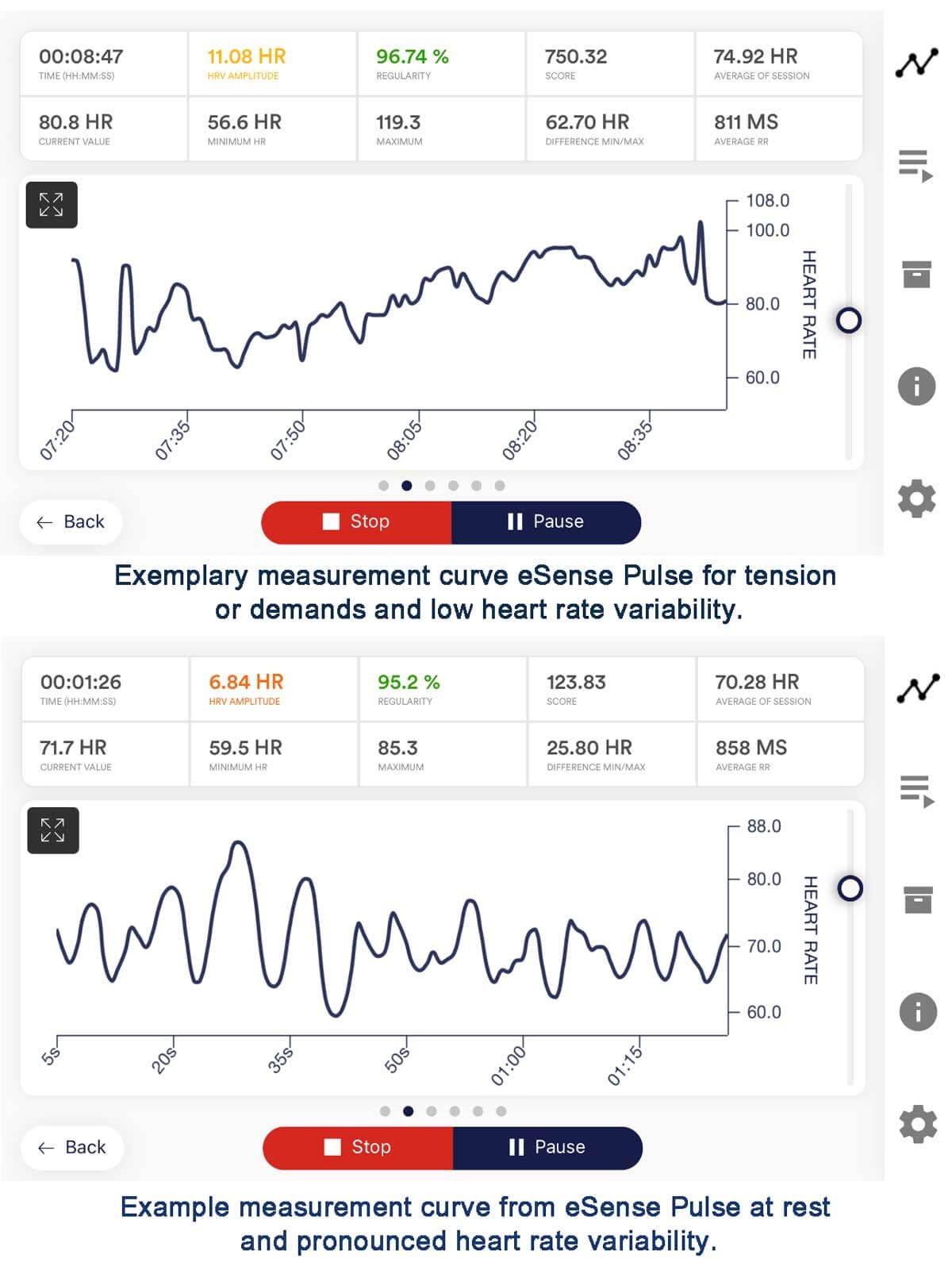
In recent years, integrating HRV training (Heart Rate Variability) with biofeedback guidance has emerged as a promising avenue for enhancing performance across various domains. This approach offers individuals real-time insights and cues to optimize their HRV metrics and overall performance outcomes.
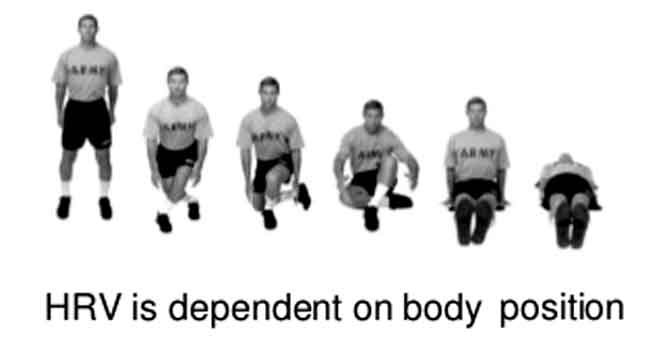
HRV, the variation in the time interval between heartbeats, is a window into the autonomic nervous system’s activity, reflecting the balance between sympathetic and parasympathetic influences. Individuals can use targeted interventions, such as controlled breathing exercises and mindfulness techniques, to modulate their HRV. This modulation can then influence their physiological and psychological states.
Introduction to HRV Training
Heart Rate Variability (HRV) training aims to improve the function of the autonomic nervous system. It works by modulating the variation in the time intervals between heartbeats. This variability indicates the balance between sympathetic (fight-or-flight) and parasympathetic (rest-and-digest) nervous system activity. HRV training typically involves controlled breathing exercises, meditation, and relaxation techniques influencing HRV patterns. By enhancing HRV, individuals can potentially improve their resilience to stress. They may also experience better recovery and optimize performance in various aspects of life.
HRV Indexes
A high HRV index indicates more significant variability between heartbeats. This suggests a well-regulated and flexible autonomic nervous system. Such regulation is associated with better health outcomes and greater resilience to stress. A high HRV index typically falls within the 50-100 milliseconds range. However, specific values can vary based on age and overall health status.
A low HRV index reflects reduced variability between heartbeats, indicating a more rigid and less adaptable autonomic nervous system. Lower HRV often correlates with an increased risk of health issues, including cardiovascular disease, anxiety disorders, and poor emotional regulation. Typically, a low HRV index is below 50 milliseconds. Monitoring HRV indices offers valuable insights into an individual’s physiological and psychological well-being. Understanding these indices can guide interventions aimed at improving overall health and performance.
