-face interactions, relying more on digital communication, impacting social skills and relationships.
- Negative Impact on Mental Health: Over time, the fear of being without a mobile phone can contribute to the development or exacerbation of mental health conditions such as depression and social anxiety. It may also lead to a diminished sense of well-being.
Physical Health Impacts and Productivity Concerns
- Physical Health Issues: Using smartphones can contribute to physical health problems, including eye strain, neck and back pain (text neck), and repetitive strain injuries from prolonged phone use.
- Reduced Productivity: Nomophobia may lead to decreased productivity, as individuals may find it challenging to focus on tasks without the constant distraction of their phones. This can affect work and academic performance.
- Compromised Personal Relationships: Excessive phone use and the fear of separation from one’s device can strain personal relationships. For instance, individuals may prioritize their phones over face-to-face interactions, leading to misunderstandings and emotional distance. As a result, this shift in focus can affect the quality of personal connections and communication.

It is essential to recognize the potential health impacts of nomophobia and take proactive steps to foster a healthy relationship with technology.
What changes in behavior cause nomophobia
Nomophobia can lead to various changes in behavior. These behavioral changes can significantly impact an individual’s daily life, relationships, and well-being. Common behavioral changes associated with nomophobia include:
Behavioral Changes Affecting Daily Life
- Excessive Smartphone Use: People with nomophobia tend to use their smartphones excessively, often checking their devices for messages, notifications, or updates even when it’s not necessary. This behavior can lead to reduced productivity and increased distraction.
- Avoidance of Certain Situations: Individuals with nomophobia may avoid situations or places where they know they won’t have phone signals or access to their phones. This can affect their willingness to engage in social activities, travel, or attend events.
- Reduced Face-to-Face Social Interaction: Excessive phone use can decrease in-person social interactions. People with nomophobia may prioritize virtual connections over real-world relationships, impacting their ability to build and maintain meaningful connections with others.
- Increased Anxiety and Stress: Constantly checking the phone for messages or updates can lead to heightened anxiety and stress levels. This behavior can respond to the fear of missing out (FOMO) on important information or social interactions.
- Sleep Disruption: Smartphones, often associated with nomophobia, can disrupt sleep patterns before bedtime. Blue light emitted by screens can interfere with the body’s production of melatonin, a hormone that regulates sleep, leading to insomnia or poor sleep quality.
