Autism Spectrum Disorder (ASD) is a complex neurodevelopmental condition characterized by challenges in social interaction, communication, and repetitive behaviors. As the prevalence of autism continues to rise, with recent estimates suggesting that 1 in 54 children in the United States is diagnosed with ASD, there is an increasing need for effective management strategies. Traditional treatment approaches, including behavioral therapies, speech therapy, and pharmacological interventions, have been instrumental in helping individuals with autism improve their quality of life. However, neurofeedback, a cutting-edge biofeedback technique, has emerged as a promising complementary therapy in autism management. By harnessing the brain’s neuroplasticity, neurofeedback aims to train individuals to regulate their brainwave patterns, potentially leading to improved behavior, communication, and overall cognitive function. This article explores the role of neurofeedback autism management, delving into its mechanisms, benefits, and future potential.
Table of Contents
ToggleOverview of Autism Spectrum Disorder (ASD)
Autism Spectrum Disorder (ASD) is a complex neurodevelopmental condition that affects individuals in varying degrees of severity. Characterized by difficulties in social communication and interaction, as well as the presence of restricted and repetitive behaviors, ASD manifests differently in each individual, making it a spectrum disorder. The understanding of ASD has evolved significantly over the years, leading to better diagnostic criteria and more effective management strategies.
Definition and Characteristics of ASD
ASD encompasses a range of conditions previously classified separately, including autistic disorder, Asperger’s syndrome, and pervasive developmental disorder not otherwise specified (PDD-NOS). The core characteristics of ASD include:
• Social Communication Challenges: Individuals with ASD often struggle with verbal and non-verbal communication. They may have difficulty understanding social cues, maintaining eye contact, and engaging in back-and-forth conversations.
• Restricted and Repetitive Behaviors: These may include repetitive movements, insistence on sameness, and highly focused interests. Some individuals may exhibit extreme distress at small changes in routines or surroundings.
• Sensory Sensitivities: Many individuals with ASD experience sensory processing issues, leading to hyper- or hypo-sensitivity to sounds, lights, textures, and other sensory stimuli.
Prevalence and Diagnosis
The prevalence of ASD has been steadily increasing, with current estimates indicating that approximately 1 in 54 children in the United States is diagnosed with the disorder. This rise in prevalence can be attributed to increased awareness, better diagnostic practices, and changes in diagnostic criteria.
Diagnosis of ASD typically occurs in early childhood, although some individuals may not be diagnosed until later in life. The diagnostic process involves comprehensive evaluations by healthcare professionals, including developmental screenings, behavioral assessments, and standardized diagnostic tools such as the Autism Diagnostic Observation Schedule (ADOS) and the Autism Diagnostic Interview-Revised (ADI-R).
Autism Spectrum Screening Questionnaire
The ASSQ is a 27-question assessment completed by parents or teachers of children or adolescents (6 to 17 years of age). It is designed to be an initial screen for Autism Spectrum Disorder (ASD), especially in those with high or normal IQ, or those with only mild intellectual disability.
Results consist of a total score between 0 and 54, where higher scores indicate that many characteristics of ASD were reported.
A score of 13 and above indicates ASD is probable, with a true positive rate of 90% and a false positive rate of 22% (Ehlers, Gillberg, Wing, 1999). This test is not diagnostic.
Challenges Faced by Individuals with ASD
Individuals with ASD face a variety of challenges that can impact their daily lives and overall well-being. These challenges include:
• Social Isolation: Difficulties in social communication can lead to feelings of isolation and loneliness.
• Educational Barriers: Many children with ASD require specialized educational plans to address their unique learning needs.
• Employment Difficulties: Adults with ASD may struggle to find and maintain employment due to social and communication challenges.
• Mental Health Issues: Co-occurring conditions such as anxiety, depression, and attention deficit hyperactivity disorder (ADHD) are common in individuals with ASD.
Despite these challenges, many individuals with ASD lead fulfilling lives, particularly when they have access to appropriate support and interventions.
Treatment Strategies for ASD
Management of ASD typically involves a multidisciplinary approach that may include behavioral therapies, educational interventions, speech and language therapy, occupational therapy, and, in some cases, medication. Early intervention is crucial in maximizing the potential for positive outcomes.
• Behavioral Therapies: Applied Behavior Analysis (ABA) is one of the most widely used and evidence-based therapies for ASD. It focuses on improving specific behaviors, such as social skills, communication, and academics.
• Educational Interventions: Individualized Education Programs (IEPs) and specialized teaching strategies can help children with ASD succeed in school.
• Speech and Language Therapy: It helps individuals with ASD improve verbal and non-verbal communication skills.
• Occupational Therapy: Focuses on improving daily living skills and sensory integration.
The Role of Neurofeedback Autism Management
Neurofeedback Autism management is an emerging and promising complementary therapy for ASD. It involves training individuals to regulate their brainwave patterns using real-time feedback from EEG recordings. By promoting healthier brain function, neurofeedback autism management improves symptoms of ASD related to attention, behavior, and emotional regulation in individuals with ASD. Research and clinical practice continues to explore and refine neurofeedback protocols to maximize the effectiveness of neurofeedback autism management.
In summary, ASD is a complex and multifaceted disorder that requires a comprehensive and individualized approach to treatment. As our understanding of ASD grows, so does the potential for innovative therapies like neurofeedback autism management to play a significant role in improving the lives of those affected by this condition.