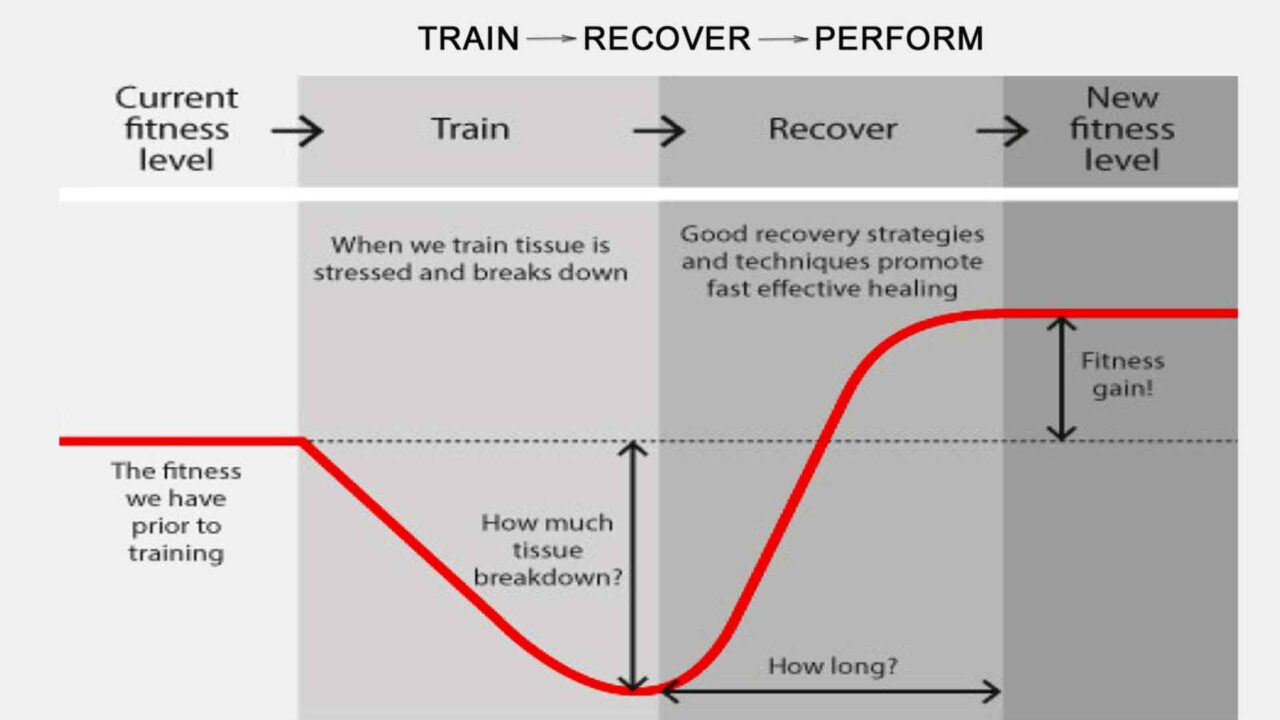
HRV training leverages the body’s ability to adapt and respond to stressors. Consistent practice allows individuals to train their autonomic nervous system to achieve better balance and coherence. This results in increased variability in heart rate patterns. Consistent practice can improve cardiovascular health, emotional regulation, cognitive function, and well-being.
Indications for using HRV training
Experts may recommend HRV training as a complementary therapy for conditions such as hypertension, anxiety disorders, depression, and chronic pain. These conditions often involve dysregulation of the autonomic nervous system.
Stress Management:
HRV training helps individuals cope with stress by promoting relaxation and reducing its physiological effects on the body. Improved HRV links to greater resilience to stressors and better emotional regulation.
Athletic Performance Enhancement:
HRV training can benefit athletes by optimizing performance and enhancing recovery. It also helps manage the demands of training and competition more effectively. Enhanced HRV is linked to better endurance, faster recovery, and overall athletic performance.
Anxiety Reduction:
Experts may recommend HRV training as a complementary therapy for individuals experiencing anxiety disorders. Increasing HRV is associated with reduced anxiety symptoms, improved mood, and greater overall well-being.
Cardiovascular Health:
HRV training can benefit individuals with cardiovascular conditions like hypertension and heart disease. Improving HRV is linked to better cardiovascular function, lower blood pressure, and reduced risk of adverse cardiac events.
Chronic Pain Management:
Individuals suffering from chronic pain conditions may benefit from HRV training as part of a comprehensive pain management strategy. Increasing HRV is associated with reduced pain perception, improved pain tolerance, and enhanced quality of life.
Sleep Quality Improvement:
HRV training has positively impacted sleep quality and duration. Improving HRV can lead to better sleep patterns, fewer disturbances, and enhanced sleep quality.
Emotional Regulation:
HRV training can help individuals better regulate their emotions and respond more effectively to stressful situations. Increasing HRV is associated with improved emotional resilience, excellent emotional stability, and enhanced coping abilities.
Cognitive Function Enhancement:
HRV training improves cognitive function, including enhanced focus, attention, and memory. Increasing HRV may support better cognitive performance and overall mental acuity.
Resilience Building:
HRV training can help build resilience to physical and psychological stressors. Improving HRV promotes greater adaptability, increased resilience, and an enhanced ability to bounce back from challenges.
General Well-being Promotion:
HRV training can promote overall well-being and foster a sense of balance and harmony between mind and body. Increasing HRV is associated with excellent overall health, vitality, and quality of life.
These indications highlight the wide range of benefits HRV training offers. It can improve physical, emotional, and cognitive aspects of health and performance.
The Importance of Biofeedback Guidance for HRV Training
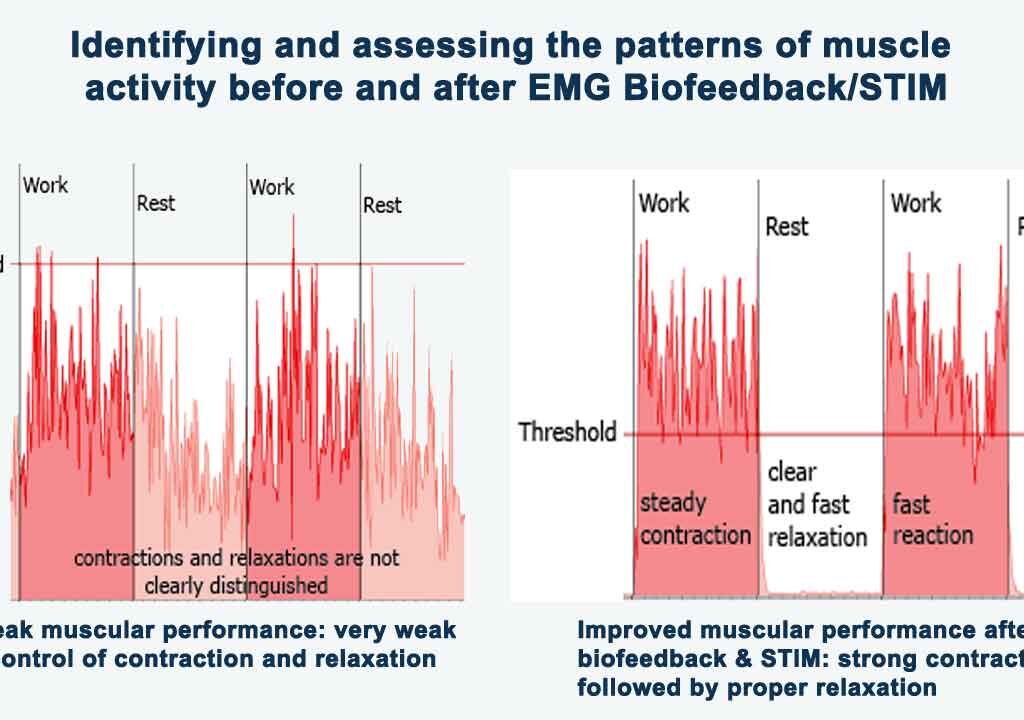
The main distinction between traditional HRV training and HRV training with biofeedback guidance is providing real-time feedback. Both approaches aim to modulate HRV to enhance performance and well-being. However, biofeedback-guided training provides immediate insights into physiological responses, enabling more precise and personalized interventions. The real-time feedback loop enhances the efficacy and efficiency of HRV training. This leads to better outcomes compared to traditional methods alone.
The HRV training biofeedback loop continuously monitors HRV parameters. It interprets physiological responses and adjusts training techniques based on real-time feedback. Sensors detect changes in HRV patterns and present them to the individual through visual or auditory cues. This feedback enables individuals to modulate their HRV responses, improving performance, stress management, and overall well-being.
In summary, while HRV training offers significant potential benefits, incorporating biofeedback guidance can enhance its effectiveness and efficiency. Biofeedback gives individuals real-time information about their physiological responses. This information allows them to adjust their techniques and practices for optimal results. The immediate feedback loop enhances awareness and control over HRV patterns, leading to more targeted and personalized interventions. This approach improves outcomes in stress management, athletic performance, and emotional regulation.
Moreover, biofeedback guidance ensures that individuals adhere to proper techniques and protocols, maximizing the therapeutic benefits of HRV training. Integrating biofeedback into HRV training enhances performance outcomes and deepens the understanding of the mind-body connection. It also enables individuals to modulate HRV patterns more effectively, improving health and performance.
Parameters of HRV Training with Biofeedback Guidance
Heart Rate Variability (HRV) training with biofeedback guidance monitors various parameters and indexes. This approach helps optimize training outcomes and health management. Understanding these parameters is crucial for assessing autonomic nervous system function and guiding interventions to improve HRV patterns.