- Impaired Concentration and Productivity: Frequent phone checking and social media use can make it difficult for individuals to focus on tasks, whether at work or school, reducing productivity and concentration. Some research has found a strong association between academic performance and nomophobia and shows weaker academic performance among students with severe nomophobia.
Safety Concerns and Relationship Impact
- Distraction While Driving: Nomophobia can lead to dangerous behavior, such as using a smartphone while driving. Distracted driving is a significant safety concern and can lead to accidents.
- Negative Impact on Mental Health: The constant need to be connected can contribute to feelings of loneliness, depression, and anxiety. This behavioral change can have long-term consequences for mental well-being.
- Relationship Issues: Nomophobia can strain personal relationships, as partners or family members may feel neglected or frustrated when someone is more focused on their phone than on spending time with loved ones.
- Difficulty Disconnecting: People with nomophobia often find it challenging to disconnect from their phones, even during vacations or leisure time. This can prevent them from fully enjoying moments of relaxation.
It’s important to recognize these behavioral changes associated with nomophobia, as they can negatively impact an individual’s quality of life.
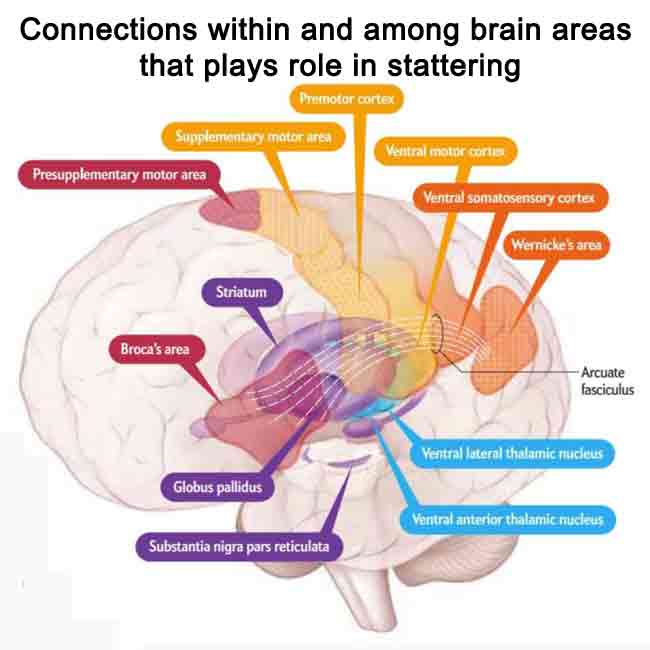
What changes in brain and its function cause nomophobia
There is ongoing research into the specific changes in the brain that may be associated with nomophobia. However, some research suggests that the fear and anxiety associated with nomophobia may be linked to changes in brain activity and neurochemistry, similar to other forms of addiction or anxiety disorders. Here are some potential brain-related factors:
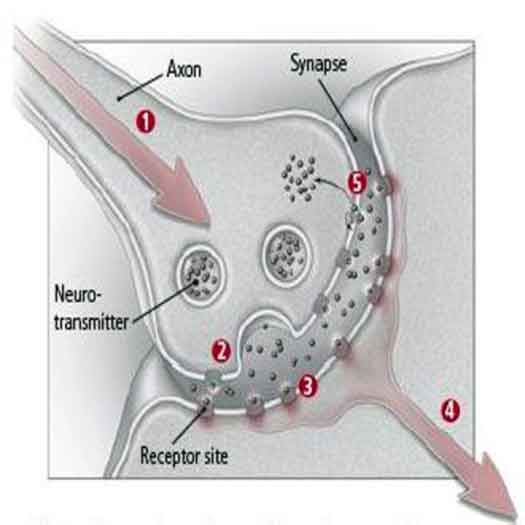
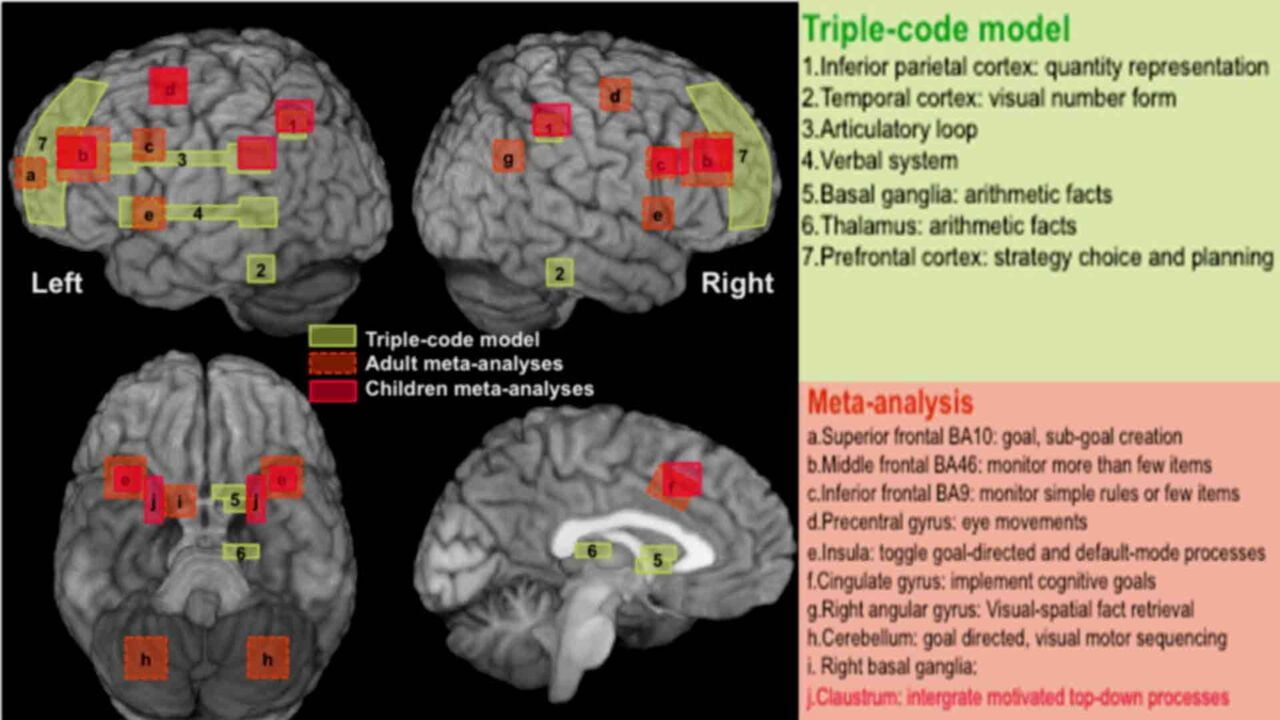
Neurochemical and Brain Activity Changes
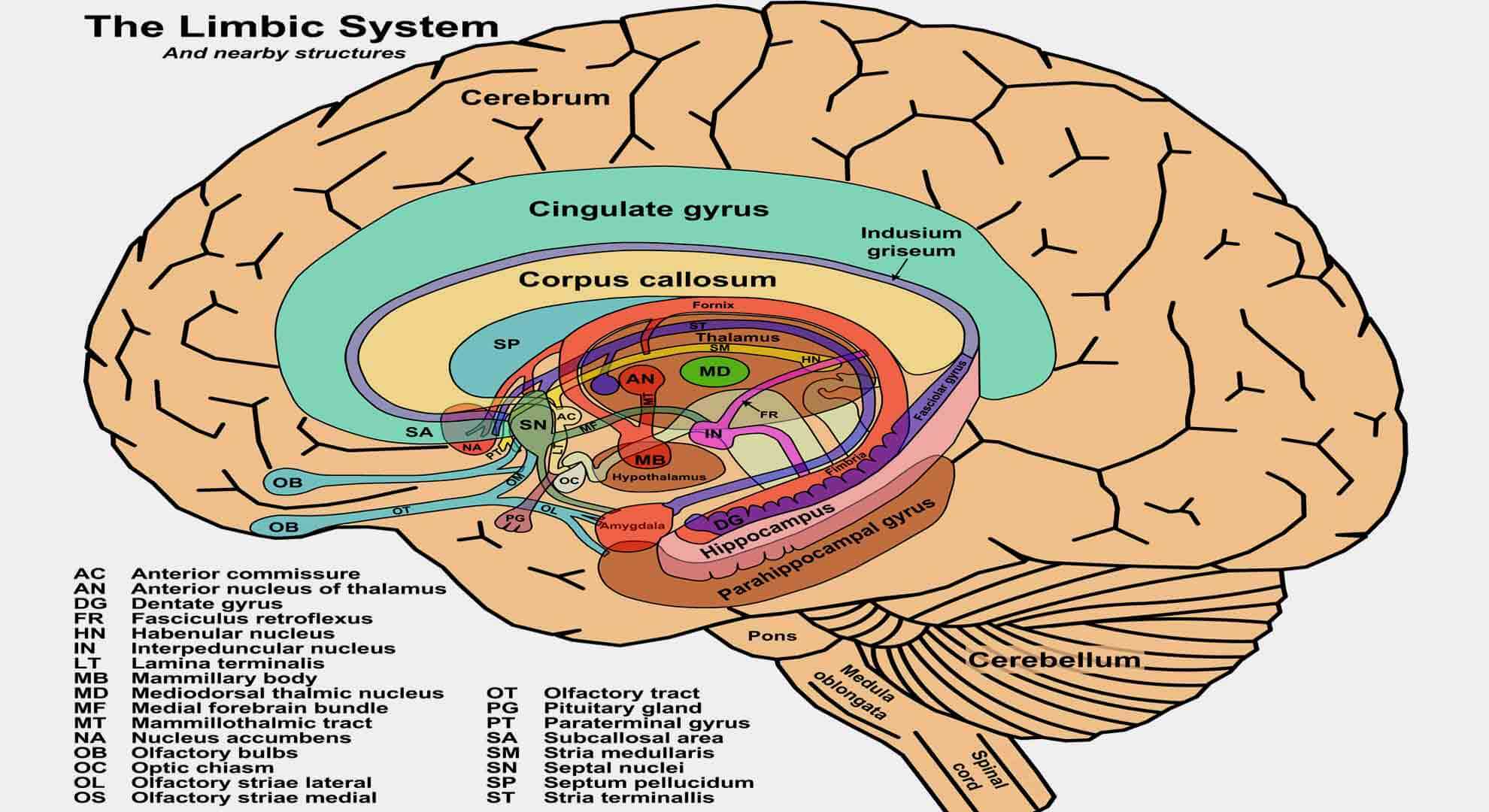
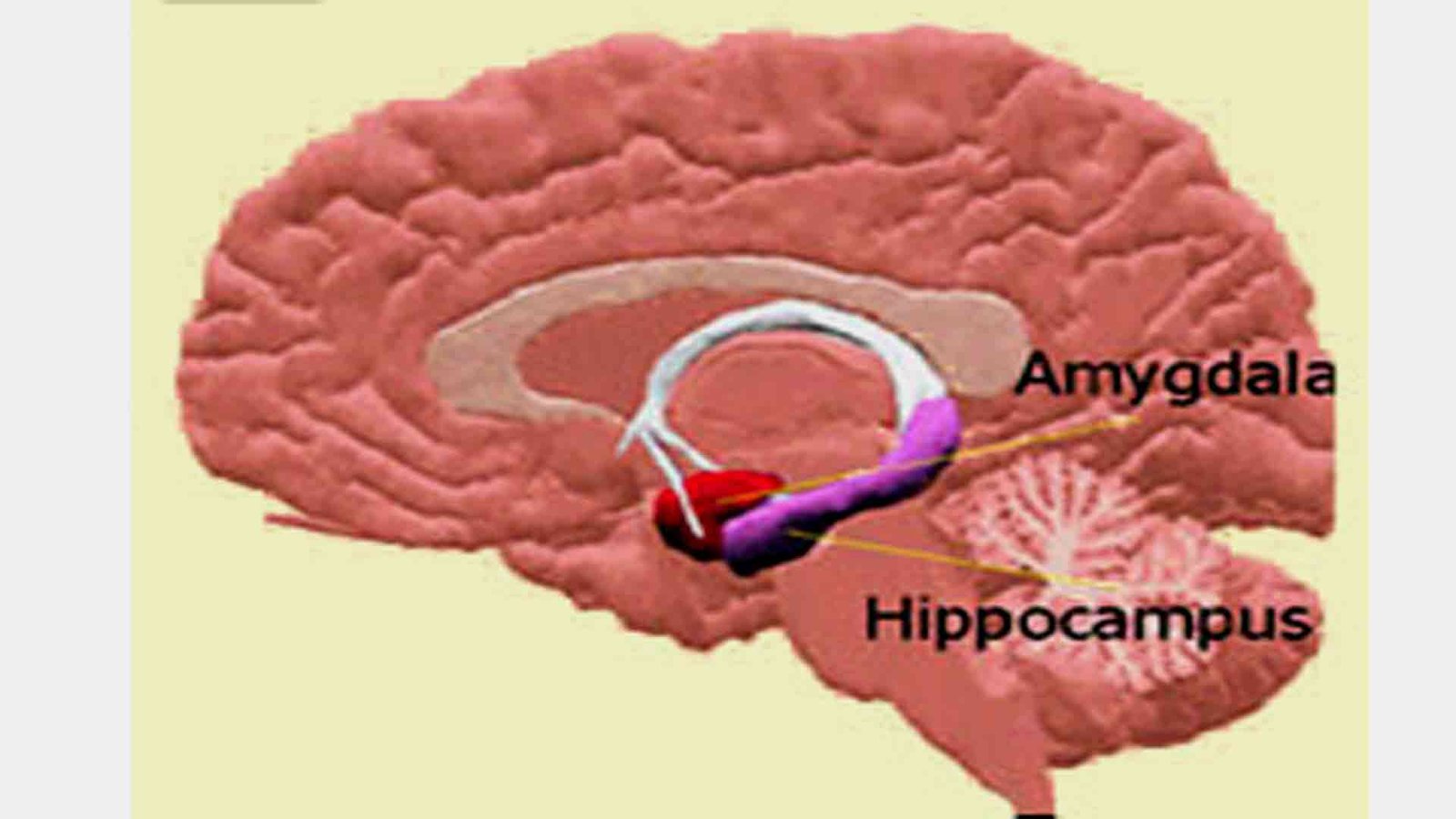
1. Dopamine Release: When individuals receive notifications or messages on their phones, their brain releases dopamine. This neurotransmitter is linked to pleasure and reward. Over time, excessive smartphone use can change the brain’s reward system. As a result, people may become more dependent on their phones for these pleasurable experiences.
2. Cortisol Levels: The constant need to check and respond to messages, notifications, or social media updates can create a sense of pressure and stress, leading to increased levels of the stress hormone cortisol in the brain. Chronic stress can have negative effects on brain health.
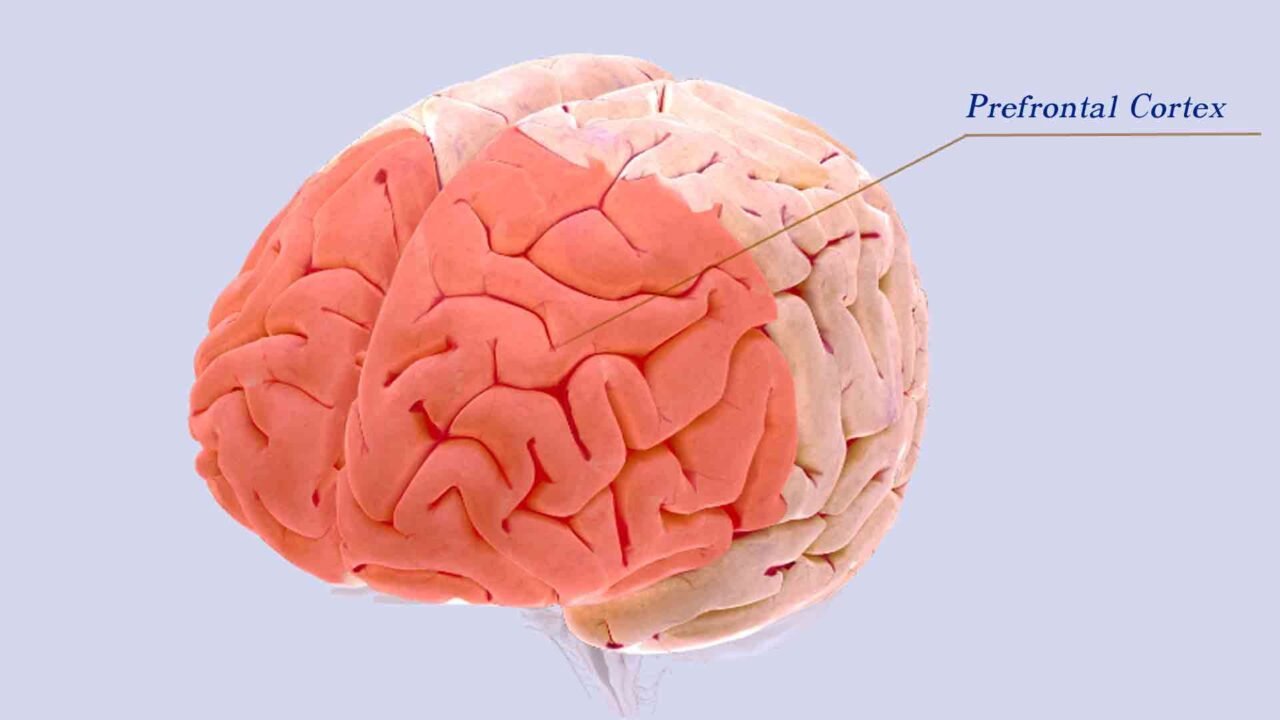
3. Prefrontal Cortex Activity: The prefrontal cortex involves decision-making and impulse control. Excessive smartphone use may alter the functioning of this region, making it harder for individuals to resist the urge to check their phones constantly.