Brain Changes in Autism
Autism Spectrum Disorder (ASD) is associated with a variety of structural and functional brain changes. Understanding these neurobiological differences is crucial for tailoring neurofeedback protocols to address the specific needs of individuals with ASD. This chapter explores the key brain changes observed in autism and how these alterations impact behavior, cognition, and sensory processing.

Structural Brain Changes in Autism
1. Cortical Thickness and Volume
- Increased Cortical Thickness: Studies have shown that individuals with ASD often have increased cortical thickness in certain brain regions, particularly frontal and temporal lobes. This increase can be associated with difficulties in social communication and executive functioning.
- Altered Brain Volume: There is evidence of both increased and decreased brain volume in different regions. For instance, some individuals with ASD exhibit larger overall brain volumes during early childhood, followed by a normalization or reduction in volume as they age.
2. Amygdala and Hippocampus
- Amygdala: The amygdala, involved in emotion processing and social behavior, is often found to be enlarged in individuals with ASD. This enlargement can correlate with heightened anxiety and difficulties in social interactions.
- Hippocampus: Alterations in the hippocampus, a region critical for memory formation, have been observed, potentially contributing to the cognitive and memory-related challenges seen in autism.
3. Corpus Callosum
- Reduced Size: The corpus callosum, which connects the brain hemispheres, is often smaller in individuals with ASD. This reduction may lead to impaired communication between the hemispheres, affecting coordination and integration of information.
Functional Brain Changes in Autism
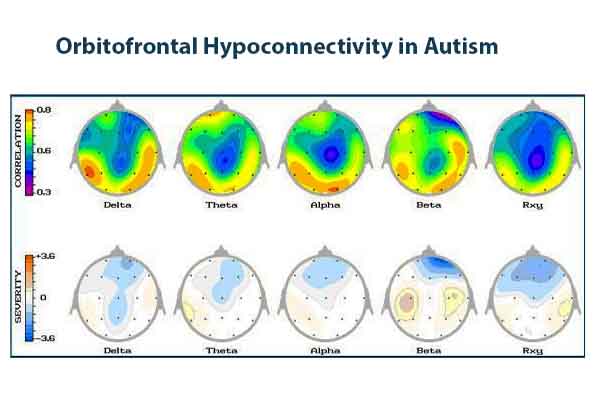
1. Altered Brain Connectivity
- Hypo- and Hyperconnectivity: Individuals with ASD exhibit both hypo- and hyperconnectivity in different brain networks. Hypoconnectivity, or reduced connectivity, is often observed in long-range connections between different brain regions, affecting the integration of sensory and cognitive information. Hyperconnectivity, or increased connectivity, is seen in local, short-range connections, which can lead to repetitive behaviors and focused interests.
2. Impaired Mirror Neuron System
- Social Cognition and Imitation: The mirror neuron system, which is believed to be involved in understanding others’ actions and intentions, is often dysfunctional in individuals with ASD. This impairment may contribute to difficulties in social communication and empathy.
3. Altered Brainwave Activity
- Increased Theta and Delta Waves: Excessive slow-wave activity, such as theta (4-8 Hz) and delta (0.5-4 Hz) waves, is commonly observed in individuals with ASD. These brainwaves are associated with reduced cognitive clarity and attentional deficits.
- Decreased Alpha and Beta Waves: Individuals with ASD often show reduced alpha (8-12 Hz) and beta (12-30 Hz) wave activity, which can lead to difficulties in relaxation, focus, and executive functioning.
Sensory Processing Abnormalities
1. Hyper- and Hyposensitivity
- Sensory Overload: Many individuals with ASD experience heightened sensitivity to sensory stimuli, leading to sensory overload and discomfort. This hyperresponsiveness can affect daily functioning and behavior.
- Reduced Sensitivity: Conversely, some individuals exhibit reduced sensitivity to sensory inputs, which can result in seeking intense sensory experiences or displaying a lack of response to environmental stimuli.
2. Impaired Integration
- Sensory Integration Dysfunction: The ability to integrate sensory information from different modalities is often impaired in ASD. This dysfunction can contribute to challenges in motor coordination, spatial awareness, and adaptive behavior.
Implications for Neurofeedback Protocols. Neurofeedback Autism Management
Individuals with Autism Spectrum Disorder (ASD) often exhibit distinct brainwave patterns compared to neurotypical individuals. These patterns include atypical connectivity and synchronization between different brain regions, as well as deviations in the levels of certain brainwaves such as increased delta and theta waves, decreased alpha waves, and altered beta waves. Such abnormalities can contribute to the sensory processing, social communication, and behavioral challenges seen in ASD. To identify and address these specific brainwave changes, Quantitative Electroencephalography (QEEG) is utilized. QEEG provides a detailed map of the brain’s electrical activity, pinpointing areas with abnormal patterns. Using this data, practitioners can tailor neurofeedback protocols to target these anomalies effectively. One of the most effective protocols involves enhancing alpha waves to promote relaxation and focus, while simultaneously reducing excessive theta and delta waves to improve cognitive function and behavioral control. This personalized approach allows for more precise and effective neurofeedback training, leading to better outcomes for individuals with ASD.