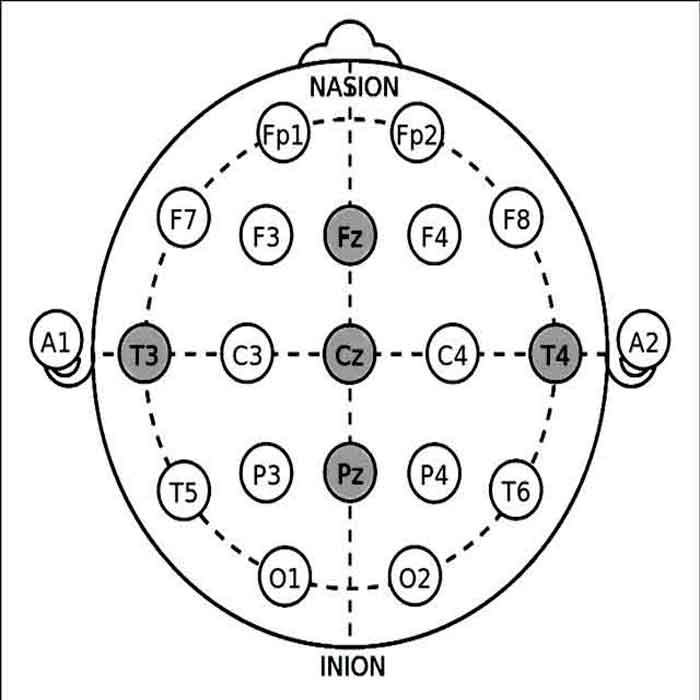
The interval between successive normal heartbeats (between consecutive R waves on an electrocardiogram) tracing is called the NN interval. This interval is also referred to as the normal-to-normal interval. In other words, it measures the time elapsed from one heartbeat to the next normal heartbeat. The NN interval is the basic unit for calculating heart rate variability (HRV). It represents the heart’s rhythm in a stable state.
NN intervals are crucial for analyzing HRV because they reveal variations in the timing between heartbeats. This variation reflects the dynamic interplay of the autonomic nervous system. HRV analysis assesses the balance between sympathetic (fight-or-flight) and parasympathetic (rest-and-digest) nervous system activity. This measurement is based on evaluating differences between successive NN intervals. The balance between sympathetic and parasympathetic systems is vital for regulating various physiological functions and maintaining overall health.
Here are the key parameters and indexes of HRV training with biofeedback guidance.
1. Time Domain Parameters:
SDNN (Standard Deviation of NN intervals): SDNN measures the overall variability of NN intervals, reflecting both sympathetic and parasympathetic influences. A higher SDNN indicates greater HRV and better autonomic function. Typical range: 50-100 ms.
RMSSD (Root Mean Square of Successive Differences): RMSSD reflects parasympathetic activity and short-term HRV. Higher RMSSD values suggest better vagal tone and enhanced relaxation response. The normal range is 20-50 ms.
2. Frequency Domain Parameters:
LF (Low Frequency): LF power represents a mixture of sympathetic and parasympathetic influences, reflecting baroreceptor activity and sympathetic modulation. Increased LF may indicate heightened sympathetic activity or reduced parasympathetic activity. This change could suggest a state of heightened arousal, stress, or a diminished relaxation response. Typical range: 20-40% of total power.
HF (High Frequency): HF power primarily reflects parasympathetic activity and respiratory sinus arrhythmia. Higher HF indicates the prevalence of vagal tone and relaxation response. Elevated HF values suggest a dominance of parasympathetic nervous system activity, particularly the vagus nerve’s influence on the heart. A higher HF indicates a more robust relaxation response and better regulation of physiological functions associated with rest and digestion. Typical range: 40-60% of total power.
3. Nonlinear Parameters:
SD1 (Standard Deviation 1): SD1 represents short-term HRV and reflects beat-to-beat variability influenced by respiratory sinus arrhythmia. Higher SD1 values indicate better parasympathetic modulation, reflecting increased variability in heart rate patterns associated with the respiratory cycle. This mechanism suggests a more decisive influence of the parasympathetic nervous system on heart rate regulation. It promotes relaxation and adaptability to changing physiological demands. The typical range is 5-15 milliseconds.
SD2 (Standard Deviation 2): SD2 reflects long-term HRV and overall variability influenced by sympathetic and parasympathetic activity. Higher SD2 values suggest greater overall HRV, indicating increased variability in heart rate patterns over more extended periods. This broader variability is linked to better adaptability to stressors. It also shows improved cardiovascular health and enhanced overall well-being. The typical range for this variability is 20-50 milliseconds.
4. Others:
Coherence: Coherence measures the degree of synchronization between respiration and heart rate oscillations. Higher coherence values indicate better cardiovascular and respiratory coupling, reflecting more efficient autonomic function.
Unlike other HRV parameters, coherence measures 0 to 1 on a scale. Higher values indicate more robust synchronization between respiratory and heart rate rhythms.
A coherence value closer to 1 indicates high synchronization, reflecting efficient cardiovascular and respiratory coupling. This synchronization is associated with optimal autonomic nervous system function and cardiovascular health. On the other hand, a coherence value closer to 0 suggests weaker synchronization between respiratory and heart rate rhythms. This may indicate autonomic dysfunction or other health issues.
Coherence doesn’t have a specific range like other HRV parameters. Interpreting coherence values involves assessing the synchronization strength between respiratory and heart rate oscillations. This helps understand autonomic nervous system function and cardiovascular health.
Importance of HRV Training with Biofeedback Guidance Parameters in Performance and Health Management
Heart Rate Variability (HRV) training with biofeedback guidance is valuable for optimizing performance and health outcomes. By monitoring and modulating HRV parameters with real-time feedback, individuals can enhance their physiological resilience, emotional regulation, and overall well-being.
Performance Optimization:
HRV training with biofeedback guidance provides athletes, performers, and professionals with a strategic approach to optimizing performance outcomes. Individuals can optimally balance sympathetic and parasympathetic nervous system activity by fine-tuning HRV parameters such as SDNN, RMSSD, LF, HF, SD1, SD2, and coherence. This balance fosters a state of physiological coherence, promoting peak performance, endurance, and recovery. By leveraging biofeedback to adjust real-time training protocols, individuals can adapt to changing demands, manage fatigue, and maximize their competitive edge.
Stress Resilience and Emotional Regulation:
Biofeedback-guided HRV training empowers individuals to manage stress better and regulate their emotions in high-pressure situations. Monitoring HRV parameters, such as LF, HF, SD1, and coherence, helps individuals understand their autonomic nervous system activity and stress response. Targeted interventions, like controlled breathing exercises and mindfulness techniques, allow individuals to modulate HRV patterns. These techniques induce relaxation, reduce anxiety, and enhance emotional resilience. Integrating biofeedback into HRV training boosts self-awareness and control over physiological and psychological responses. This integration fosters a more adaptive stress-coping mechanism.
Cardiovascular Health and Disease Prevention:
HRV training with biofeedback guidance holds promise for promoting cardiovascular health and mitigating the risk of heart disease. Individuals can enhance autonomic nervous system function and cardiovascular regulation by improving HRV parameters such as SDNN, RMSSD, LF, HF, SD1, SD2, and coherence. This optimization reduces the burden on the heart, lowers blood pressure, and improves vascular function. Incorporating biofeedback into HRV training provides personalized feedback on cardiovascular responses. This feedback allows individuals to tailor interventions to meet their specific needs. Over time, this proactive approach to cardiovascular health management may help prevent the onset of heart disease and related complications.
Sleep Quality Enhancement:
HRV training with biofeedback guidance can also improve sleep quality and health. Monitoring HRV parameters like RMSSD, HF, and coherence helps individuals assess autonomic nervous system activity and its effect on sleep patterns. Biofeedback-guided interventions, including relaxation techniques and breathing exercises, help individuals regulate their HRV patterns. These interventions promote relaxation and improve sleep onset and maintenance. Integrating HRV training with biofeedback into a bedtime routine can enhance sleep quality, reduce sleep disturbances, and improve overall sleep health.