4. Altered Sleep Patterns: Overuse of smartphones, especially at night, can disrupt sleep patterns due to the blue light emitted by screens. Sleep disruption can affect cognitive functions and mood regulation.
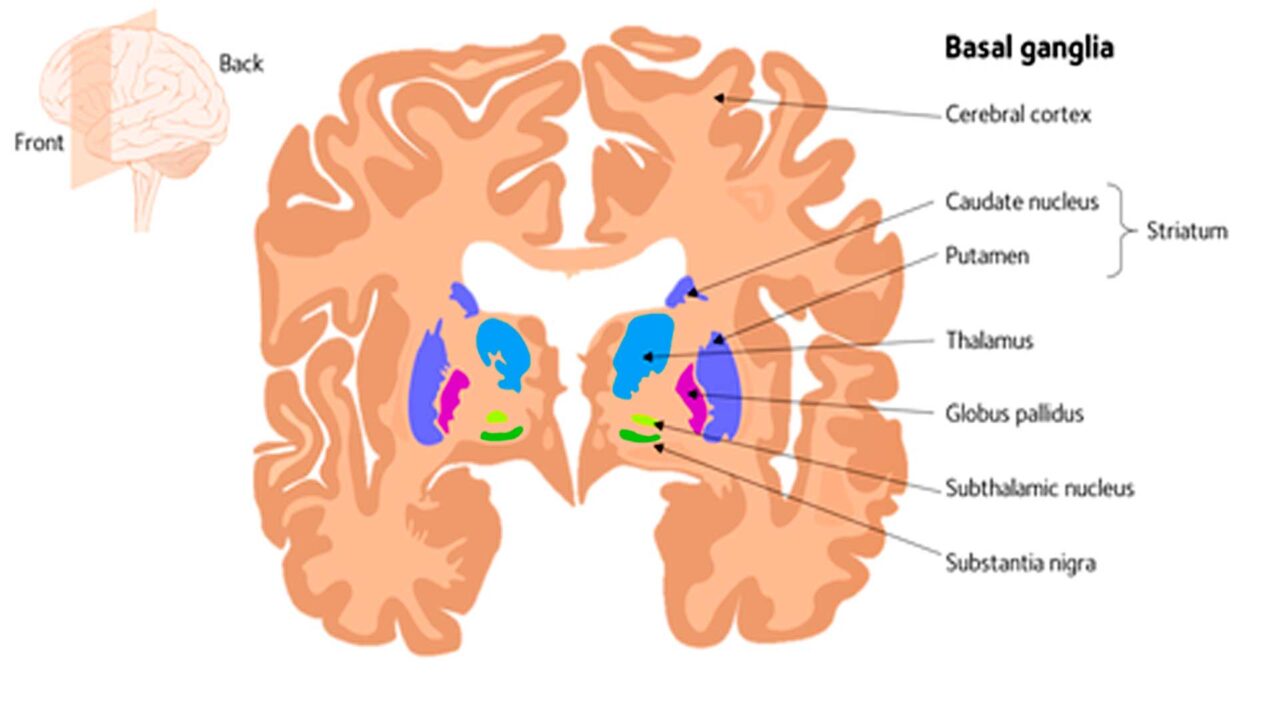
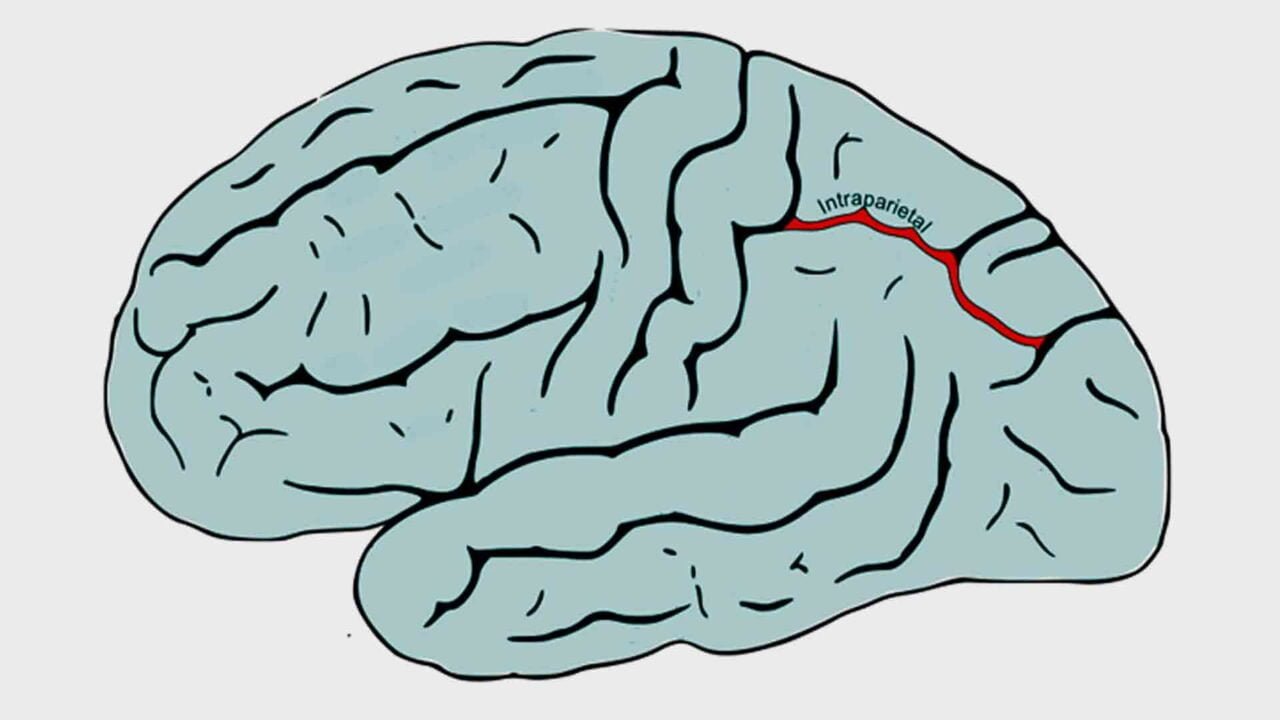
Structural Brain Changes and Neuroplasticity
- Gray Matter Atrophy
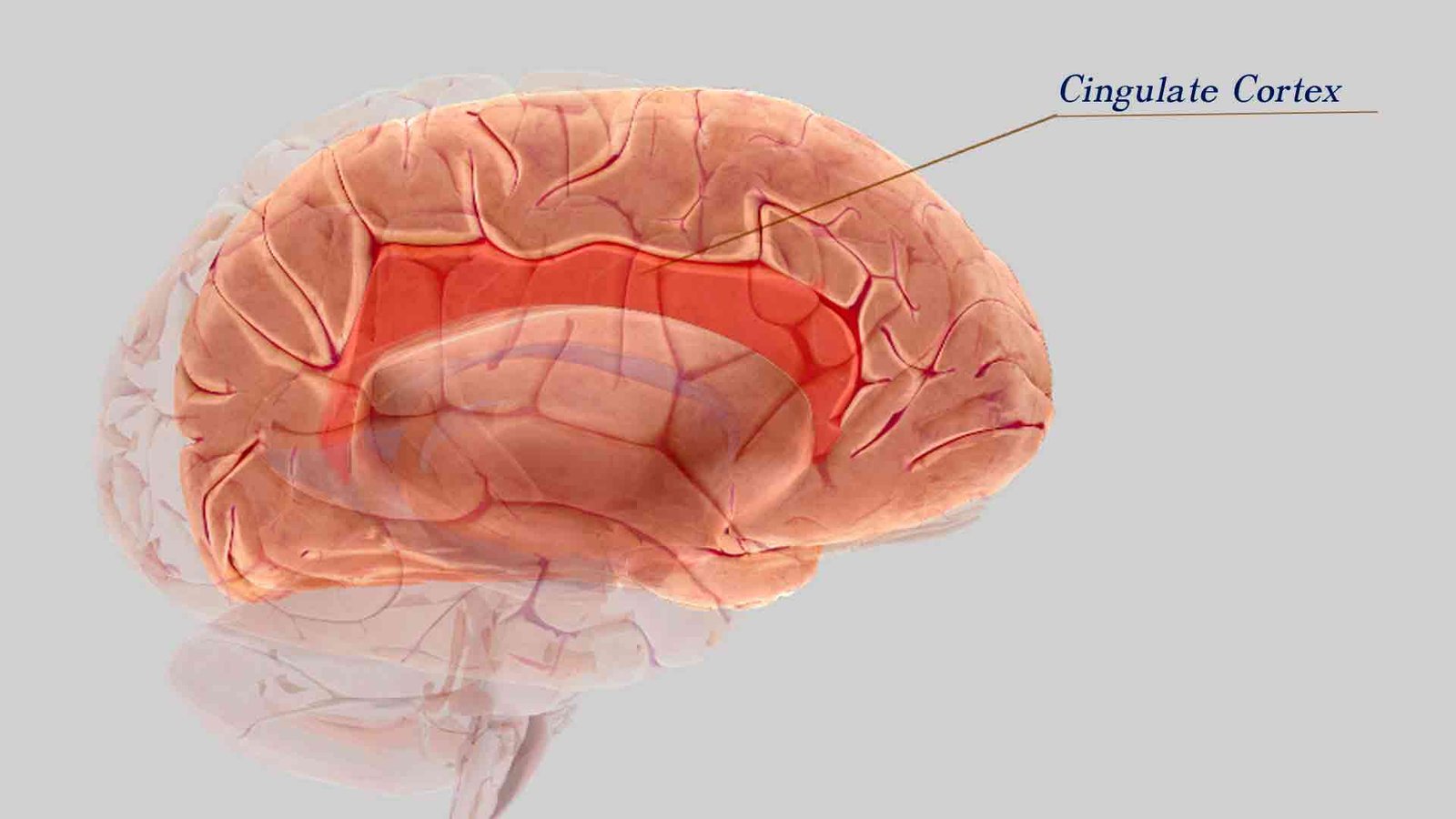
Research has indicated atrophy (shrinkage or tissue volume loss) related to the brain’s reward pathways in gray matter areas. Notable volume loss was observed in the striatum, which is involved in reward processing and impulse control. - Damage to the Insula
Damage to the insula, an area involved in empathy, compassion, and integrating physical signals with emotion, has been linked to nomophobia. This damage can affect personal relationships and emotional depth. - Neuroplasticity: The brain is highly adaptable and can rewire itself based on repeated behaviors. If a person is constantly engaged with their smartphone, the brain may reorganize its neural connections to prioritize this behavior, potentially at the expense of other essential activities and interactions.