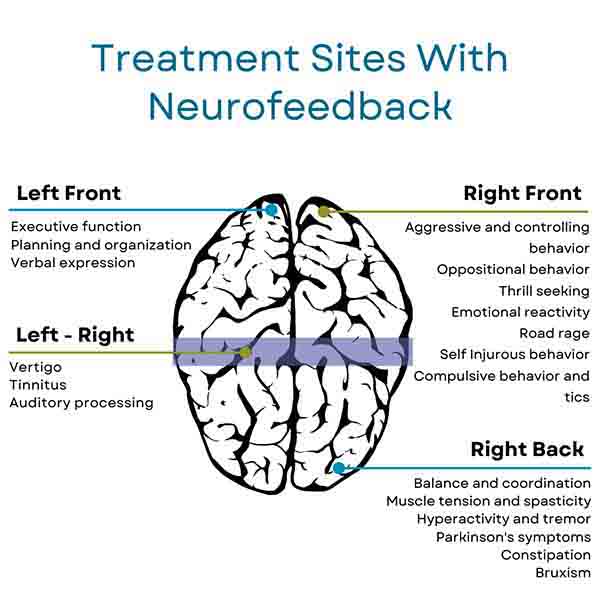
Understanding these brainwave changes is essential for designing effective protocols for neurofeedback autism management for individuals with ASD. For instance:
• Theta/Beta Training: Given the increased theta and decreased beta activity, protocols focusing on reducing theta waves and enhancing beta waves can improve attention and cognitive clarity.
• SMR Training: Enhancing sensorimotor rhythm (SMR) activity can help improve sensory processing and motor control, addressing some of the sensory and behavioral challenges in ASD.
• Alpha/Theta Training: Balancing alpha and theta activity can promote relaxation and emotional regulation, beneficial for individuals with anxiety and emotional dysregulation.
• Delta/Theta Downtraining: Reducing excessive slow-wave activity can enhance cognitive function and reduce brain fog, aiding in better attention and executive functioning.
By targeting these specific brain changes, neurofeedback autism management can provide a personalized approach to improving the symptoms and overall quality of life for individuals with autism.
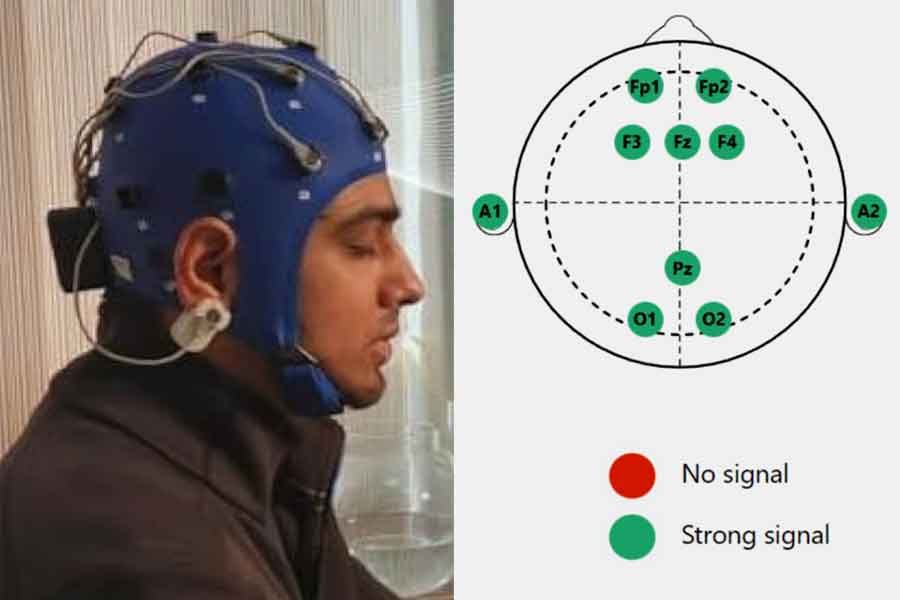
Protocols for Neurofeedback Autism Management
Protocols for Neurofeedback autism management are tailored to address the specific neural dysregulations associated with Autism Spectrum Disorder (ASD). These protocols are designed to improve brain function by training individuals to produce healthier brainwave patterns. Here are some commonly used neurofeedback protocols, along with detailed explanations of their effects and electrode location sites:
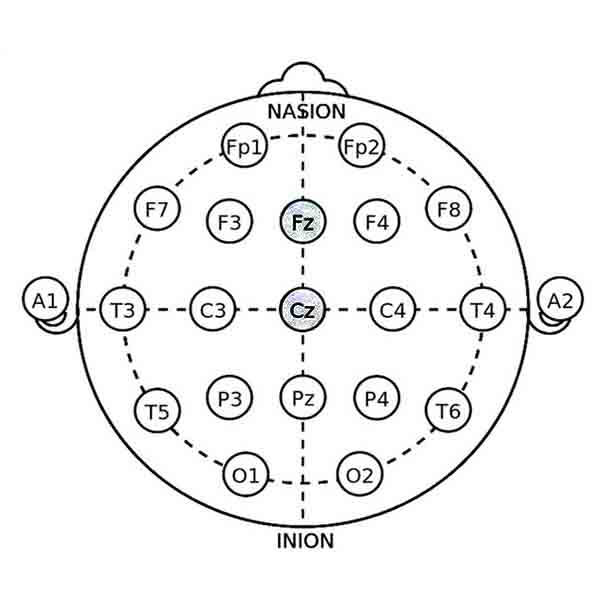
1. Theta/Beta Training for Neurofeedback Autism Management
• Objective: To reduce theta (4-8 Hz) activity and increase beta (12-15 Hz) activity.
• Effect: This protocol aims to enhance attention and cognitive processing while reducing hyperactivity and impulsivity. It is based on the premise that individuals with ASD often exhibit excessive theta waves and insufficient beta waves.