Chronic Pain Management:
For individuals dealing with chronic pain conditions, HRV training with biofeedback guidance offers a complementary approach to pain management. Monitoring HRV parameters such as SDNN, LF, and coherence provides valuable insights into autonomic nervous system function. Furthermore, it clarifies the connection between this function and pain perception. Biofeedback-guided interventions, such as deep breathing exercises and mindfulness practices, help modulate HRV patterns. This modulation can reduce pain intensity and improve pain tolerance. Regular HRV training sessions with biofeedback guidance can potentially lead to a decreased reliance on pain medications. Additionally, these sessions may enhance functional abilities and improve overall quality of life.
Cognitive Function Enhancement:
In addition to physical health benefits, HRV training with biofeedback guidance can also support cognitive function and mental well-being. By monitoring HRV parameters such as SDNN, RMSSD, and coherence, individuals can assess their autonomic nervous system activity and its impact on cognitive performance.
Biofeedback-guided HRV training influences cognitive function through several physiological and psychological mechanisms. By providing real-time feedback on HRV parameters, individuals can effectively modulate autonomic nervous system activity. Consequently, this promotes a balanced response characterized by increased parasympathetic activity and decreased sympathetic activity. This physiological balance reduces stress levels and enhances cardiorespiratory efficiency, facilitating optimal oxygenation and blood flow to the brain. Biofeedback-guided HRV training may also synchronize brainwave patterns with HRV parameters, fostering coherence between brain and heart activity.
Combined with consistent modulation of HRV patterns, this coherence promotes neuroplasticity and strengthens neural connections associated with cognitive function. Biofeedback-guided HRV training creates an optimal physiological state for cognitive functioning, improving attention, memory, decision-making, and overall mental well-being.
Biofeedback-guided interventions, such as cognitive-behavioral techniques and attentional focus exercises, can help modulate HRV patterns to enhance cognitive function, including attention, memory, and decision-making. By integrating HRV training with biofeedback guidance into a cognitive training regimen, individuals may experience improved cognitive resilience, enhanced mental clarity, and greater overall cognitive well-being.
Personalized Health Management:
HRV training with biofeedback guidance provides a personalized health management approach. It allows individuals to monitor and optimize physiological responses in real time. Tracking HRV parameters and adjusting training protocols help address specific health concerns like chronic pain, sleep disturbances, and mood disorders. This approach empowers individuals to engage actively in their health and well-being, improving adherence to therapeutic interventions and fostering long-term behavior change. Integrating HRV training with biofeedback into routine health practices can cultivate resilience, enhance performance, and optimize quality of life.
Overall Well-being Promotion:
Ultimately, HRV training with biofeedback guidance promotes overall well-being by empowering individuals to participate actively in their health and performance optimization. Monitoring HRV parameters and adjusting real-time training protocols help individuals cultivate resilience. Additionally, these adjustments reduce stress and enhance physical, emotional, and cognitive well-being. Biofeedback-guided HRV training supports a holistic approach to health management. It addresses the interconnectedness of mind and body and promotes sustainable behavior change. Incorporating HRV training with biofeedback guidance into daily routines enables individuals to unlock their full potential. Consequently, they can thrive in all aspects of life.
In conclusion, HRV training with biofeedback guidance parameters offers a comprehensive approach to performance enhancement and health management. Leveraging real-time feedback to modulate HRV patterns allows individuals to optimize their physiological responses. In addition, this modulation promotes resilience and supports overall health and well-being. As a result, individuals can achieve peak performance while maintaining their overall health. Through personalized interventions and targeted training protocols, HRV training with biofeedback guidance empowers individuals to lead healthier, more fulfilling lives.
How to Regulate and Optimize HRV Parameters and Patterns
Regulating and optimizing HRV parameters and patterns is crucial for enhancing overall health and well-being. By understanding how to modulate these parameters in both high and low cases, individuals can achieve a balanced autonomic nervous system response and promote optimal physiological function. Here are explored strategies for regulating and optimizing HRV parameters, including SDNN, RMSSD, LF, HF, SD1, SD2, and coherence, in various scenarios.
SDNN (Standard Deviation of NN Intervals):
- High SDNN: To regulate high SDNN, individuals can engage in relaxation techniques such as deep breathing exercises, meditation, or progressive muscle relaxation. These practices promote parasympathetic activation, reducing sympathetic dominance and decreasing SDNN.
- Low SDNN: Conversely, to increase low SDNN, individuals can incorporate aerobic exercise into their routine, engage in stress-reducing activities such as yoga or tai chi, or ensure adequate sleep and hydration. These interventions enhance overall HRV and increase SDNN.
RMSSD (Root Mean Square of Successive Differences):
- High RMSSD: Techniques such as paced breathing, mindfulness meditation, or biofeedback-assisted relaxation can help increase RMSSD by enhancing parasympathetic activity and promoting vagal tone.
- Low RMSSD: To address low RMSSD, individuals can focus on stress management strategies, ensure sufficient sleep quality and duration, and adopt a healthy lifestyle that includes regular physical activity and balanced nutrition.
LF (Low Frequency) and HF (High Frequency):
- High LF: To regulate high LF, individuals can engage in relaxation techniques such as diaphragmatic breathing, progressive muscle relaxation, or guided imagery. These practices help reduce sympathetic activity and rebalance the autonomic nervous system.
- Low LF: Conversely, to increase low LF, individuals can engage in moderate-intensity aerobic exercise, practice stress-inducing activities such as cold exposure or intermittent hypoxic training, or consume caffeine in moderation.
- High HF: Techniques such as paced breathing, mindfulness meditation, or biofeedback-assisted relaxation can help increase HF by enhancing parasympathetic activity and promoting vagal tone.
- Low HF: To address low HF, individuals can focus on stress management strategies, ensure sufficient sleep quality and duration, and adopt a healthy lifestyle that includes regular physical activity and balanced nutrition.
SD1 (Standard Deviation 1) and SD2 (Standard Deviation 2):
- High SD1 and SD2: Techniques such as paced breathing, coherence training, or mindfulness meditation can help increase both SD1 and SD2 by promoting parasympathetic activation and enhancing heart rate variability.
- Low SD1 and SD2: To address low SD1 and SD2, individuals can use relaxation techniques, stress management strategies, and regular physical activity to enhance overall HRV and improve autonomic function.
Coherence:
- High Coherence: Techniques such as coherent breathing, HRV biofeedback training, or mindfulness-based practices can help increase coherence by promoting synchronization between respiratory and heart rate oscillations.
- Low Coherence: To address low coherence, individuals can focus on improving relaxation skills, practicing slow, deep breathing exercises, and incorporating coherence training into their daily routines.
Implementing strategies tailored to specific HRV parameters and patterns helps individuals regulate their autonomic nervous system function. This regulation effectively optimizes their overall health, well-being, and performance. As a result, people see enhancements in all these areas.
Techniques for Managing HRV Parameters with Biofeedback-Guided Training
Breathing Techniques
Diaphragmatic Breathing:
Diaphragmatic breathing (see video explanation), also known as abdominal or deep breathing, involves engaging the diaphragm to take slow, deep breaths.
To practice diaphragmatic breathing, individuals should first sit or lie comfortably. Next, they should place one hand on their abdomen and inhale deeply through their nose, allowing their belly to rise. Afterward, they should exhale slowly through their mouth while contracting their abdominal muscles.
Diaphragmatic breathing involves slow, deep inhalations and exhalations that engage the diaphragm. This practice enhances HRV by promoting relaxation and activating the parasympathetic nervous system. As individuals continue diaphragmatic breathing, they stimulate the vagus nerve. This stimulation leads to increased vagal tone and more significant variability in heart rate. Consequently, individuals experience higher HRV, which indicates a more adaptive autonomic response and improved cardiovascular health.