- Individual Variability
The specific neural changes associated with nomophobia can vary from person to person. More research is needed to fully understand the neurological aspects of nomophobia and how excessive smartphone use affects brain function and mental health.
It’s important to note that these changes are not unique to nomophobia but are generally related to excessive smartphone use. The specific neural changes associated with nomophobia may vary from person to person, and more research is needed to fully understand this phenomenon’s neurological aspects. Additionally, the impact of excessive smartphone use on brain function and mental health can vary depending on the individual and the extent of their phone dependency.
Prevention of nomophobia development
Preventing or proactively addressing nomophobia (the fear of being without one’s mobile phone) involves a combination of awareness, self-regulation, and healthy technology habits. Here are some strategies for nomophobia prophylaxis:
Strategies for Managing Smartphone Use
1. Digital Detox Days: Designate regular “digital detox” days where you intentionally disconnect from your smartphone and other devices. This can help you become less reliant on your phone for entertainment and social interaction.
2. Set Boundaries: Establish clear boundaries for smartphone use. For example, avoid using your phone during meals, in the bedroom, or other essential activities. Stick to these boundaries to prevent excessive phone use.
3. Silent Hours: Designate certain hours of the day as “silent hours” where you turn off or silence your phone. This can provide a break from notifications and constant connectivity.
4. Selective Notifications: Customize your smartphone’s notification settings. Turn off non-essential notifications or set them to “Do Not Disturb” during specific hours to reduce constant interruptions.
5. Offline Activities: Engage in offline activities that you enjoy, such as hobbies, exercise, or face-to-face social interactions. These activities can help reduce the time spent on your phone.
6. Digital Well-Being Tools: Many smartphones offer digital well-being features that can help you track and manage your screen time. Use these tools to set daily limits on app usage.
7. Mindfulness and Relaxation: Practice mindfulness and relaxation techniques to manage stress and anxiety without relying on your phone. This can help reduce the need to check your device constantly.
Proactive Measures and Support
- Self-Awareness: Reflect on your smartphone usage and its impact on your daily life. Recognize the situations or emotions that trigger your nomophobia and work on addressing them.
- Seek Support: If nomophobia is significantly affecting your life and well-being, consider seeking support from a mental health professional or a therapist. They can help you explore the root causes and develop coping strategies.
- Parental Guidance: Parents are crucial in preventing nomophobia in children and adolescents. They should set limits on screen time, educate them about the potential negative effects of excessive smartphone use, and encourage a healthy balance between online and offline activities.
- Education: Stay informed about the potential risks of excessive smartphone use and educate yourself about digital well-being. The more you know about technology’s impact on your life, the better equipped you are to make informed choices.
- Role Modeling: Be a role model for responsible smartphone use. Children and adolescents often learn by observing the behavior of adults, so demonstrate a healthy relationship with your phone.
Prophylaxis for nomophobia involves taking a balanced and mindful approach to smartphone usage. It involves understanding the role of technology in your life, recognizing the signs of dependency, and actively taking steps to maintain control over your digital habits. By implementing these strategies, you can reduce the risk of developing nomophobia or mitigate its effects if you’re already experiencing it.
Preventing nomophobia in children
To prevent nomophobia in children, it is necessary to establish healthy digital habits, foster responsible technology use, and promote a balanced relationship with smartphones and other devices. Here are some strategies for preventing nomophobia in young individuals:
Building Healthy Digital Habits
1. Educate About Digital Well-Being:
Start by educating children and adolescents about the potential risks of excessive smartphone use, including the development of nomophobia. Teach them to recognize the signs of smartphone dependency.
2. Set Screen Time Limits:
Establish daily screen time limits for the recreational use of smartphones and other devices. Consider using parental control apps or built-in features to enforce these limits.
3. Create Tech-Free Zones:
Designate specific areas in the home where smartphone use is not allowed, such as the dinner table, bedrooms, and study areas. These zones promote face-to-face interactions and better sleep habits.
4. Encourage Outdoor Activities:
Promote outdoor activities, physical exercise, and hobbies that do not involve screens. Encourage children and adolescents to explore the natural world and engage in physical play.
5. Model Responsible Behavior:
Be a positive role model by demonstrating responsible smartphone use. Show that you can disconnect from your phone and prioritize in-person interactions.
6. Open Communication:
Create an open and non-judgmental environment where children and adolescents can discuss their feelings and experiences related to smartphone use. Encourage them to talk about any anxieties or insecurities they may have.
7. Teach Time Management:
Help children and adolescents develop practical time management skills. Teach them how to allocate time for homework, chores, relaxation, and digital entertainment.
8. Set Tech-Free Bedtime Rituals:
Establish tech-free bedtime rituals to help children and adolescents unwind and prepare for restful sleep. Encourage them to leave their phones outside the bedroom to avoid sleep disruption.
Enhancing Social and Emotional Well-Being
1. Monitor Online Activity:
Keep an eye on your child’s online activity, especially on social media platforms. Be aware of any cyberbullying or negative experiences that may contribute to anxiety.
2. Limit Social Media Comparison:
Discuss the potentially harmful effects of comparing oneself to others on social media. Teach children and adolescents to appreciate their uniqueness and self-worth.
3. Teach Digital Literacy:
Promote digital literacy and critical thinking skills. Help young individuals recognize and evaluate the credibility of online information.
4. Encourage Offline Social Interactions:
Foster opportunities for children and adolescents to interact with peers in person. Encourage group activities, playdates, and involvement in clubs or sports.
5. Reward Offline Achievements:
Recognize and reward offline achievements, such as academic success, sports accomplishments, or creative endeavors. Celebrate non-digital milestones.
6. Seek Professional Help if Necessary:
If you notice signs of nomophobia or severe smartphone dependency in a child or adolescent, seek the guidance of a mental health professional. They can provide specialized support and intervention.
Preventing nomophobia in children and adolescents requires a holistic approach that combines awareness, parental involvement, education, and cultivating a balanced digital lifestyle. Parents and caregivers can help young individuals develop healthy relationships with technology and reduce the risk of experiencing nomophobia by taking proactive steps and providing guidance.
You can check if you have nomophobia by answering this questionnaire.
What is nomophobia treatment?
Treatment for nomophobia, like treatment for other technology-related behavioral issues, focuses on reducing dependency, managing anxiety, and establishing healthier habits around smartphone use. Here are some strategies and treatments that can help address nomophobia:
Therapeutic Approaches for Nomophobia
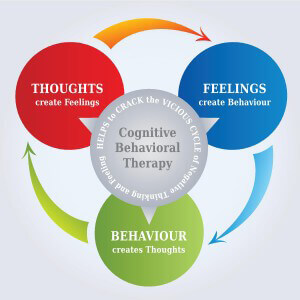
1. Cognitive-Behavioral Therapy (CBT): CBT is a common therapeutic approach for treating anxiety disorders. A therapist can work with individuals to identify and challenge irrational thoughts and behaviors related to their smartphone use and fear of being without it.
2. Exposure Therapy: This type of therapy involves gradually exposing individuals to situations where they would typically experience anxiety due to being without their phone. Over time, this can help desensitize them to the fear.
3. Mindfulness and Relaxation Techniques: Learning mindfulness and relaxation exercises can help individuals manage anxiety and stress associated with nomophobia. Breathing exercises, meditation, and yoga can be beneficial.
4. Coping Skills Training: Therapists can teach individuals healthy coping mechanisms to deal with the fear of being without their phone. This may include identifying alternative activities and strategies for managing anxiety.
5. Setting Boundaries: Establishing clear boundaries for smartphone use is essential. This can involve creating designated “phone-free” times or places, such as during meals or in the bedroom.
6. Digital Detox: Periodically disconnecting from the smartphone for an extended period can help break the cycle of dependency. Some individuals may benefit from technology-free weekends or vacations.
Additional Strategies and Support
1. Support Groups: Joining support groups or seeking the support of friends and family who understand the issue can be beneficial. Sharing experiences and strategies for managing smartphone use can provide a sense of community and accountability.
2. Behavioral Interventions: Behavior modification techniques, such as reward systems for reducing smartphone use, can be effective. Positive reinforcement for meeting goals can help individuals gradually reduce their phone attachment.
3. Educational Workshops: Some organizations and mental health professionals offer workshops or educational sessions on digital well-being and smartphone addiction. These can provide information and tools to manage smartphone use effectively.
4. Self-Help Apps: Various smartphone apps help individuals track and manage their phone usage. These apps can provide insights into usage patterns and help set limits.
5. Consultation with a Mental Health Professional: If nomophobia significantly impacts an individual’s life and well-being, it may be advisable to consult with a mental health professional, such as a psychologist or psychiatrist, for a personalized treatment plan.
Treatment for nomophobia should be tailored to the individual’s specific needs and the severity of the condition. It’s important to remember that addressing nomophobia is not about eliminating smartphone use but about finding a healthy balance and reducing the negative impact of excessive phone dependency on one’s life.
Biofeedback in nomophobia treatment
Biofeedback is a therapeutic technique that helps individuals gain awareness and control over physiological processes in their bodies, such as heart rate, muscle tension, and skin conductance. While biofeedback is not typically used as a direct treatment for nomophobia, it can be a valuable component of a broader treatment plan aimed at managing anxiety and stress, which are often associated with nomophobia. Here’s how biofeedback can be integrated into the treatment of nomophobia:
Integrating Biofeedback into Nomophobia Treatment
1. Stress Management: Nomophobia is often accompanied by stress and anxiety. Biofeedback can teach individuals how to recognize and reduce the physiological signs of stress, such as increased heart rate and muscle tension. By learning to control these responses, individuals can better manage the anxiety that can trigger their dependence on their smartphones.