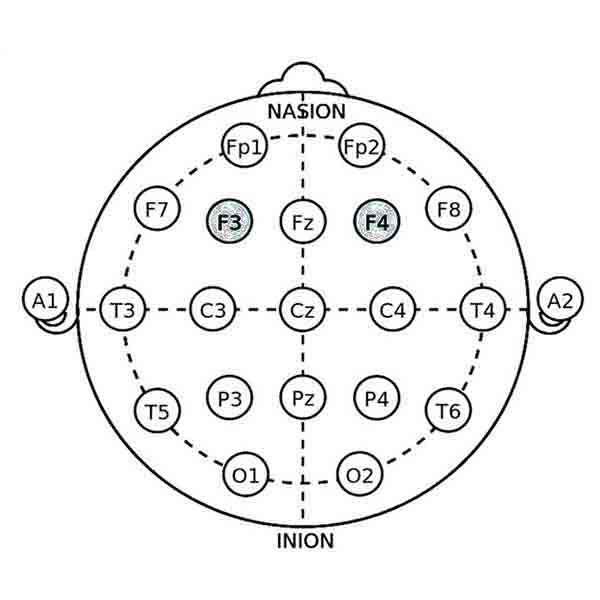
• Electrode Locations: Typically, electrodes are placed at Fz (frontal midline) and Cz (central midline). These sites are chosen to target the prefrontal cortex, which is involved in executive functions and attention regulation.
2. SMR Training
• Objective: SMR training protocol aims to increase sensorimotor rhythm (SMR) activity (12-15 Hz) over the sensorimotor cortex.
• Effect: Enhancing SMR activity is associated with improved sensory processing, motor control, and behavioral regulation. This protocol is particularly beneficial for reducing hyperactivity and improving focus.
• Electrode Locations: Electrodes are placed at C3 (left sensorimotor cortex) and C4 (right sensorimotor cortex), depending on the specific needs of the individual. Bilateral training may also be used to balance activity between the hemispheres.
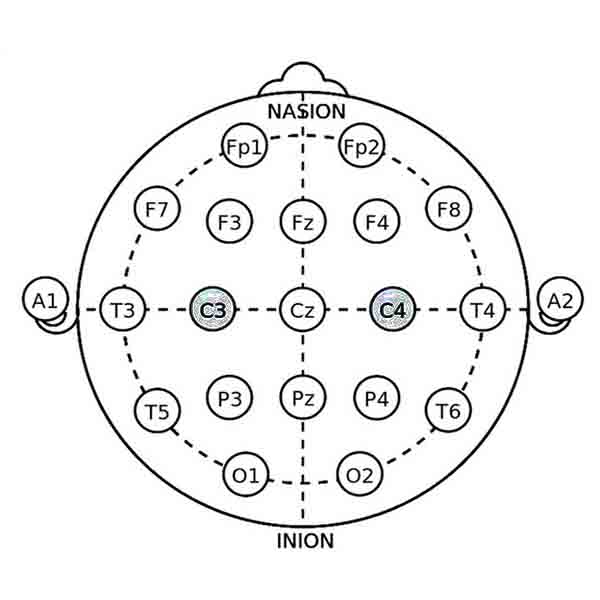
SMR Protocol at C3 (Left Sensorimotor Cortex)
Indications for Use:
- Attention and Focus: Training SMR at the C3 location is often used to improve attention and focus. This is particularly helpful for individuals with ASD who exhibit symptoms of inattention or hyperactivity, as it can enhance the brain’s ability to maintain a calm and focused state.
- Behavioral Control: Individuals with impulsive behaviors and poor behavioral control may benefit from SMR training at C3. Enhancing SMR activity at this site can help regulate these behaviors by promoting better control over motor functions and emotional responses.
- Reducing Hyperactivity: Since C3 is associated with the motor cortex on the left side of the brain, SMR training here can help reduce hyperactivity by calming the motor system and improving overall motor function control.
SMR Protocol at C4 (Right Sensorimotor Cortex)
Indications for Use:
- Anxiety and Emotional Regulation: SMR training at the C4 location is often used to address anxiety and emotional dysregulation. For individuals with ASD who struggle with anxiety or emotional outbursts, enhancing SMR at C4 can help promote a more relaxed and stable emotional state.
- Sensory Processing Issues: Since the right hemisphere of the brain is more involved in processing sensory information, SMR training at C4 can be beneficial for individuals with ASD who have sensory processing difficulties. It can help normalize sensory processing and improve responses to sensory stimuli.
- Improving Sleep Quality: Individuals with ASD often have sleep disturbances. Training SMR at C4 can help improve sleep quality by promoting relaxation and reducing arousal levels, which can lead to more restful and consistent sleep patterns.
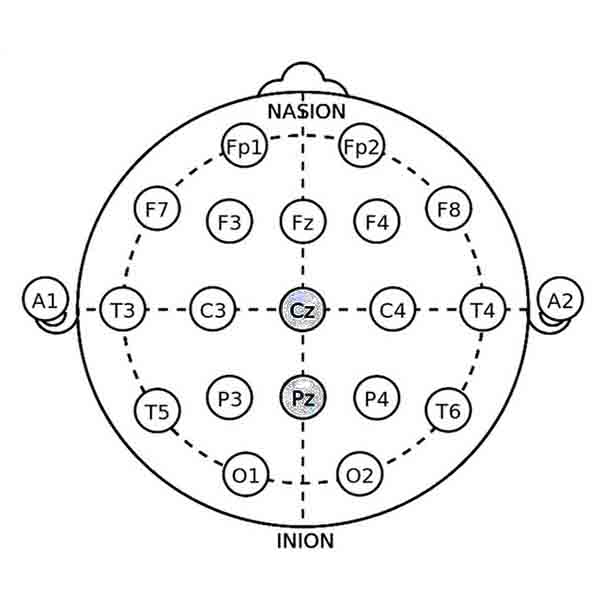
3. Alpha/Theta Training
• Objective: To increase alpha (8-12 Hz) and theta (4-8 Hz) activity while decreasing high beta (20-30 Hz) activity.