Paced Breathing:
Another effective technique is paced breathing (see video explanation), which entrains respiratory and heart rate rhythms to a specific frequency or pattern. Paced breathing involves synchronizing the breathing patterns with a particular rhythm or pace, typically guided by visual or auditory cues. Common-paced breathing techniques include coherent breathing (breathing at a rate of 6 breaths per minute) and resonance frequency breathing (see video explanation) (aligning breathing with individual resonance frequency). Paced breathing enhances HRV by promoting rhythmic heart rate patterns and coherence between respiratory and heart rate oscillations. These breathing techniques foster relaxation and stress reduction and optimize autonomic balance, ultimately improving HRV parameters and overall well-being.
Changes in HRV parameters during breathing techniques reflect the modulation of autonomic nervous system activity. Specifically, these changes include an increase in parasympathetic activity and a decrease in sympathetic activity. Additionally, breathing techniques enhance respiratory sinus arrhythmia and promote physiological coherence. As a result, parameters such as SDNN, RMSSD, HF, SD1, SD2, and Coherence increase. In contrast, LF decreases.
By practicing breathing techniques regularly, individuals can optimize HRV parameters, promote relaxation, and support overall health and well-being.
Exercise:
- Aerobic Exercise: Aerobic exercise, such as walking, running, cycling, swimming, or dancing, involves continuous, rhythmic movements that increase heart rate and oxygen consumption. Regular aerobic exercise improves cardiovascular fitness, enhances respiratory efficiency, and increases HRV. To optimize HRV benefits, individuals should engage in moderate-intensity aerobic exercise for at least 30 minutes most days a week.
- Strength Training: Strength training exercises, such as weightlifting, resistance band workouts, or bodyweight exercises, involve repetitive muscle contractions against resistance. While strength training primarily targets muscular strength and endurance, it can also indirectly improve HRV by promoting cardiovascular health and metabolic efficiency.
Moderate-intensity aerobic exercise increases HRV, particularly HF power. Regular physical activity can help rebalance autonomic nervous system activity by enhancing parasympathetic tone and reducing sympathetic dominance.
Mindfulness Practices:
- Meditation: Meditation involves focusing on a specific object, thought, or sensation to cultivate present-moment awareness and mental clarity. Mindfulness meditation practices, including focused attention meditation, loving-kindness meditation, and body scan meditation, promote relaxation, reduce stress, and increase HRV by enhancing parasympathetic activation and emotional regulation.
- Mindful Breathing: Mindful breathing, or breath awareness, involves paying attention to the sensations of breathing without judgment. By consciously observing each inhalation and exhalation, individuals can anchor their awareness in the present moment, reduce rumination, and enhance HRV by promoting relaxation and stress reduction.
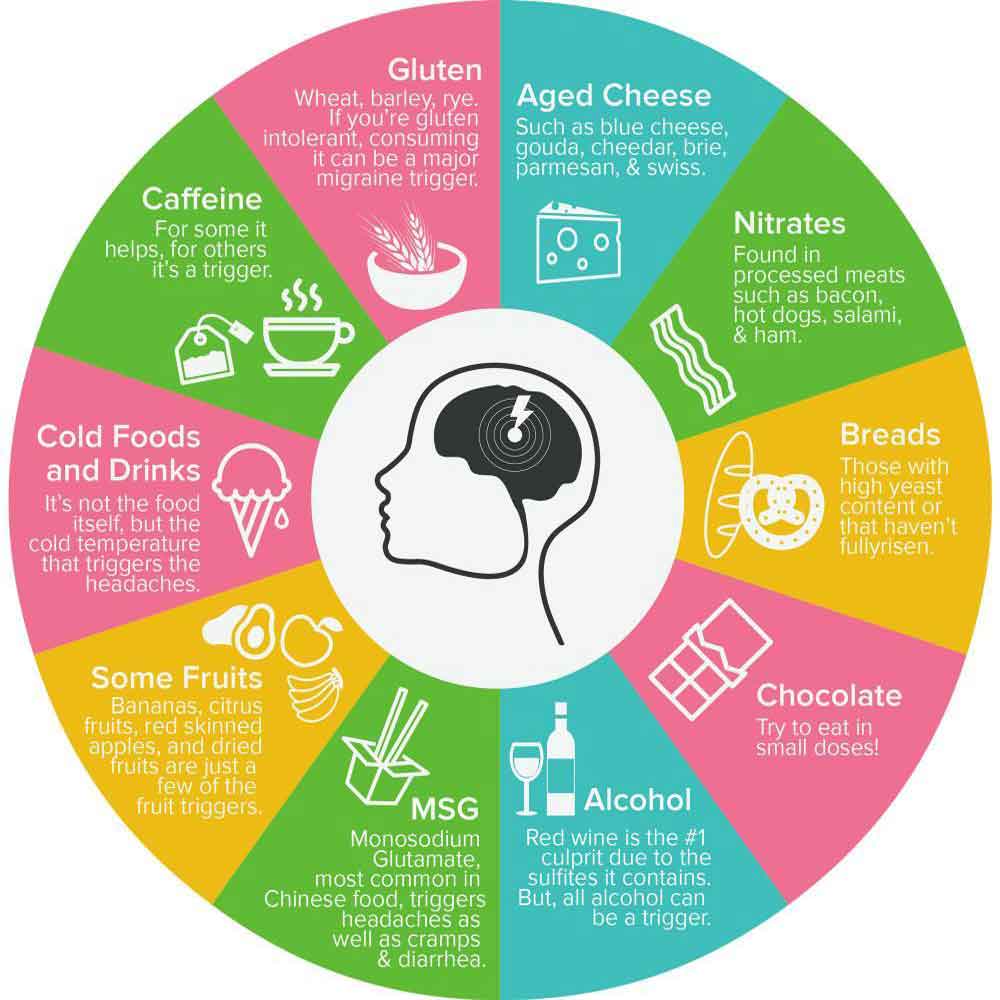
Diet:
- Balanced Nutrition: A balanced diet rich in fruits, vegetables, whole grains, lean proteins, and healthy fats supports overall health and can positively influence HRV. Certain nutrients, such as omega-3 fatty acids, magnesium, and antioxidants, have been associated with improved cardiovascular function and increased HRV. Conversely, excessive processed foods, sugary beverages, and high-fat meals may negatively impact HRV.
Sleep Hygiene:
- Consistent Sleep Schedule: Maintaining a consistent sleep schedule by going to bed and waking up at the same time daily helps regulate circadian rhythms and supports healthy sleep patterns. Adults should aim for 7-9 hours of sleep daily to optimize HRV and overall well-being.
- Sleep Environment: Creating a comfortable, relaxed, dark, and quiet environment promotes restful sleep and enhances HRV. To improve sleep quality, individuals should minimize exposure to electronic devices before bedtime, avoid caffeine and alcohol close to bedtime, and establish relaxing bedtime rituals.
Stress and Anxiety Management:
- Stress Reduction Techniques: Stress reduction techniques, such as progressive muscle relaxation, guided imagery, or journaling, help alleviate tension and promote relaxation. By practicing stress management strategies regularly, individuals can reduce chronic stress levels, improve emotional resilience, and enhance HRV.
- Anxiety Management Strategies: Anxiety management techniques, such as cognitive-behavioral therapy (CBT), deep breathing exercises, or mindfulness-based stress reduction (MBSR), empower individuals to cope effectively with anxious thoughts and emotions. These strategies promote emotional regulation, reduce physiological arousal, and increase HRV.
Implementing these techniques into biofeedback-guided HRV training can help individuals optimize HRV parameters, enhance autonomic nervous system function, and promote overall health and well-being.
Understanding the Difference Between HRV Training Devices and Biofeedback-Guided HRV Training Devices
Heart Rate Variability (HRV) training has gained popularity as a method for improving physiological resilience and overall well-being. While both HRV training devices and biofeedback-guided HRV training devices aim to enhance HRV patterns, there are fundamental differences between the two approaches.
HRV Training Devices:
HRV training devices typically measure and analyze HRV patterns without real-time feedback or intervention. These devices collect heart rate data over time and provide metrics such as SDNN, RMSSD, LF, HF, SD1, SD2, and coherence, which reflect autonomic nervous system activity and cardiovascular function. HRV training devices may include wearable heart rate monitors, smartphone apps, or standalone HRV measurement tools.