2. Self-Regulation: Biofeedback helps individuals develop self-regulation skills. By monitoring their physiological responses in real time, they can learn to control their responses consciously. This can be particularly useful for individuals who experience anxiety when separated from their phones.
3. Relaxation Techniques: Biofeedback training often involves teaching relaxation techniques, such as deep breathing and progressive muscle relaxation. These techniques can counter the anxiety and restlessness associated with nomophobia.
4. Awareness: Biofeedback can enhance awareness of one’s physiological responses to stress, including the physical sensations that may accompany nomophobia. This increased awareness can help individuals recognize their anxiety triggers and develop strategies to cope with them.
Tools and Integration
1. Biofeedback Apps and Wearables: Biofeedback apps and wearable devices can measure and provide real-time feedback on physiological parameters. These tools can help individuals track and manage their stress and anxiety, making it easier to address the emotional aspects of nomophobia.
2. Integration with Other Therapies: Biofeedback can be integrated into a broader treatment plan that includes cognitive-behavioral therapy (CBT) or exposure therapy, which are commonly used to address anxiety-related issues like nomophobia. Biofeedback can complement these therapies by helping individuals manage the physical symptoms of anxiety.
3. Comprehensive Approach
Biofeedback should be part of a broader treatment plan rather than a standalone solution for nomophobia. Mental health professionals can help integrate biofeedback with other therapeutic approaches to address both psychological and emotional aspects of nomophobia.
It’s important to note that biofeedback is not a standalone treatment for nomophobia but rather a component of a comprehensive approach. A mental health professional, such as a therapist or psychologist, can work with individuals to determine how best to integrate biofeedback into their treatment plan and address the psychological and emotional aspects of nomophobia. The goal is to help individuals manage their anxiety and stress in healthier ways, ultimately reducing their dependency on their smartphones.
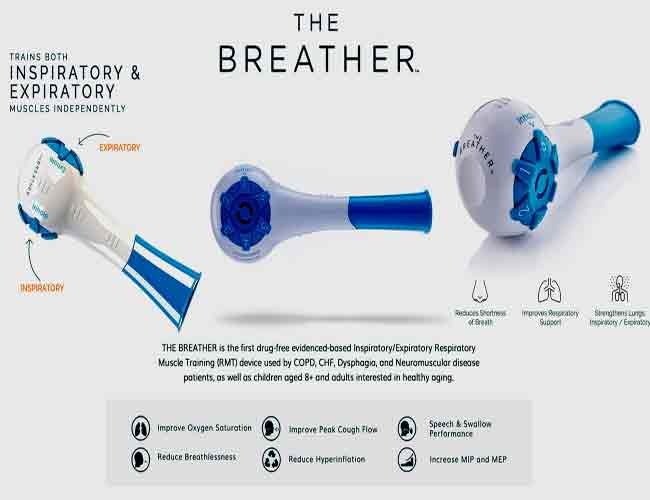
What biofeedback modalities can be used for nomophobia treatment?
Various modalities of biofeedback can be used, and the choice of modality depends on the specific physiological factors contributing to an individual’s nomophobia. Here are some common biofeedback modalities and how they can be used:
Common Biofeedback Modalities
1. Heart Rate Variability (HRV) Biofeedback:
- How it works: HRV biofeedback measures the variations in time between successive heartbeats. It reflects the balance between the autonomic nervous system’s sympathetic (fight or flight) and parasympathetic (rest and digest) branches.
- Relevance to nomophobia treatment: Many individuals with nomophobia experience increased heart rate and a “fight or flight” response when separated from their phones or experiencing phone-related anxiety. HRV biofeedback can help individuals learn to regulate their autonomic nervous system, reduce heart rate, and promote relaxation.
2. Electrodermal Activity (EDA) Biofeedback:
- How it works: EDA biofeedback measures skin conductance or sweat gland activity. It reflects the activity of the sympathetic nervous system, which is responsible for the body’s stress response.
- Relevance to nomophobia treatment: People with nomophobia often experience increased sweat gland activity when they are anxious about being without their phones. EDA biofeedback can help individuals recognize and control these physiological responses, leading to decreased anxiety and improved stress management.
- How it works: Respiration biofeedback involves monitoring and controlling one’s breathing patterns. It helps individuals achieve a balanced and controlled breathing rate.
- Relevance to nomophobia treatment: Anxiety often leads to shallow and rapid breathing. Respiration biofeedback can teach individuals to slow and engage in deep, diaphragmatic breathing, which triggers the body’s relaxation response. This can help counteract the stress response associated with nomophobia.
Additional Biofeedback Modalities
- How it works: Temperature biofeedback measures skin temperature, influenced by blood flow and circulation. It is linked to the body’s relaxation response.
- Relevance to nomophobia treatment: Stress and anxiety can lead to peripheral vasoconstriction (reduced blood flow to the extremities), resulting in cold hands and feet. Temperature biofeedback can help individuals increase peripheral blood flow and warm their extremities, promoting relaxation and reducing the physical symptoms of anxiety.
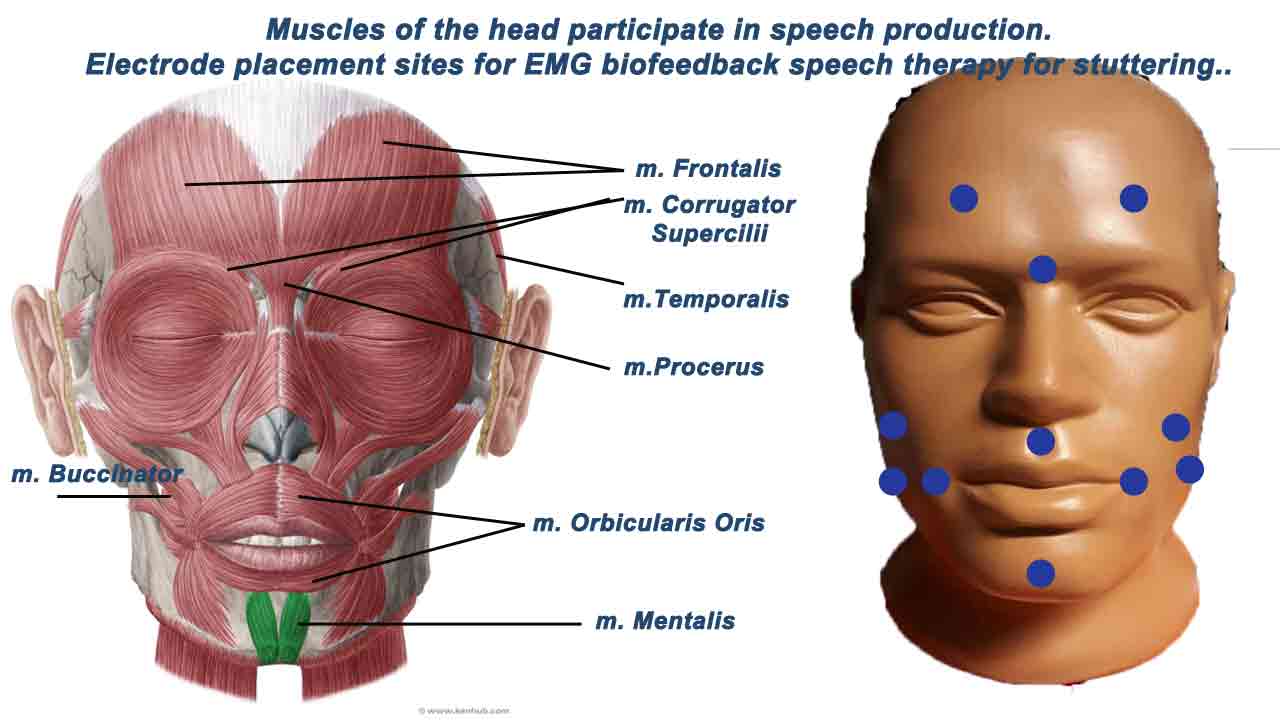
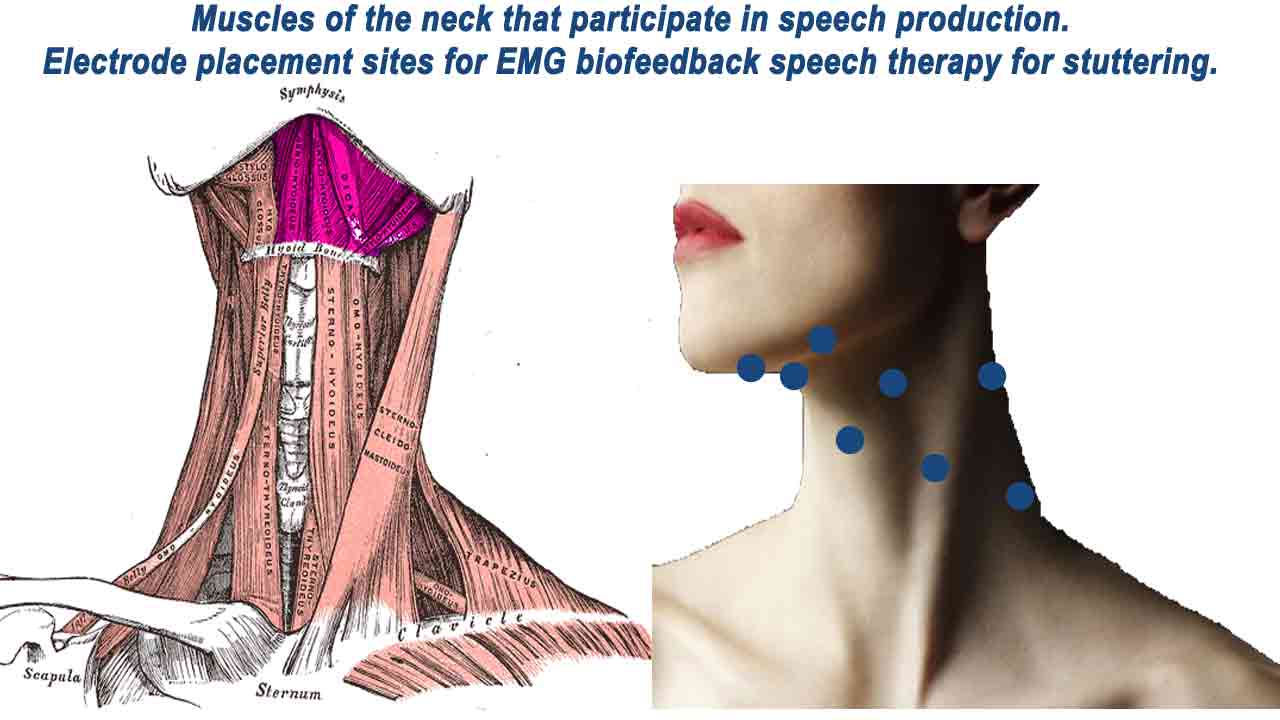
2. Muscle Electromyography (EMG) Biofeedback in nomophobia treatment:
- How it works: EMG biofeedback measures muscle tension and provides feedback on muscle activity.