• Effect: This protocol promotes relaxation, emotional regulation, and stress reduction. It can help individuals with ASD who experience anxiety and emotional dysregulation.
• Electrode Locations: Electrodes are often placed at Pz (parietal midline) and Cz (central midline). These sites target brain regions involved in relaxation and emotional processing.
4. Delta/Theta Down-training for Neurofeedback Autism Management
• Objective: To reduce excessive delta (0.5-4 Hz) and theta (4-8 Hz) activity.
• Effect: This protocol aims to enhance cognitive clarity and reduce brain fog by decreasing slow-wave activity that is often associated with cognitive and attentional difficulties in ASD.
• Electrode Locations: Electrodes are placed at F3 (left frontal) and F4 (right frontal) to target the frontal lobes, which play a critical role in executive functions and attention.
5. Alpha Peak Frequency Training
• Objective: To adjust the peak frequency of alpha waves to an optimal range (usually around 10 Hz).
• Effect: Optimizing alpha peak frequency can improve cognitive performance, memory, and overall brain efficiency. It is particularly useful for individuals with ASD who exhibit irregular alpha activity.
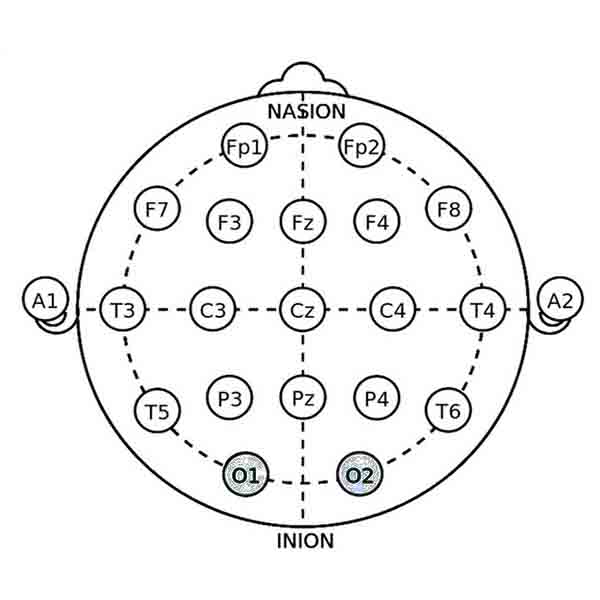
• Electrode Locations: Electrodes are placed at O1 (left occipital) and O2 (right occipital) to target the occipital lobes, which are involved in visual processing and overall brain synchronization.
Neurofeedback Autism Management
Neurofeedback has emerged as a promising tool in the management of Autism Spectrum Disorder (ASD). By training individuals to self-regulate their brainwave activity, neurofeedback autism management aims to improve various cognitive and behavioral functions. This chapter explores the benefits of neurofeedback for individuals with ASD, presents case studies and success stories, and compares neurofeedback with other therapies and treatments.

Benefits of Neurofeedback for Individuals with ASD
1. Improved Attention and Focus
Neurofeedback autism management training can enhance attention and focus by normalizing brainwave patterns associated with attentional deficits. Protocols that reduce theta waves and increase beta waves are particularly effective in addressing issues related to inattention and distractibility.
2. Enhanced Social Skills and Communication
By improving the functioning of neural networks involved in social cognition and communication, neurofeedback can help individuals with ASD better interpret social cues, engage in more meaningful interactions, and improve their verbal and non-verbal communication skills.
3. Reduction in Repetitive Behaviors
Neurofeedback can help reduce the frequency and intensity of repetitive behaviors by balancing brainwave activity and improving self-regulation. This can lead to a more flexible and adaptive behavior pattern.
4. Emotional Regulation and Anxiety Reduction
Neurofeedback protocols that target brain regions involved in emotional processing can help individuals with ASD manage anxiety and emotional dysregulation. This leads to improved emotional stability and a reduction in anxiety-related symptoms.
5. Sensory Processing Improvements
Training aimed at normalizing sensory processing can help individuals with ASD better manage sensory sensitivities and reduce sensory overload. This can significantly improve daily functioning and comfort.
6. Cognitive Enhancements
Neurofeedback autism management training can lead to improvements in executive functions such as planning, organization, and problem-solving. This is achieved by enhancing the connectivity and efficiency of brain networks involved in higher-order cognitive processes.
Symptoms of Autism that can be improved with neurofeedback
The following symptoms can be improved by neurofeedback sessions.
1. Stimming
Repetition of physical movements or sounds is common in ASD patients. Often, this is done because sensory stimuli can become too overwhelming or uncomfortable. Neurofeedback makes the brain function more calmly and efficiently, reducing the patient’s perception of stimuli as being overwhelming. If the patient feels calm overall and the stimuli around them do not seem overwhelming, the stimming can be reduced or eliminated.
2. Emotional outbursts
Neurofeedback improves emotional control within the brain to help the brain function calmly. Emotional outbursts are often due to feeling overwhelmed. Just as stimming results from this, emotional outbursts can also result, as the brain does not know how to cope with the information being provided to it. When the brain functions calmer, the person no longer feels compelled to act out emotionally.