Users of HRV training devices often review their HRV data retrospectively and adjust lifestyle factors, such as exercise, sleep, stress management, and nutrition, to optimize HRV patterns. While HRV training devices offer valuable insights into autonomic function, they lack real-time feedback mechanisms for guiding interventions and behavior modifications.
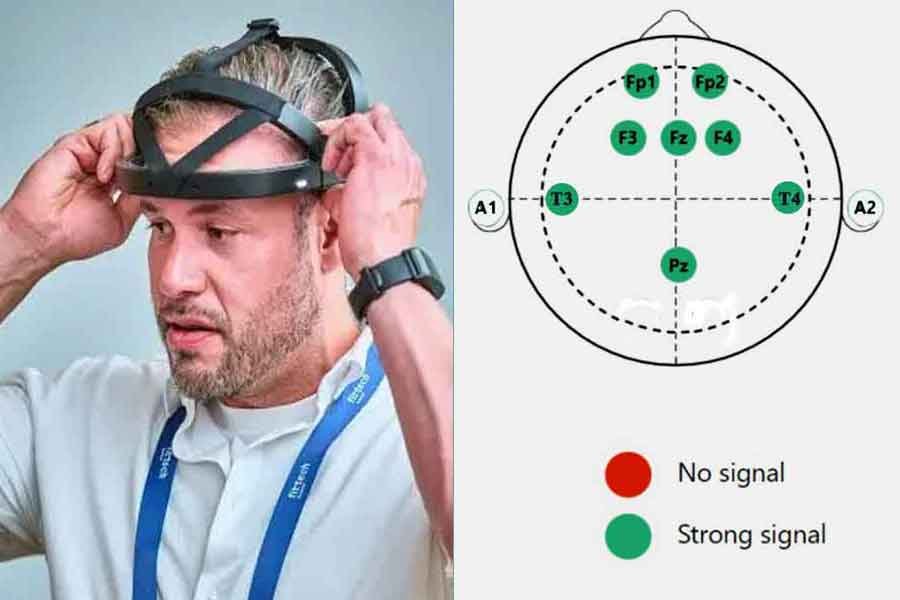
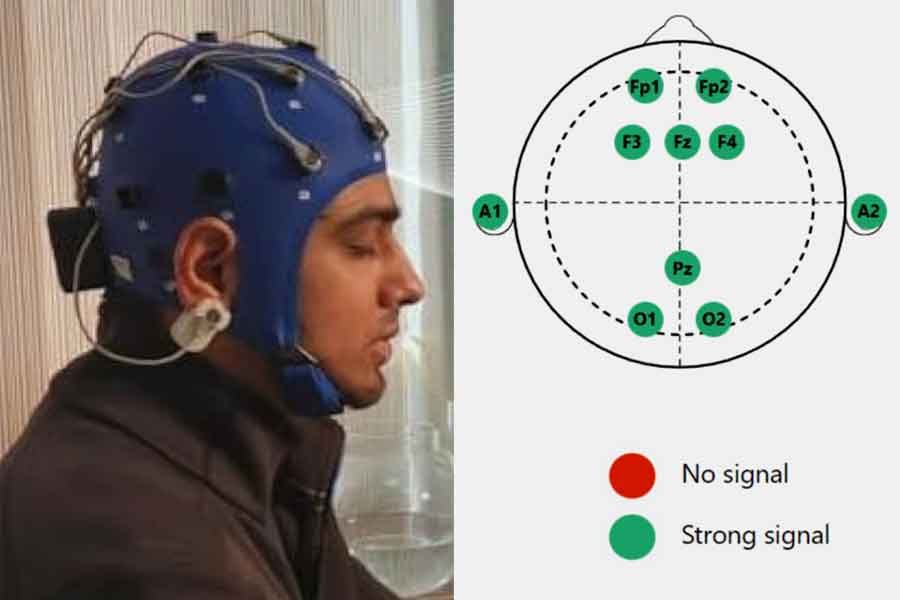
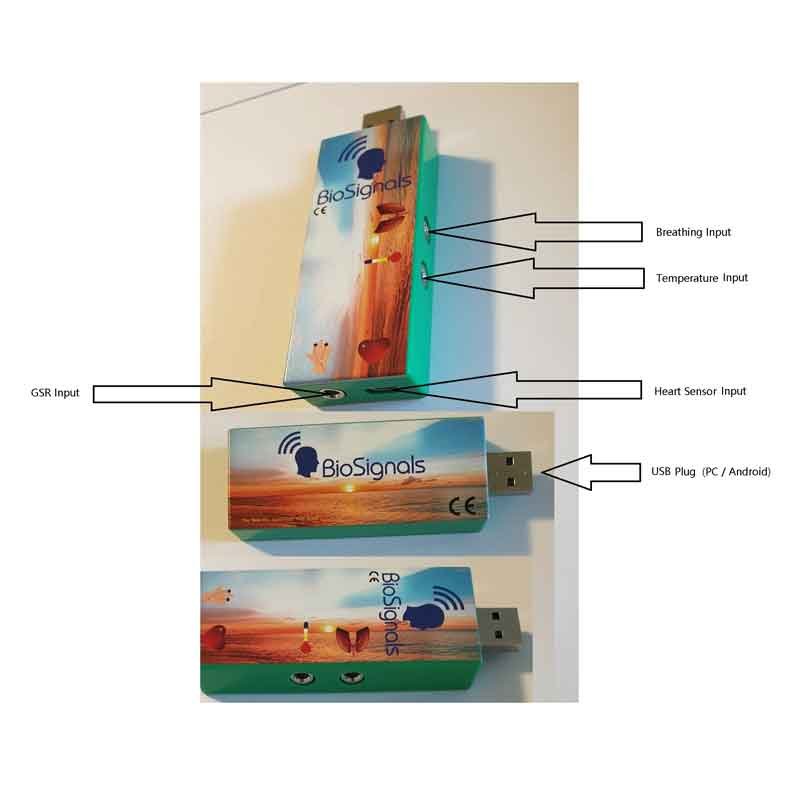
Biofeedback-Guided HRV Training Devices:
In contrast, biofeedback-guided HRV training devices combine HRV measurement with real-time feedback and intervention capabilities. These devices monitor HRV parameters and provide immediate feedback to users, allowing them to modulate their physiological responses in real-time. Biofeedback-guided HRV training devices typically employ visual, auditory, or tactile cues to indicate changes in HRV patterns and guide users in achieving desired physiological states. Users can actively influence their HRV patterns and promote physiological coherence by engaging in paced breathing, relaxation exercises, or mindfulness practices.
Biofeedback-guided HRV training devices may include wearable sensors, smartphone apps, or standalone biofeedback devices equipped with HRV monitoring capabilities. Integrating real-time feedback into HRV training facilitates personalized interventions, enhances self-regulation skills, and promotes efficient physiological adaptation.
Key Differences:
The primary difference between HRV training devices and biofeedback-guided HRV training devices lies in providing real-time feedback and intervention capabilities. While HRV training devices focus on data collection and retrospective analysis, biofeedback-guided HRV training devices enable users to engage in HRV modulation through immediate feedback and intervention actively. Biofeedback-guided HRV training devices offer a dynamic and interactive approach to HRV training, empowering users to optimize autonomic function and enhance overall well-being in real time.
In summary, while HRV training devices and biofeedback-guided HRV training devices aim to improve HRV patterns, the latter approach distinguishes itself by incorporating real-time feedback. By providing immediate feedback and intervention capabilities, biofeedback-guided HRV training devices offer a more interactive and personalized approach to HRV modulation, facilitating efficient self-regulation and physiological adaptation.
Selecting the Right Biofeedback-Guided HRV Training Device
Choosing the appropriate biofeedback-guided HRV training device is essential for optimizing your HRV training experience and achieving your health and wellness goals. With various available options, consider several factors to ensure you select the device that best suits your needs and preferences.
Define Your Goals:
Before selecting a biofeedback-guided HRV training device, you must clarify your specific goals and objectives. Determine whether you aim to reduce stress, improve resilience, enhance athletic performance, manage chronic health conditions, or optimize overall well-being. Understanding your goals will help you narrow down the features and functionalities required in a training device.