- Relevance to nomophobia treatment: People with nomophobia may experience muscle tension and physical discomfort when separated from their phones or when they experience anxiety related to phone use. EMG biofeedback can help individuals recognize and reduce muscle tension, promoting physical relaxation.
The biofeedback modality for treating nomophobia should be based on an individual’s physiological responses and needs. In therapy, a trained professional can conduct an assessment to determine which modality would be most effective. The goal of using biofeedback is to increase self-awareness, develop self-regulation skills, and reduce the physiological markers of anxiety and stress, ultimately helping individuals manage their nomophobia-related symptoms more effectively.
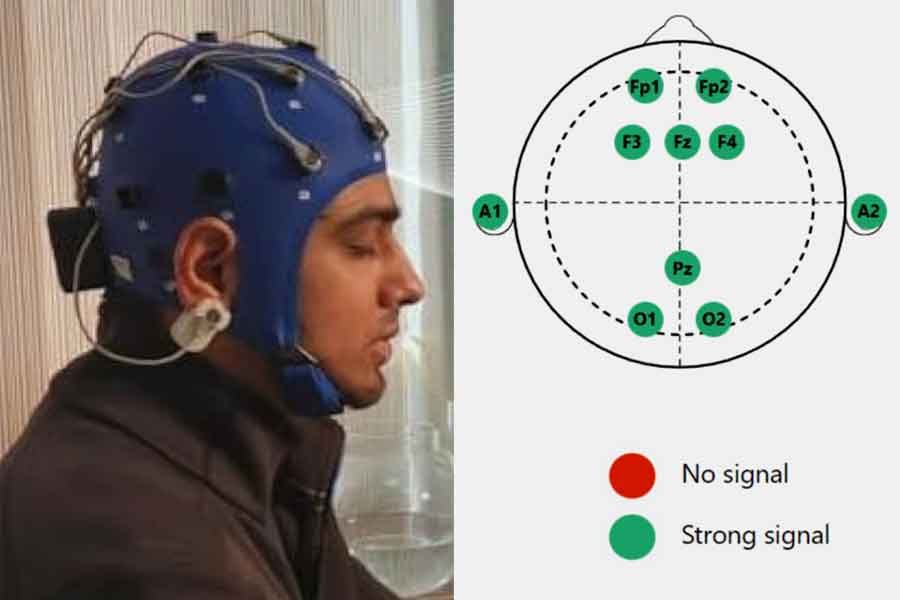
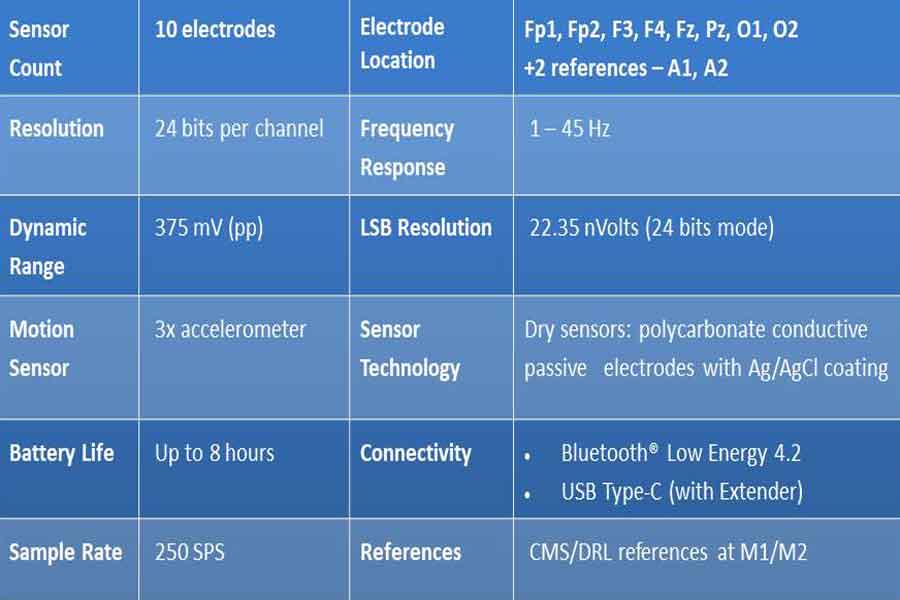
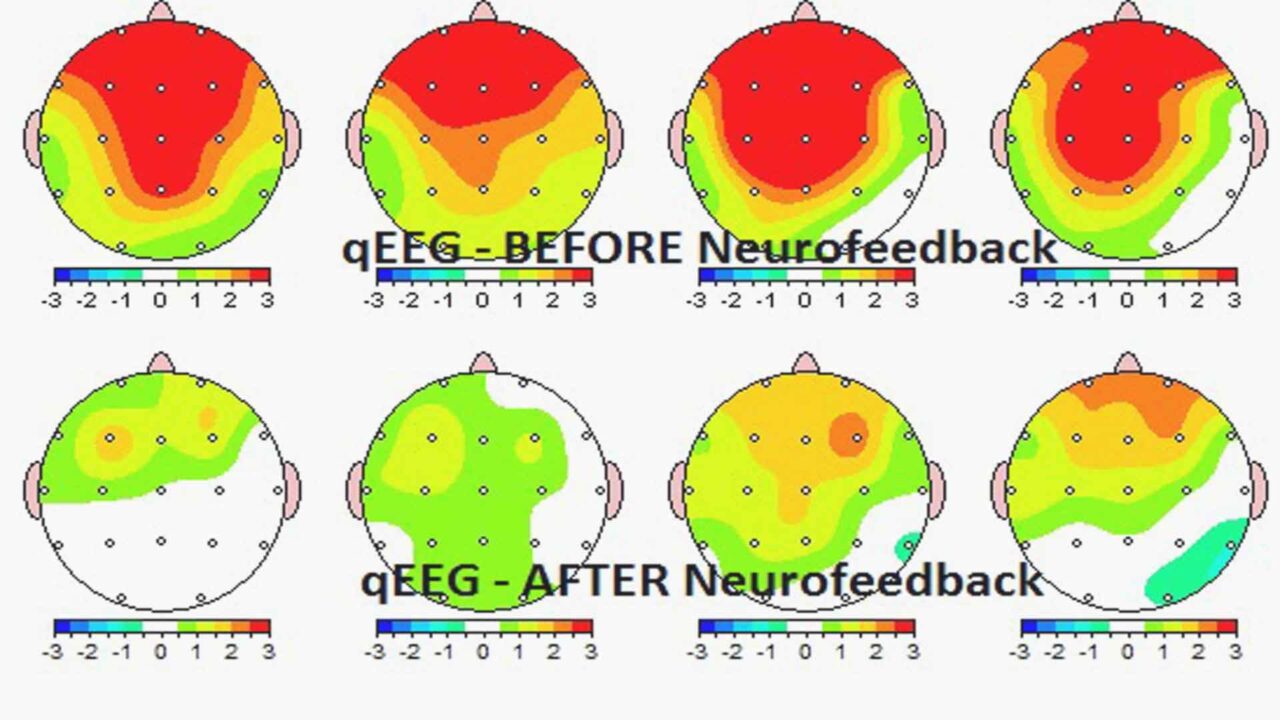
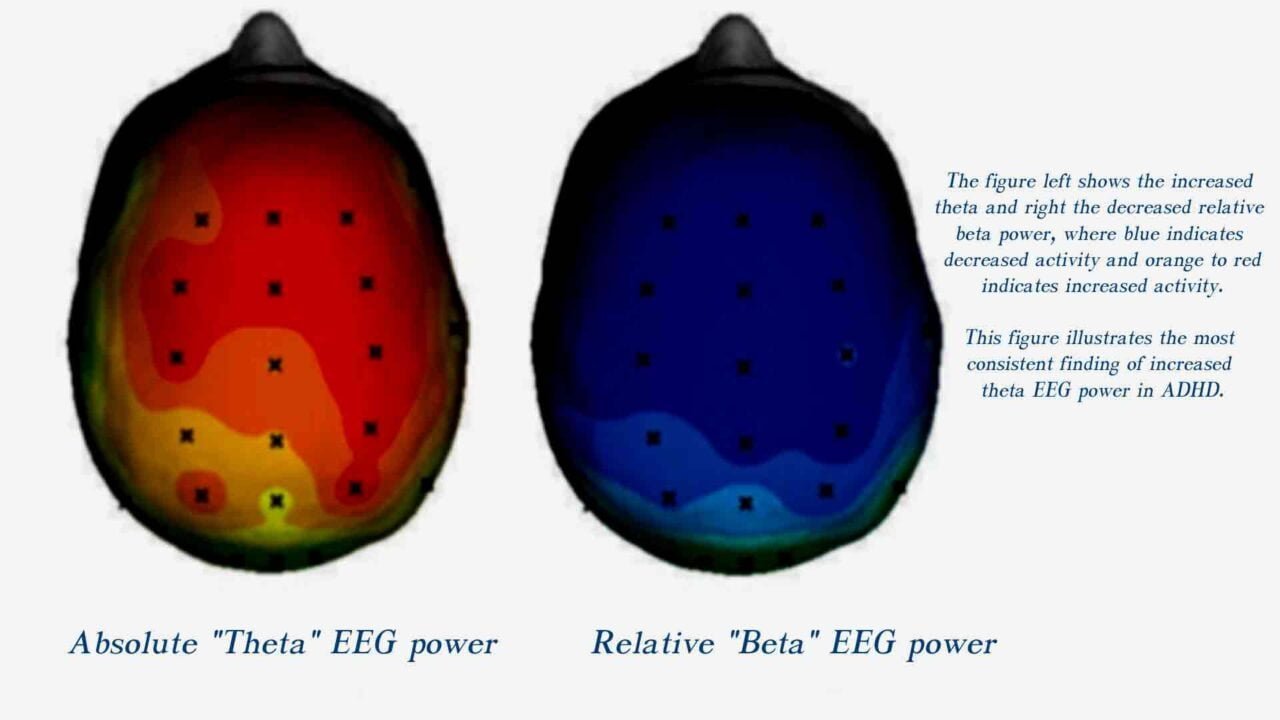
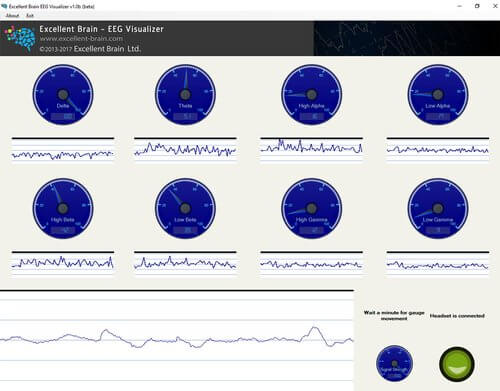
EEG (Electroencephalography) biofeedback in nomophobia treatment
EEG (Electroencephalography) biofeedback, also known as neurofeedback, is a therapeutic technique that involves real-time monitoring of brainwave activity to provide individuals with information about their brain functioning. Although researchers have only recently started applying EEG biofeedback specifically for nomophobia, they can explore the general principles of qEEG-based neurofeedback to manage the underlying factors contributing to the condition.