3. Speech issues
Neurofeedback strengthens brain processing, including the areas in the brain that are responsible for taking in sensory information and building a response. Therefore, neurofeedback sessions can improve a person’s ability to engage in conversation and appropriately process what is being said and what should be said in return.
4. Ritualistic behavior
Ritualistic behavior is often performed to deal with anxiety or overwhelming external stimuli, giving the patient a sense of self-control. However, neurofeedback trains the brain to be able to cope with anxiety and external stimuli with more ease, thereby substantially reducing and/or eliminating ritualistic behaviors.
5. Intolerance to change
Neurofeedback trains the brain to process information calmly and appropriately, so when new, even surprising information is presented, the person can cope with the seemingly sudden change without feeling overwhelmed.
6. Hyperactivity
The brain is taught to function more calmly and deal with anxiety more appropriately, thereby reducing symptoms of hyperactivity.
7. Impulsivity
Impulsivity can be significantly reduced and/or eliminated as the brain learns to cope with anxiety in a healthy, sustainable way through neurofeedback.
8. Inability to follow/regard direction from authority figures
Often for those struggling on the autistic spectrum, even processing the information given regarding directions can be overwhelming, so expecting the patient to be able to fulfill these directions seems overwhelming if not impossible. Neurofeedback sessions make the brain function more efficiently and calmly, allowing the patient to improve information processing, which improves the ability to follow the directions given by parents and/or teachers.
9. Anxiety
As one can see after reading the previous eight symptoms, so very many symptoms of ASD are rooted in anxiety. If the brain is overwhelmed by anxiety, processing information can be overwhelming and cause emotional reactions. Once the brain learns to calm itself anxiety can be reduced or eliminated.
10. Issues with social skills
When the brain is working at its best, with far less anxiety and better processing, being social becomes easier.
Case Studies and Success Stories
Numerous case studies and clinical reports have highlighted the positive impact of neurofeedback on individuals with ASD. Here are a few examples:
1. Case Study 1:
Improving Attention and Reducing Hyperactivity
A young boy with ASD and ADHD underwent 40 sessions of neurofeedback focusing on theta/beta training. Post-training assessments showed significant improvements in attention span, reduced hyperactivity, and better classroom performance.
2. Case Study 2:
Enhancing Social Communication
A teenager with ASD received neurofeedback training aimed at increasing SMR activity. After 30 sessions, the individual demonstrated improved eye contact, increased initiation of social interactions, and better verbal communication skills.
3. Case Study 3:
Reducing Anxiety and Emotional Outbursts
An adult with ASD and severe anxiety underwent alpha/theta training for emotional regulation. Following the intervention, there was a marked decrease in anxiety levels, fewer emotional outbursts, and enhanced overall mood stability.
These success stories underline the potential of neurofeedback as a valuable tool in the comprehensive management of autism, offering hope and tangible improvements in various aspects of life for individuals with ASD.
Comparison with Other Therapies and Treatments
1. Behavioral Therapies (e.g., ABA)
Strengths: Applied Behavior Analysis (ABA) is a well-established therapy for ASD, focusing on reinforcing desired behaviors and reducing undesirable ones through structured interventions.
Comparison: While ABA is highly effective in behavior modification, neurofeedback addresses underlying neural dysregulations, potentially leading to more holistic and lasting improvements in brain function and behavior.
2. Pharmacological Interventions
Strengths: Medications can help manage specific symptoms such as anxiety, hyperactivity, and irritability in individuals with ASD.
Comparison: Unlike pharmacological treatments, neurofeedback is non-invasive and free from medication-related side effects. It focuses on self-regulation and brain training, offering a complementary approach that can enhance the effects of medication.
3. Speech and Language Therapy
Strengths: Speech and language therapy is crucial for improving communication skills in individuals with ASD, providing targeted interventions for speech production, language comprehension, and social communication.
Comparison: Neurofeedback can complement speech therapy by addressing brainwave patterns that affect communication abilities, potentially enhancing the outcomes of traditional speech and language interventions.
4. Occupational Therapy
Strengths: Occupational therapy helps individuals with ASD develop daily living skills, improve sensory integration, and enhance motor coordination.
Comparison: Neurofeedback can support occupational therapy by improving sensory processing and overall brain function, leading to better outcomes in motor skills and adaptive behaviors.
5. Social Skills Training
Strengths: Social skills training programs focus on teaching specific social behaviors, improving peer interactions, and enhancing social understanding.
Comparison: By improving neural networks involved in social cognition, neurofeedback can augment the effectiveness of social skills training, leading to more natural and sustained improvements in social behavior.
Table summarizing the effectiveness of neurofeedback and other therapy methods for autism
This table is based on available literature and summarizes the general trends and outcomes associated with each therapy method. The effectiveness of these interventions can vary significantly depending on individual circumstances and the specifics of the implementation.
• Neurofeedback: Studies show significant improvements in attention, social skills, and anxiety reduction, with the effects varying based on individual differences and protocol specifics.
• ABA: Widely regarded as the gold standard for ASD treatment, ABA demonstrates high effectiveness in improving adaptive behaviors and skills, especially when started early and implemented intensively.
• Speech and Language Therapy: Highly effective in improving communication skills, particularly for individuals with speech and language deficits.
• Occupational Therapy: Effective in improving sensory integration and daily living skills, crucial for enhancing independence and quality of life.