Consider Device Features:
Please evaluate the features and capabilities of each biofeedback-guided HRV training device to ensure they align with your needs. Key features to consider include:
Real-time Feedback: Look for devices that offer immediate feedback on HRV parameters and guide you through real-time interventions.
User Interface: Assess the usability and intuitiveness of the device’s interface, including the display, controls, and navigation.
Customization Options: Choose a device for personalized settings and training programs tailored to your preferences and goals.
Compatibility: Ensure compatibility with your existing devices and platforms, such as smartphones, tablets, or computers, for seamless integration and data sharing.
Portability: Consider the device’s portability and convenience in various settings, including home, office, or travel.
Review Training Programs:
Explore the training programs and protocols each biofeedback-guided HRV training device offers to determine their suitability for your goals and preferences. Look for devices that provide a variety of guided interventions, such as paced breathing exercises, relaxation techniques, mindfulness practices, or coherence training. Consider whether the device offers customizable training programs to accommodate your needs and progression.
Assess Data Insights:
Examine the data insights and analytics each biofeedback-guided HRV training device provides to ensure they offer valuable information for monitoring progress and optimizing training outcomes. Look for devices that provide comprehensive metrics on HRV parameters, trends, patterns, and actionable recommendations for adjustments and improvements. Consider whether the device offers data visualization tools, reporting capabilities, or integration with third-party platforms for enhanced data analysis and interpretation.
Read Reviews and Recommendations:
Before making a purchase decision, research and read reviews from other users, healthcare professionals, or experts in the field. Pay attention to feedback regarding device reliability, accuracy, effectiveness, ease of use, and customer support. Seek recommendations from trusted sources or online communities to gain insights into the real-world experiences of users using the device for HRV training.
Budget Considerations:
Finally, consider your budget constraints and investment preferences when selecting a biofeedback-guided HRV training device. Compare the cost of each device relative to its features, capabilities, and long-term value for achieving your goals. Remember that while some devices may have a higher upfront cost, they may offer greater functionality, durability, and support for long-term use.
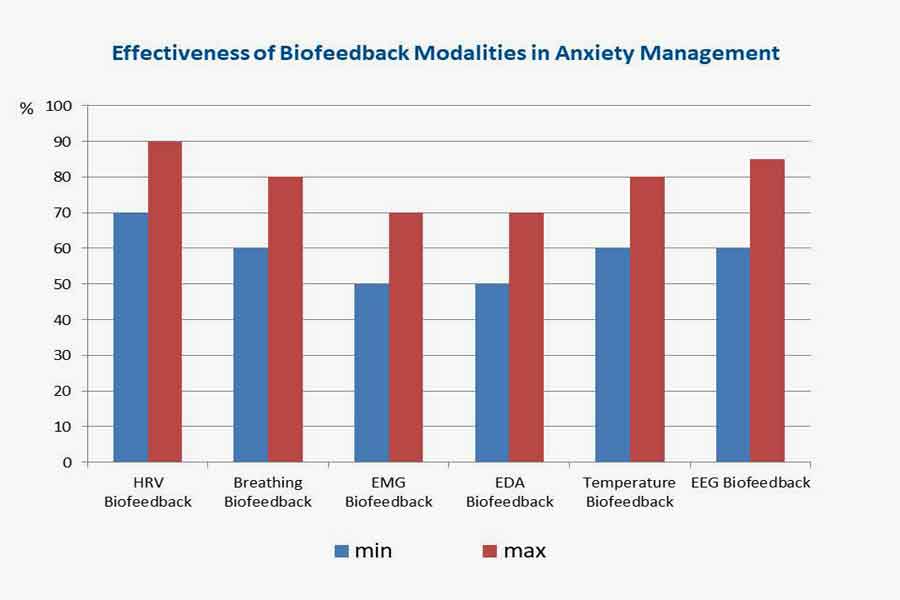
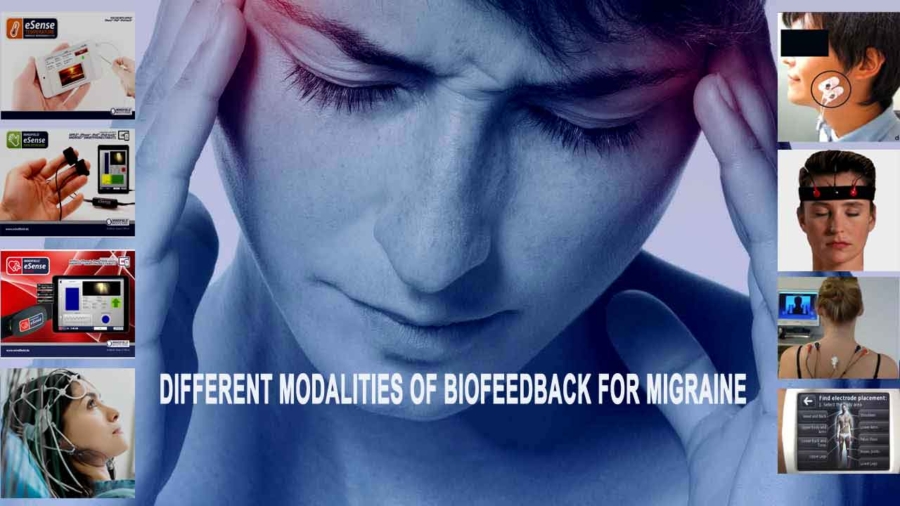
Enhancing Effectiveness with Combined Biofeedback Modalities:
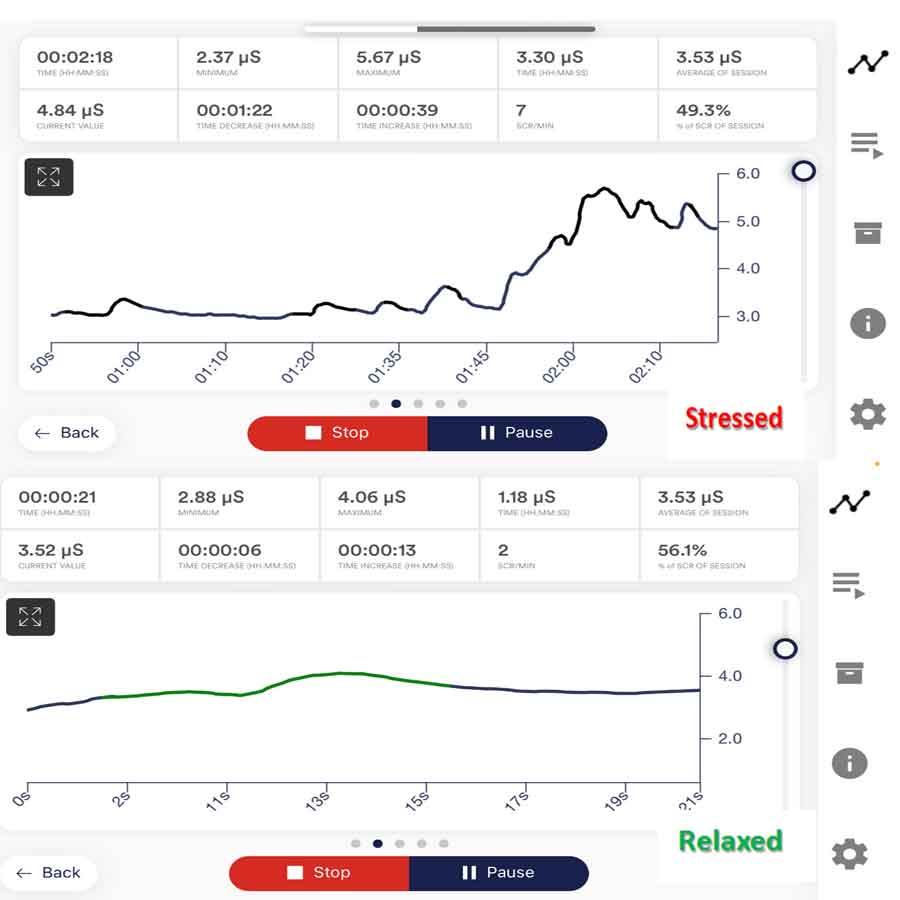
Combining biofeedback-guided HRV training with other biofeedback modalities, such as breathing biofeedback and galvanic skin response (GSR) biofeedback, can enhance the effectiveness of HRV training and optimize physiological regulation. Breathing biofeedback focuses on improving respiratory patterns and promoting relaxation through paced and diaphragmatic breathing techniques.