Here’s how EEG biofeedback could be considered for the treatment of nomophobia:
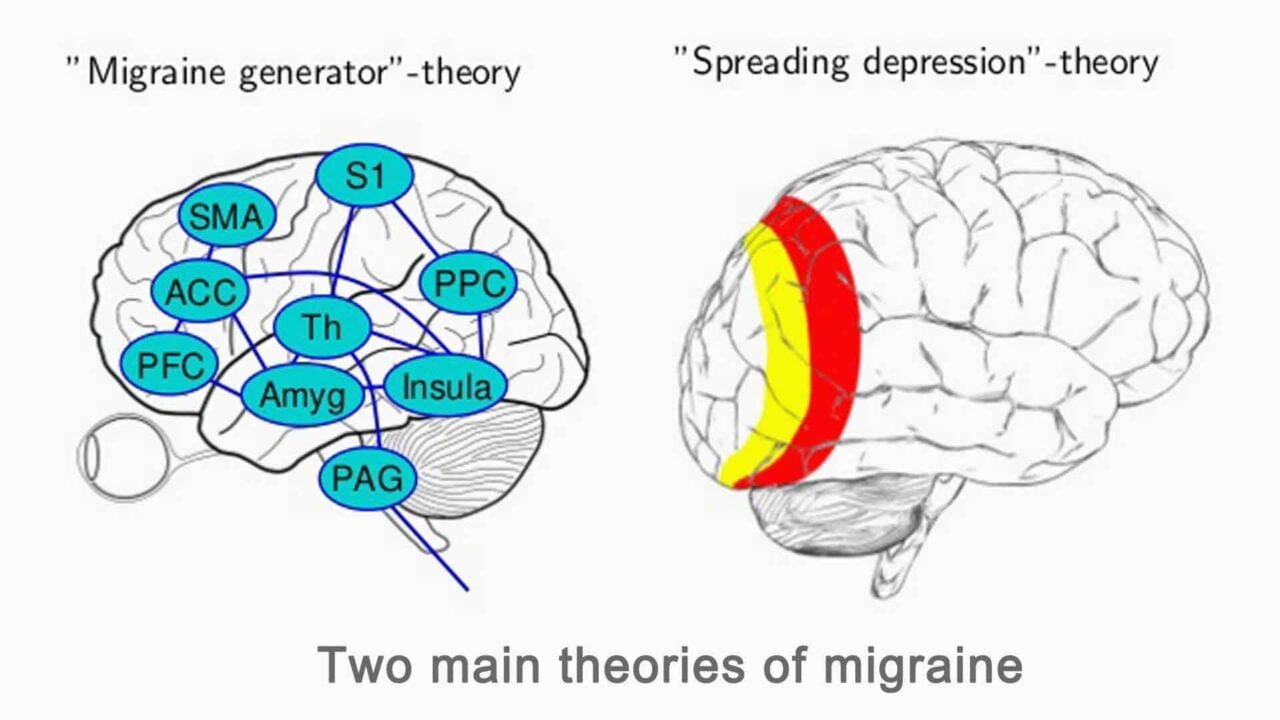
Understanding Brain Activity in Nomophobia:
1. Identifying Stress Patterns:
- EEG biofeedback allows for identifying specific brainwave patterns associated with stress and anxiety.
- Nomophobia often involves heightened stress responses when individuals are separated from their phones. EEG can pinpoint these stress-related brainwave patterns.
2. Neurological Correlates of Nomophobia:
- Research could be conducted to identify neurological correlates of nomophobia using EEG technology.
- Understanding how the brain responds during situations that trigger nomophobia could inform targeted neurofeedback interventions.
Potential Benefits of EEG Biofeedback in Nomophobia Treatment
Self-Regulation Training:
- EEG biofeedback enables individuals to learn how to regulate their brain activity consciously.
- Nomophobia treatment can involve training individuals to self-regulate their stress responses by modulating specific brainwave patterns associated with anxiety.
Alpha-Theta Training:
- Alpha-theta neurofeedback has been used for anxiety and stress management.
- This biofeedback involves enhancing alpha brainwaves (associated with relaxation) and theta brainwaves (associated with deep relaxation and creativity). It could potentially help individuals achieve a calmer state, reducing nomophobia-related stress.
Cognitive Behavioral Therapy Enhancement:
- EEG biofeedback can complement traditional therapeutic approaches like Cognitive Behavioral Therapy (CBT).
- By incorporating neurofeedback, individuals may gain insights into the physiological aspects of their anxiety and enhance the effectiveness of cognitive strategies to manage nomophobia.
Real-Time Feedback during Exposure:
- Individuals can receive real-time feedback during exposure to situations that trigger nomophobia.
- The biofeedback process can help individuals understand and control their physiological responses, gradually reducing the anxiety associated with being without a mobile phone.
Individualized Treatment Plans:
- EEG biofeedback allows for individualized treatment plans based on the unique brainwave patterns of each person.
- Tailoring interventions to address specific neurological aspects contributing to nomophobia enhances the effectiveness of the treatment.
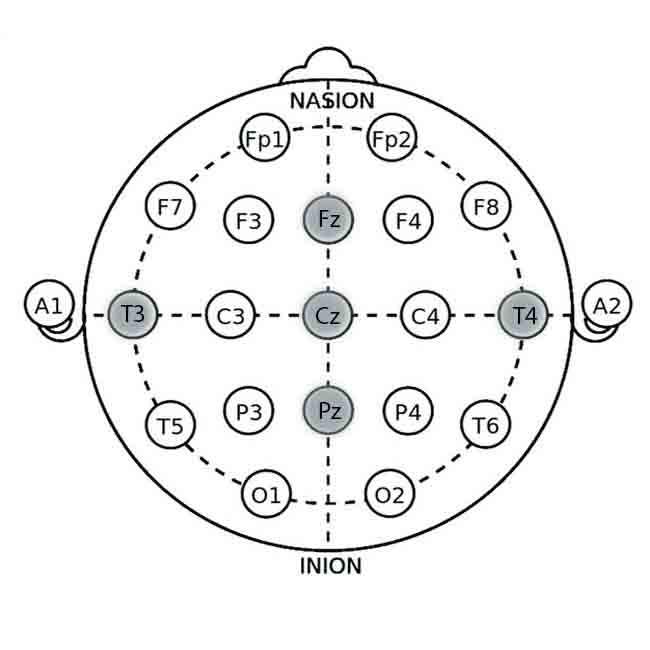
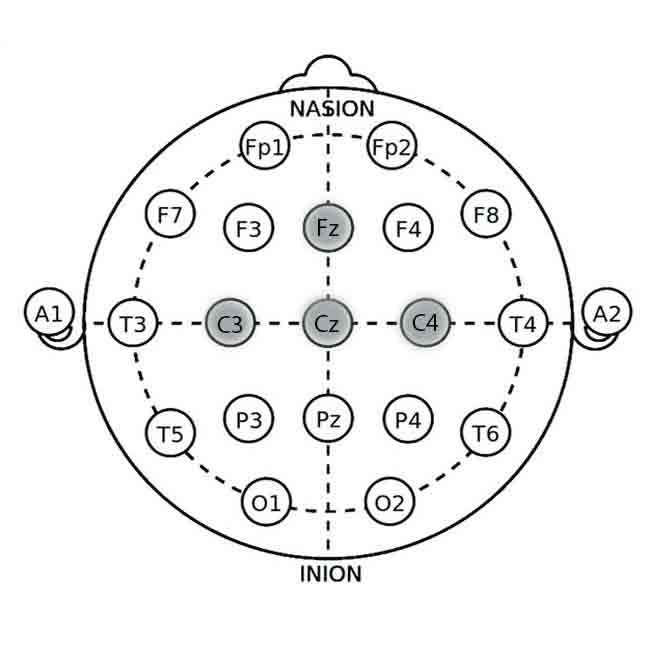
Neurofeedback Protocols for Nomophobia:
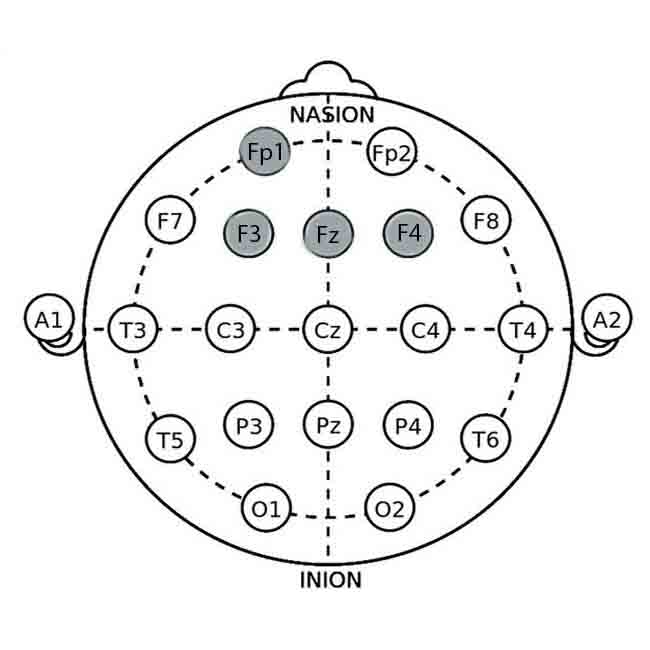
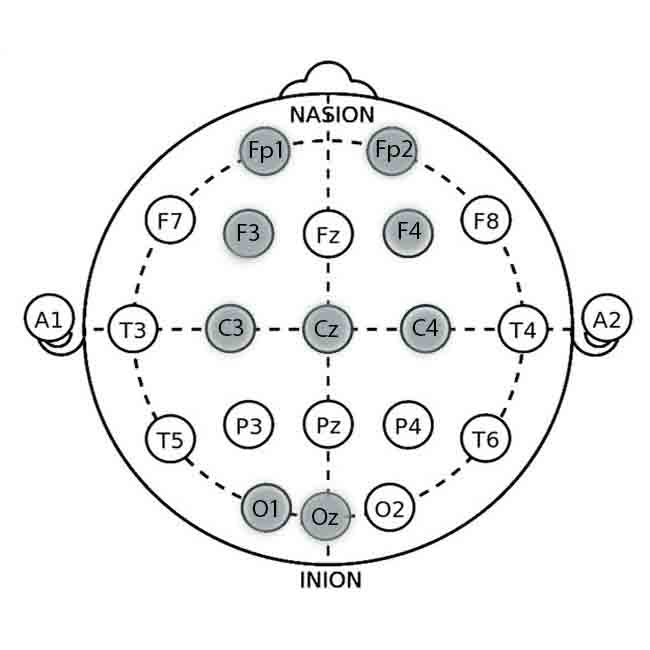
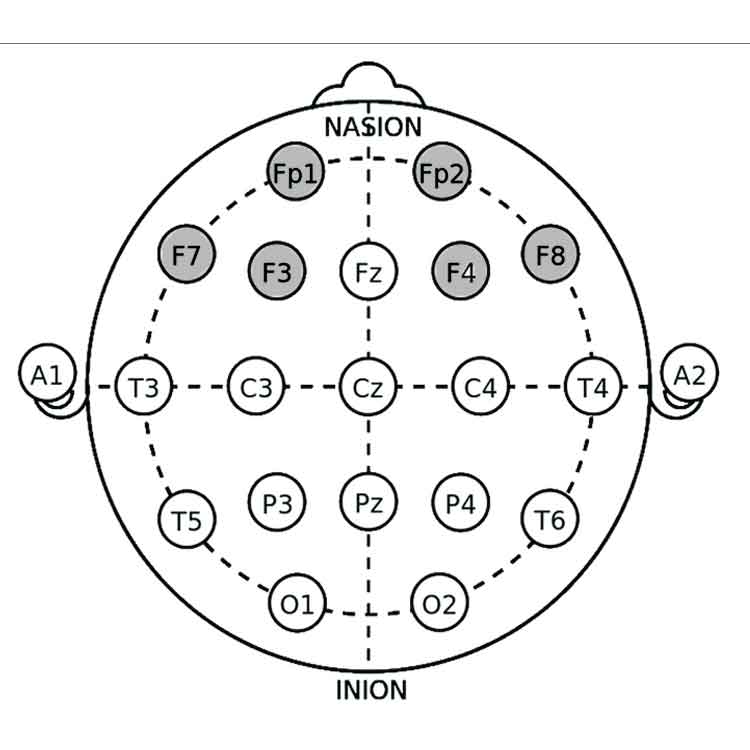
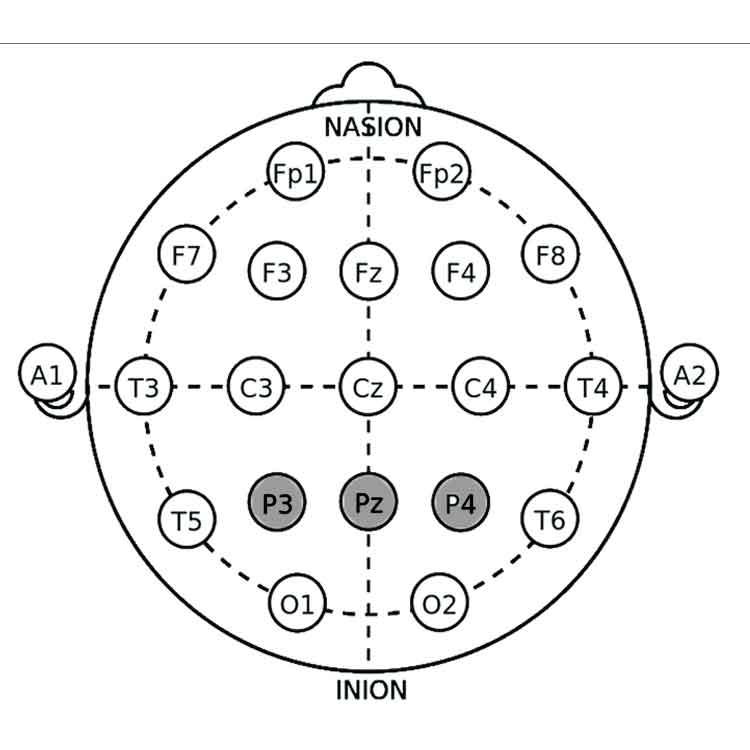
Alpha Training (Occipital Lobe – O1, O2):
- Aim: Increase alpha brainwave activity.