• CBT: Moderately effective, particularly for managing co-occurring anxiety and emotional regulation issues.
• Pharmacological Interventions: Effectiveness varies widely depending on the individual and specific symptoms being treated. Often used in combination with other therapies.
• Social Skills Training: Moderately effective, especially when integrated with other therapeutic approaches.
• Music Therapy: This can be beneficial for enhancing social engagement and reducing anxiety, although results can be variable.
• Animal-Assisted Therapy: Shows promise in increasing social interaction and reducing anxiety, though more research is needed to confirm long-term benefits.
• Dietary and Nutritional Interventions: Limited and inconsistent evidence regarding effectiveness; may benefit some individuals but not universally recommended.

• High Effectiveness: 70-100% improvement in targeted symptoms/behaviors
• Moderate Effectiveness: 40-70% improvement in targeted symptoms/behaviors
• Variable Effectiveness: 20-40% improvement in targeted symptoms/behaviors (highly dependent on individual factors and specific implementations)
• Limited Effectiveness: 0-20% improvement in targeted symptoms/behaviors
Conclusion
Neurofeedback offers a promising and innovative approach to managing Autism Spectrum Disorder by addressing the underlying neural dysregulations associated with the condition. Its ability to complement traditional therapies and provide lasting improvements in various cognitive, behavioral, and emotional domains makes it a valuable addition to the comprehensive treatment of ASD. As research and clinical practice continue to advance, neurofeedback is likely to play an increasingly important role in improving the quality of life for individuals with autism.
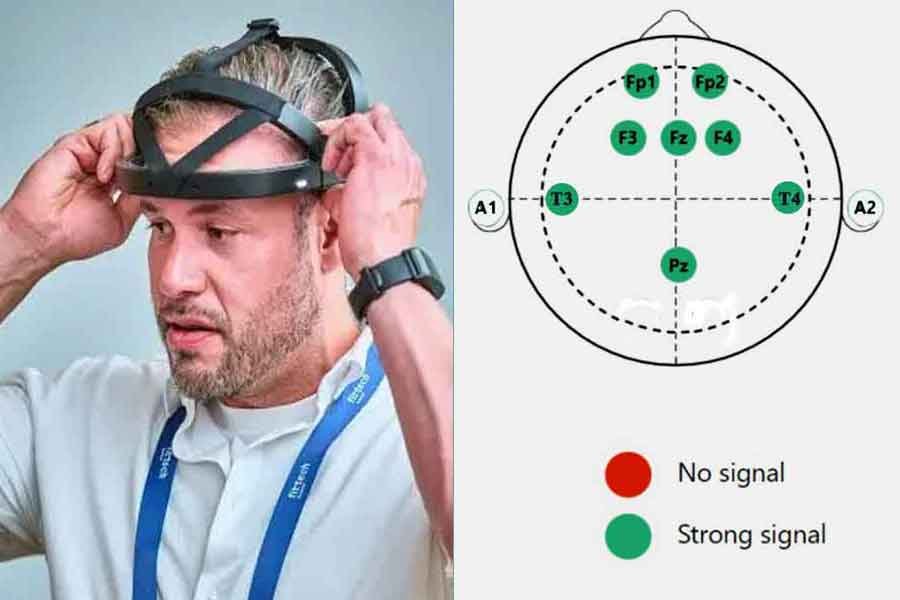
Personal Home-Use Devices for Neurofeedback Autism Management
Personal home-use neurofeedback devices are increasingly becoming popular as a convenient and potentially cost-effective option for managing various conditions, including Autism Spectrum Disorder (ASD). These devices allow individuals to engage in neurofeedback training from the comfort of their own homes, under the guidance of a trained professional or through pre-programmed protocols. This section explores the place of home-use neurofeedback devices, their cost-effectiveness, indications, and contraindications for use.

Role of Personal Home-Use Neurofeedback Devices
1. Convenience and Accessibility
- Ease of Use: Home-use devices are designed to be user-friendly, allowing individuals or their caregivers to easily set up and use the equipment without the need for extensive technical knowledge.
- Accessibility: These devices make neurofeedback accessible to individuals who may not have easy access to professional clinics due to geographic or mobility constraints.
2. Flexibility
- Training Schedule: Users can engage in neurofeedback sessions at times that are convenient for them, without being bound by clinic hours.
- Customization: Many home-use devices offer customizable training protocols that can be tailored to the individual’s specific needs and progress.
3. Support and Guidance
- Professional Oversight: Some home-use neurofeedback systems are used in conjunction with remote monitoring and guidance from trained neurofeedback practitioners, ensuring that the therapy is conducted safely and effectively.
- User Resources: These devices often come with comprehensive user manuals, video tutorials, and customer support to assist users in getting the most out of their training.
Cost-Effectiveness
1. Initial Investment vs. Long-Term Savings
Initial Costs: The upfront cost of purchasing a personal neurofeedback device can be significant, ranging from a few hundred to several thousand dollars, depending on the complexity and features of the device.
Long-Term Savings: Over time, home-use devices can be more cost-effective compared to the cumulative costs of regular in-clinic sessions, especially for long-term therapy needs.
2. Elimination of Travel Costs
No Travel Required: Home-use devices eliminate the need for travel to a clinic, saving time and transportation costs, which can be particularly beneficial for individuals living in remote areas.
3. Family Use
Multiple Users: These devices can often be used by multiple family members, spreading the cost across more than one user and increasing the overall value of the investment.