By incorporating breathing biofeedback into HRV training, individuals can enhance respiratory sinus arrhythmia, synchronize respiratory and heart rate rhythms, and achieve greater coherence between autonomic functions.
Similarly, GSR biofeedback measures changes in skin conductance, reflecting sympathetic nervous system arousal and emotional regulation. Integrating GSR biofeedback with HRV training allows individuals to monitor stress levels, enhance emotional awareness, and develop strategies for stress management. Combining multiple biofeedback modalities, individuals can access a comprehensive toolkit for self-regulation, optimizing HRV patterns, and promoting holistic well-being. This synergistic approach leverages the complementary benefits of different biofeedback modalities, resulting in more profound physiological and psychological effects.
Performing Biofeedback-Guided HRV Training Correctly
Performing biofeedback-guided HRV training according to recommendations is essential for maximizing its benefits and avoiding potential adverse or side effects. Here are guidelines and recommendations for conducting it effectively, including considerations for monitoring HRV parameters, scheduling training sessions, setting intensity levels, and implementing other best practices.
Attend to Proper Technique:
Ensure you use proper technique during biofeedback-guided HRV training sessions, especially when performing breathing exercises or relaxation techniques. Follow the instructions the device or app provides accurately and maintain a relaxed, comfortable posture throughout the session. Pay attention to your breathing pattern, heart rate variability, and any visual or auditory cues the device provides to guide your interventions.
Monitor HRV Parameters:
Monitor HRV parameters during training sessions regularly to track your progress and ensure you achieve the desired physiological responses. Focus on metrics such as SDNN, RMSSD, LF, HF, SD1, SD2, and coherence to assess changes in autonomic nervous system activity and cardiovascular function. Aim to maintain or increase HRV parameters within optimal ranges while avoiding excessive fluctuations that may indicate overexertion or stress.
Set Realistic Goals:
Establish realistic goals for your biofeedback-guided HRV training based on your needs, preferences, and health status. Start with achievable objectives, such as reducing stress levels, improving relaxation skills, or enhancing overall well-being, and gradually progress as you build proficiency and confidence in your training. Avoid setting overly ambitious goals that may lead to frustration or burnout.
Schedule Training Sessions:
Consistently schedule biofeedback-guided HRV training sessions into your daily or weekly routine to ensure regular practice and sustained progress. Allocate dedicated time for training sessions, ideally at the same time each day or week, to establish a consistent habit. Choose a quiet, comfortable environment free from distractions to optimize your focus and relaxation during training.
Adjust Intensity Levels:
Pay attention to your body’s responses and adjust the intensity levels of your training sessions accordingly. Start with gentle interventions and gradually increase the intensity as you become more comfortable and proficient. Monitor HRV parameters throughout the session and establish stop lines or thresholds to prevent overexertion or adverse reactions. Aim to balance challenging yourself and staying within your physiological limits.
Listen to Your Body:
Listen to your body’s signals and respect its limitations during biofeedback-guided HRV training. If you experience discomfort, fatigue, or negative symptoms such as dizziness or shortness of breath, pause the training session and take a break. Pay attention to any warning signs of overtraining or excessive stress and adjust your training intensity or duration accordingly.
Seek Professional Guidance:
Consider seeking guidance from a qualified healthcare professional or certified biofeedback therapist to ensure safe and effective implementation of biofeedback-guided HRV training. Consult with experts who can provide personalized recommendations, monitor your progress, and address any concerns or challenges you encounter during training. Professional guidance can enhance the effectiveness of your training and help you achieve optimal results while minimizing risks.
Maintain Balance and Consistency:
Maintain a balance between biofeedback-guided HRV training and other aspects of your lifestyle, including exercise, nutrition, sleep, and stress management. Avoid overemphasizing HRV training at the expense of other important health behaviors. Strive for consistency in your training regimen, but also allow for flexibility and adaptability to accommodate changes in your schedule or individual needs.
Following these guidelines and recommendations, you can perform biofeedback-guided HRV training correctly, maximize its benefits, and minimize potential adverse or side effects. Stay attentive to proper technique, monitor HRV parameters, set realistic goals, schedule training sessions consistently, adjust intensity levels appropriately, listen to your body, seek professional guidance, and maintain balance and consistency in your training approach. With diligent practice and mindful attention, biofeedback-guided HRV training can be a powerful tool for enhancing health, resilience, and well-being.
Conclusion
In conclusion, biofeedback-guided HRV training enhances physiological resilience, promotes stress management, and optimizes overall well-being. By leveraging real-time feedback mechanisms and interventions, individuals can actively modulate their autonomic nervous system activity, improve HRV patterns, and achieve greater physiological coherence.
Biofeedback-guided HRV training offers a dynamic and interactive method for self-regulation. It empowers individuals to cultivate skills for managing stress, enhancing relaxation, and promoting adaptive responses to environmental challenges. By incorporating techniques such as paced breathing, relaxation exercises, mindfulness practices, and coherence training, individuals can optimize HRV parameters, support cardiovascular health, and foster emotional well-being.
When performing biofeedback-guided HRV training, it is crucial to focus on proper technique. Additionally, individuals should monitor HRV parameters closely. Setting realistic goals is also essential. Consistently scheduling training sessions helps maintain progress. Adjusting intensity levels appropriately is necessary to match individual needs.
Furthermore, listening to the body’s signals ensures that the training remains effective. Seeking professional guidance as needed can provide additional support. Lastly, maintaining balance and consistency in the training approach is essential.
By following these guidelines and recommendations, individuals can fully harness the benefits of biofeedback-guided HRV training. As a result, they will be better equipped to achieve their health and wellness goals.
HRV Training Biofeedback Device
List of References
- Lehrer, P. M., & Gevirtz, R. (2014). Heart rate variability biofeedback: How and why does it work? Frontiers in Psychology, 5, 756.
- McCraty, R., Atkinson, M., et al. (2009). The coherent heart: Heart–brain interactions, psychophysiological coherence, and the emergence of system-wide order. Integral Review, 5(2), 10-115.
- Shaffer, F., & Ginsberg, J. P. (2017). An overview of heart rate variability metrics and norms. Frontiers in public health, 5, 258.
- Laborde, S., Mosley, E., et al. (2017). Heart rate variability and cardiac vagal tone in psychophysiological research–recommendations for experiment planning, data analysis, and data reporting. Frontiers in Psychology, 8, 213.
- McCraty, R., & Shaffer, F. (2015). Heart rate variability: new perspectives on physiological mechanisms, assessment of self-regulatory capacity, and health risk. Global advances in health and medicine, 4(1), 46-61.
- Laborde, S., & Allen, M. S. (2016). The role of cardiac vagal activity in the relationship between exercise and executive functioning. Brain and Cognition, 110, 102-106.
- Gevirtz, R. (2013). The promise of heart rate variability biofeedback: evidence-based applications. Biofeedback, 41(3), 110-120.
- Zaccaro, A., Piarulli, A., et al. (2018). How breath-control can change your life: A systematic review on psycho-physiological correlates of slow breathing. Frontiers in human neuroscience, 12, 353.
- van der Zwan, J. E., de Vente, W., et al. (2015). Physical activity, mindfulness meditation, or heart rate variability biofeedback for stress reduction: A randomized controlled trial. Applied Psychophysiology and Biofeedback, 40(4), 257-268.
- Grossman, P., & Taylor, E. W. (2007). Toward understanding respiratory sinus arrhythmia: Relations to cardiac vagal tone, evolution, and biobehavioral functions. Biological Psychology, 74(2), 263-285.