- Rationale: Alpha waves are associated with relaxation and a calm mental state. Training individuals to enhance alpha activity may help reduce overall stress and anxiety related to nomophobia.
Theta Training (Frontal Lobe – F3, F4):
- Aim: Increase theta brainwave activity.
- Rationale: Theta waves are associated with deep relaxation and creativity. By encouraging theta activity, individuals may experience a more tranquil mental state, potentially alleviating the anxiety associated with phone separation.
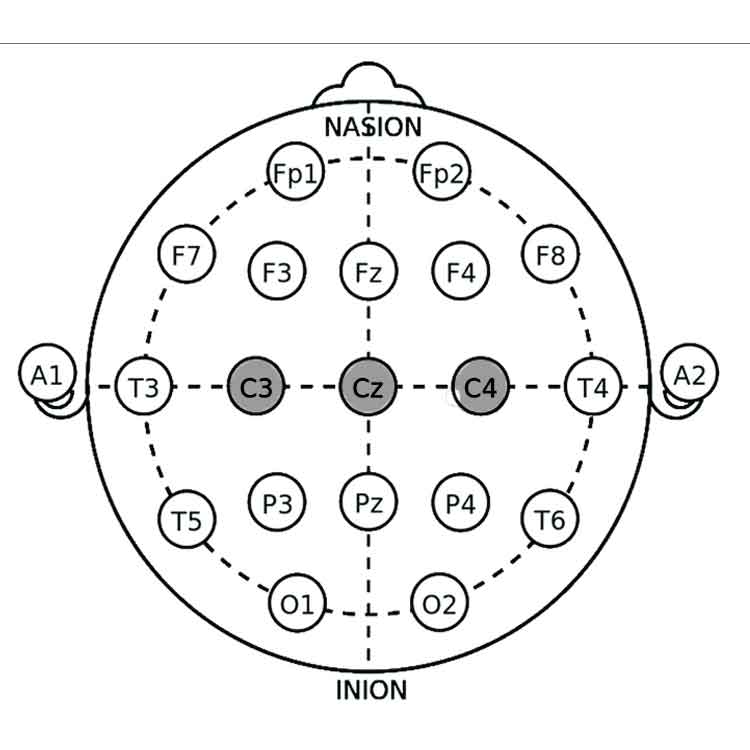
SMR (Sensory-Motor Rhythm) Training (Central Cortex – C3, C4):
- Aim: Increase SMR (12-15 Hz) brainwave activity.
- Rationale: SMR is associated with a calm and focused state. Enhancing SMR activity may contribute to better attention regulation and stress reduction.
Beta Training (Frontal Cortex – F3, F4):
- Aim: Normalize beta brainwave activity.
- Rationale: Abnormal beta activity has been associated with increased anxiety. Normalizing beta levels may help individuals maintain a more balanced and less anxious state.
Application Sites According to the 10-20 System
- O1 and O2: Occipital lobe electrodes for alpha training.
- F3 and F4: Frontal lobe electrodes for theta and beta training.
- C3 and C4: Central cortex electrodes for SMR training.
Challenges and Considerations
1. Research and Validation:
- Rigorous research is needed to establish the effectiveness of EEG biofeedback specifically for nomophobia.
- Validating the neurological correlates of nomophobia and developing targeted interventions require comprehensive studies.
2. Integration with Behavioral Therapy:
- Combining EEG biofeedback with behavioral therapy approaches is crucial for a comprehensive treatment plan.
- Neurofeedback should complement, not replace, traditional therapeutic methods.
3. Ethical Considerations:
- Ethical considerations, such as informed consent and ensuring the well-being of participants, are essential when utilizing neurofeedback for mental health applications. In conclusion, while the direct application of EEG biofeedback for nomophobia remains an evolving area, its potential lies in offering personalized insights into the neural mechanisms underlying stress and anxiety. Furthermore, integrating neurofeedback with existing therapeutic strategies could provide a holistic approach to addressing the complex interplay of psychological and physiological factors associated with nomophobia.
Biofeedback devices that can be used in nomophobia treatment
eSense Biofeedback devices for various biofeedback modalities
Biosignals Multimodal Biofeedback devices that combine all biofeedback modalities in one device provide a multimodal approach to nomophobia management and bring more effective and long-lasting results.