Indications for Use
1. Mild to Moderate Symptoms of ASD
Behavioral and Cognitive Issues: Home-use neurofeedback devices can be effective for managing mild to moderate symptoms related to attention, behavior, social communication, and sensory processing in individuals with ASD.
2. Complementary Therapy
Supplement to Professional Treatment: These devices can serve as a complementary therapy to professional neurofeedback sessions, allowing for more frequent training and reinforcement of therapeutic gains.
3. Maintenance and General Well-Being
Post-Clinical Therapy: Individuals who have completed a course of professional neurofeedback training may use home devices for maintenance and ongoing support.
Stress and Anxiety Reduction: Home-use devices can also be used to manage general stress and anxiety, which are common co-occurring conditions in individuals with ASD.
Contraindications for Use
1. Severe or Complex Symptoms
Severe ASD Symptoms: Individuals with severe ASD symptoms or those with complex neuropsychiatric conditions may require the supervision and expertise of professional neurofeedback practitioners and should not rely solely on home-use devices.
2. Lack of Professional Supervision
Initial Unsupervised Use: Beginners should avoid using these devices without initial professional guidance to ensure correct use and to tailor protocols to their specific needs.
Complex Protocols: Users who require complex or highly specialized neurofeedback protocols should seek professional supervision to avoid potential misuse or ineffective training.
3. Medical Contraindications
Certain Medical Conditions: Individuals with certain medical conditions, such as epilepsy or severe cardiovascular issues, should use neurofeedback devices only under medical supervision, as brainwave training could potentially trigger adverse effects.
Conclusion
Personal home-use neurofeedback devices offer a convenient, flexible, and potentially cost-effective alternative to traditional in-clinic neurofeedback therapy. They are particularly suited for individuals with mild to moderate symptoms of ASD and can serve as a valuable complementary therapy. However, it is crucial to use these devices under appropriate guidance and to be aware of their limitations, especially for those with severe symptoms or specific medical contraindications. When used correctly, home-use neurofeedback devices can significantly enhance the management of ASD and improve overall quality of life.
List of References
1. American Psychiatric Association. (2013). Diagnostic and Statistical Manual of Mental Disorders (5th ed.). Arlington, VA: American Psychiatric Publishing.
2. Centers for Disease Control and Prevention. (2020). Data and Statistics on Autism Spectrum Disorder.
3. Dawson, G., & Bernier, R. (2013). A Review of Early Intervention in Autism Spectrum Disorders: Evidence, Challenges, and Future Directions. Annual Review of Clinical Psychology, 9, 425-451. doi:10.1146/annurev-clinpsy-032511-143125
4. Ecker, C., Bookheimer, S. Y., & Murphy, D. G. M. (2015). Neuroimaging in Autism Spectrum Disorder: Brain Structure and Function Across the Lifespan. The Lancet Neurology, 14(11), 1121-1134. doi:10.1016/S1474-4422(15)00050-2
5. Fostick, L., & Babkoff, H. (2013). Different Response to Neurofeedback Intervention in ADHD and Asperger’s Syndrome. Clinical EEG and Neuroscience, 44(4), 207-213. doi:10.1177/1550059412451881
6. Kouijzer, M. E. J., de Moor, J. M. H., Gerrits, B. J. L., Buitelaar, J. K., & van Schie, H. T. (2009). Long-Term Effects of Neurofeedback Treatment in Autism. Research in Autism Spectrum Disorders, 3(2), 496-501. doi:10.1016/j.rasd.2008.10.003
7. Loo, S. K., & Barkley, R. A. (2005). Clinical Utility of EEG in Attention Deficit Hyperactivity Disorder: A Research Update. Neurotherapeutics, 2(3), 485-495. doi:10.1602/neurorx.2.3.485
8. Pineda, J. A., Carrasco, K., Datko, M., Pillen, S., & Schalles, M. (2014). Neurofeedback Training Produces Changes in EEG and ERP Measures of Attention and Social Cognition in Autism Spectrum Disorder. Frontiers in Neuroscience, 8, 169. doi:10.3389/fnins.2014.00169
9. Sukhodolsky, D. G., Bloch, M. H., Panza, K. E., & Reichow, B. (2013). Cognitive-Behavioral Therapy for Anxiety in Children with High-Functioning Autism: A Meta-Analysis. Pediatrics, 132(5), e1341-e1350. doi:10.1542/peds.2013-1193
10. Thompson, M., & Thompson, L. (2003). The Neurofeedback Book: An Introduction to Basic Concepts in Applied Psychophysiology. Wheat Ridge, CO: Association for Applied Psychophysiology and Biofeedback.
11. Van Hecke, A. V., Mundy, P. C., Acra, C. F., Block, J. J., et all. (2012). Neural Correlates of Joint Attention in Children with Autism Spectrum Disorder. Brain Research, 1438, 108-119. doi:10.1016/j.brainres.2011.12.019
12. Wang, T., Wang, X., Chen, Y., Sun, L., & Cao, G. (2019). The Efficacy of Neurofeedback for Individuals with Autism Spectrum Disorder: A Meta-Analysis of Randomized Controlled Trials. Neuropsychiatric Disease and Treatment, 15, 1581-1591. doi:10.2147/NDT.S209589
13. Yeo, R. A., Ryman, S. G., Thompson, L. L., & Hutchison, K. E. (2013). Application of Neurofeedback in the Treatment of Autism Spectrum Disorders: Practical and Theoretical Considerations. Journal of Applied Psychophysiology and Biofeedback, 38(3), 135-144. doi:10.1007/s10484-013-9218-4






Add a Comment